Abstract
Aim
Receiving a diagnosis of brain stem death poses significant challenges for families. While much research focuses on organ donation in the context of brain stem death, there is a notable dearth of studies examining the experiences of families themselves. The aim of this review is to explore the experiences of families facing brain stem death.
Design
Systematic review.
Method
A narrative synthesis was conducted, drawing on 11 studies that employed both qualitative and quantitative methodologies. The search encompassed four electronic databases: AHMED (Allied and Complementary Medicine), Emcare (1995-present), MEDLINE (Ovid), and APA PsycInfo (Ovid). Due to the limited research on this topic, no restrictions were placed on the publication dates.
Results
The synthesis revealed five main themes: The Unexpected Prognosis, Coming to Terms with Brain Stem Death—Grieving Process, Observing Brain Stem Death Testing, The Impact of Staff on Families’ Experience, and The Lasting Impact.
Conclusion
The review underscores the pervasive lack of understanding among families regarding the diagnosis and process of brain stem death, as well as the short- and long-term distress it can engender. There is a clear imperative to establish national or international protocols for brain stem death, ensuring more effective and consistent support for affected families.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Despite the first definition of brain stem death (BSD) being identified in 1968 by the Harvard Medical School, there still is not a universally shared concept or recognition accepted. General understanding of BSD is the permanent and total loss of all brain function in the brainstem and cerebrum when oxygen or blood supply to the brain is stopped. BSD differs from a vegetative state or coma as with BSD, mechanical ventilation is required for the patient to breathe and is a permanent state with no possibility of recovery.
1.1 Global differences in BSD practice
As a result of the lack of universal standard of method for BSD diagnosis, the practise surrounding brain death can vary across countries [1, 2]. Prior to testing for BSD, proof is required to confirm that there is irreversible structural brain damage, and that all possibility of a reversible cause of coma can be excluded [3]. Some components of the formal neurological examination and diagnostic criteria that follows are: apnoea testing, absence of corneal reflex, absence of vestibulo-ocular reflex, demonstration of no motor response to pain, no pupillary response to light and no gag reflex tests [4]. These are designed to test the lack of automatic responses, demonstrating permanent damage to the brainstem [5]. Countries will utilize not only different tests, but they also require these tests to be conducted by different professionals with varying expertise [6]. Therefore, the differences in perception and practices surrounding brain death globally are substantial, making the concept of BSD complex for both professionals and patients and their families.
1.2 The current review
Death by neurological criteria (DNC) is often an unexpected, tragic, and difficult experience. Patients who are diagnosed as BSD can still appear to be breathing, retaining their usual colour and body temperature, because of the ventilator oxygenating their bodies. That being so, scepticism or confusion of BSD is understandable.
In the same way diagnostic criteria is not standardised internationally across Intensive Care Units (ICUs), treatment for families going through this difficult situation is not either. Often the language used by clinicians is confusing and hard to follow for families and this inconsistency can lead to further distress [7]. For these reasons, adequate and appropriate care is paramount for the families of those diagnosed as BSD. Given the lack of research regarding families’ experiences of BSD, a review of the current studies is important to analyse and evaluate peoples’ perceptions and experiences of BSD and the care they received to help understand what best practice looks like, what needs to be improved, and what could be developed to ensure support for families.
2 Methods
The review was prospectively registered on PROSPERO (CRD42022332267). Since initial registration the analysis approach and choice of quality bias tool have been altered. Four electronic databases: AHMED (Allied and Complimentary Medicine), Emcare (1995-present), MEDLINE (Ovid) and APA PsycInfo (Ovid) were searched. No limit was placed on date of publishing due to this being a relatively under researched topic.
Search terms were created using the PICO framework (population, intervention, comparison, outcome), resulting in the three concepts: Brain Stem Death, Family and Experience. The following terms were used in our searches: ((brain adj dea*) OR (brain adj stem adj dea*) OR (death adj by adj neurological adj criteria)) AND (family OR families OR (loved adj one*) OR carer* OR partner* OR spouse OR parent* OR guardian* OR sibling* OR brother* OR sister*) AND (experience* OR presence OR attitude* OR acceptance OR opinion* OR perspective*). The original search was conducted on 4th November 2021 and updated on 6th December 2022 and 22nd March 2024 to ensure the inclusion of any new published studies.
Qualitative, quantitative, and mixed methods studies that reported families’ experience of a relatives BSD were included. Studies were included if participants were related to a person with BSD, as a result of blood connection (e.g., sibling, grandmother), marriage (e.g., partner, stepfather) or had any significant relationship with the person with BSD. Studies that were not in English, reviews and individual case reports were excluded.
Title and abstract and full text screening were conducted by ECS and MS. LM independently assessed eligibility of 100% of papers at the full text stage. Any disagreements were resolved with MS. Data for included studies were extracted using a predefined form and identified author(s), year, country, study objective, participants age and relationship to the person with BSD, and families’ experiences of BSD directly (excluding organ donation).
A narrative synthesis was used due to the inclusion of various study designs [9]. Data was translated using thematic analysis using an inductive approach [9]. In this context a process of ‘translation’ of primary themes or concepts reported across studies was used to explore similarities and/or differences between different studies [10]. This provided a means of organising and summarising the findings related to BSD directly from a range of studies and reflect directly, the main ideas and conclusions across studies, rather than developing new knowledge. Thus, the key qualitative and quantitative findings are presented as they are reported in the original paper. The Joanna Briggs Institute Critical Appraisal Tool (JBI) was used to review the potential risk of bias and quality of publication of qualitative, quantitative, and randomised control trial studies (10 item scale and 13 item scale) and the Mixed Methods Appraisal Tool (MMAT) was used to review mixed method studies (7 item scale). Each checklist had criteria to evaluate the most relevant aspects of the specific study design with possible responses of ‘yes’, ‘no’ or ‘unclear’. Risk of bias was determined low if at least 70% of answers were scored ‘yes’, moderate if 50–69% were scored ‘yes’ and high if there were less than 50% scored ‘yes’ for the individual study [11]. Papers were independently assessed by two authors and any disagreements were resolved through discussion or further evaluation with a third author. Overall study quality was not used as an exclusion criterion because we opted to be overly inclusive to gain a sense of the methodological quality of available evidence and provide a comprehensive overview.
3 Results
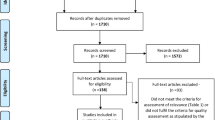
As shown in the PRISMA flow diagram, 11 papers met inclusion criteria for this review (Fig. 1). Across the 11 studies, 987 family members were included. The studies were from Sweden (n = 2), England (n = 2), the USA (n = 2), Canada (n = 1), the Netherlands (n = 1), France (n = 2), and Switzerland (n = 1). Most studies used a qualitative method (n = 7), followed by mixed methods (n = 2) and one Randomised Controlled Trial and one longitudinal study. The key study details and results are shown in Table 1.
PRISMA diagram- Flowchart for study selection and inclusion [8]
3.1 Quality assessment
Four studies were rated as being low quality (i.e., high risk of bias), whilst three studies were rated as being of medium quality and four as high (i.e. low risk of bias). Most qualitative studies failed to consider the influence of the researcher on the research as authors did not locate themselves theoretically and/or culturally and there was not congruence between the research methodology and the methods used to collect data (e.g., using grounded theory but failing to use an iterative process in terms of participant recruitment). Methodological aspects and objective were unclear in the mixed method study by Siminoff [23].
The RCT by Tawil et al. [12] was scored medium because it was unclear whether the treatment groups were similar at baseline and whether the outcome assessors were blind to the treatment allocation. Finally, the mixed methods study by Omrod et al. [13] scored low because the different components of the study were not effectively integrated to answer the research question.
3.2 Narrative synthesis
Results were synthesised based on similarity across the included studies, placed in chronological order and relabelled. This resulted in five overarching themes (Table 2).
3.2.1 The unexpected prognosis
Families experienced a lack of preparedness for BSD [22] and experienced difficulties with the suddenness in which they received news of their family members’ imminent or confirmed BSD diagnosis. Participants described feeling shocked [14, 17], and finding it difficult to understand “Her death was so sudden, so quick. The doctor said, ‘You know your wife is going to die’. I was staggered. In a matter of hours, she went from completely fine to being told that. I was totally gob-smacked. All too sudden. She was such an alive person” [19].
Imagery was used to describe participants first encounter with the BSD prognosis that included an empty room, murder, the collapse of life and descending into hell [15]. ‘Bad news’ was delivered privately or in public waiting rooms, at times by professionals they did not know. This added to the chaos they were experiencing, the disintegration of the life they once knew. There was a feeling of being in another world, or as though the world that was known to the participant is ‘collapsing’ [16].
3.2.2 Coming to terms with brain stem death
This theme was split into 3 stages (denial, bargaining and acceptance) that resemble some stages of Kübler-Ross [23] staged grieving process. Denial, which includes a lack of understanding and unanswered questions, bargaining, in which there is understanding but not believing and having the hope for survival, and acceptance.
3.2.2.1 Denial: partial understanding
Siminoff et al. [20] found, out of the 403 family members informed of the brain stem death diagnosis, only 28.3% could provide an accurate explanation of the diagnosis and 4.5% provided an entirely inaccurate explanation. Although more than half of their participants could identify at least one test to determine BD only 23.1% knew of specific tests used but could not provide any explanation or if they did, they spoke of misconceptions. 1/5 even felt that there had not been any specific tests done to determine the diagnosis of their loved one.
Kesselring et al. [17] found that none of the participants they interviewed could reproduce a ‘scientific’ description of BSD. For many, it was difficult to differentiate between BSD and states like a coma, despite being given verbal explanations and documents.
For some, even witnessing the BSD testing left them with a confused understanding, many did not realise what the tests were supposed to demonstrate, or what they would entail [18]. Ormrod et al. [13] found some similar results, 9/27 family members still had some hope that the tests would demonstrate potential survival, 3/27 remained confused about the status of death after observing the tests, and 2 out of those 3 hoped that even after the ventilation was withdrawn, the BSD patient might still breathe. This might be due to a lack of communication from their relatives’ physicians.
This uncertainty about tests was also cause for additional distress for family members. Participants stated concern that the tests would inflict pain on their relative. Some found the tests quite difficult to watch, especially if the tests were not explained to them throughout. Conversely, if the family had not observed the BSD tests, some of their imagined ideas of those tests could also cause distress.
Sarti et al. [22] reported that the timing and frequency of conversations with families were important for their comprehension. Families needed to be informed early in the death determination process, and to have information repeated several times to understand. Moreover, multimodal communication strategies (e.g., notes, diagrams, images) were critical, helping to ensure that families do not have unanswered questions about the process.
3.2.2.2 Bargaining: understanding but not believing and the hope for survival
An understanding of BSD did not stop the families hope for survival, even if they knew it was not possible. This conflict was often referenced because of the body being warm, and the ventilator still causing the body to breathe and appear alive “We kept on touching her, all the time, she was warm….so she was there. And frankly, when I think about it now, I know that during all that time we believed that she would come back. Even if we knew it wasn’t possible” [16]. In order to feel fully convinced they needed to see the body after the ventilators were turned off [16]. Sarti et al. [22] Also found that families experienced difficulties understanding that their relative could be brain-dead given the fact they appeared as though they were sleeping. The legal time of death appeared to be confusing for many families, particular the distinction between when the person died and when the body died and how this was communicated by the clinicians. Families experienced guilt if they felt their loved one was declared dead in their absence [22].
Others felt that they understood the concept of BSD, but due to not witnessing the BSD tests they did not feel able to accept or believe it. The BSD testing was believed to provide a finality for some that they were unable to have if not allowed to observe [13].
Siminoff et al. [18,19,20] found most families accepted that their family member would not recover either before or immediately after the pronouncement of brain death (78.95%), but 21.1% still felt that their relative may survive and recover. Despite this, over half (60%) of families made statements indicating they believed the patient was still alive after being told their family member was brain dead (n = 241).
3.2.2.3 Acceptance
Acceptance of a situation is to recognize, endure and believe something to be true. The experience of acceptance will exist at different levels and develop over time. For some family members, acceptance occurred once they were able to realise their loved one had passed despite them showing signs of life (breathing, warm skin etc.) [14, 17, 22]. However, they also found that others needed to see the relative once the organ donation operation was complete. In this state, the body would be cold and unmoving, having most likely been in the morgue. This enabled the families to witness their family member in a condition that fit their pre-existing understanding of death, rather than warm and seemingly breathing; “After the operation, I was able to see him once more. I was very happy and seeing him cold was good since you cannot say goodbye when he is still breathing”. For some, observing the BSD testing enabled the family member to have closure as it helped to remove any doubts that death had occurred [13].
Siminoff et al. [20] referred to the concept of acceptance as “Giving Up Hope” which was related to the families’ ethnicity. Non-white family members were less likely to give up hope (58.1%) than white families and more inclined to continue to hope that their family member would recover even after learning the patient was brain dead (41.9%). Furthermore, 63.5% of the families first considered their relative to be dead when the announcement of the brain death diagnosis was given, whereas 21.8% first considered their relative to be dead when the machines had turned off and their heart had stopped. Moreover, they found that those with lower-level education were more likely to agree with the statement that a person is only dead when their heart stops, and that non-white family members were more likely to agree with this statement than the white family members.
3.2.3 Observation of brain stem death testing
3.2.3.1 An inconsistent offer
Ormrod et al. [13] found family members were inconsistently offered the choice to observe brain stem testing. One of the participants who was not offered the choice, requested they see the tests which was granted. All participants included in their study (n = 27) said afterwards that they would have liked to have been able to observe the tests, but only 5 accepted this offer, including the participant who requested. Out of the 8 participants who were offered the opportunity to observe but declined, 1/8 regretted not making the decision and wished that they had.
3.2.3.2 Increasing understanding and acceptance
Tawil et al. [12] conducted a randomized control trial and found that observing the tests led to an increased understanding of BSD. They measured family members understanding of BSD prior to randomizing them into two groups, one of which would allow the family members to be present whilst the BSD tests took place, and the other where they were absent. At a baseline, the group which would be present had a median score of 3/4 and the group who were not going to be present in the BSD tests had a median score of 2.5/4. However, when the groups understanding was measured immediately after the experience, those who were randomized to be present for the BSD tests had increased scores and therefore increased understanding of brain death, whereas those who were randomized to be absent from the tests demonstrated no change in their understanding. Furthermore, 66% of those who were present during the BSD tests achieved perfect post-intervention BSD understanding scores, compared to only 20% who were absent (median 5.0 vs 2.5).
In addition, their study demonstrated that there was a correlation between those with a higher education, who were earning over $25,000, who were younger and those who understood and could describe BSD tests. 36/38 of those who were present during the tests reported that being able to observe them had helped their understanding of BSD. In addition, 32/38 said they would recommend family presence during the tests to others going through the same experience.
In addition, Siminoff et al. [13] found that out of the 14 who had not been offered the opportunity to observe the tests, 5 said they would have liked to in retrospect. All 5 participants who did observe the BSD tests were pleased they had done and reported that it had removed any doubt that their family member had died. For some, seeing the tests only confirmed what they already knew, and was seen as more of a formality.
Sarti et al. [22] found that families were clear that being present for the test was beneficial on three important levels: (1) they clearly understood that their loved one was indeed dead, (2) it was beneficial for their bereavement process in that they had obtained closure in that moment, and (3) they were able to begin grieving without any unanswered questions.
3.2.4 The effect of staff on families’ experience
3.2.4.1 Feeling seen by staff
Encounters with the carers are perceived as important to families, demonstration of empathy and genuine sympathy are key in making the families feel supported and ‘seen’ [14].
Having both the family members and the BSD relative treated with respect and cared for was important for a positive experience. This included communication regarding the BSD, taking initiative to answer any unanswered questions, treating the families loved one with dignity (like being washed) and communication to the loved one at times too [14, 17, 19]; “They saw if we looked questioning at them and they provided information of their own accord. One didn’t need to ask, that I thought was really good.” [14]
3.2.4.2 Feeling neglected by staff
In some papers, staff were reported to have been ‘too busy’ to spend quality time with families to make sure they were ok and understood what was happening [14]. Family members wished they had received more support and guidance from those in the know [19]. Another issue that families confronted was a lack of communication or miscommunication which led to distress, confusion, and unanswered questions [14, 17, 19]; “Nobody said anything to us there—nobody communicated with us. Nobody came out and talked to us during those days—we were told absolutely nothing.” [14]. Conversely families whose medical team took the time to explain BSD testing in advance reported feeling more prepared for the determination and accepting of the result [22].
3.2.5 The lasting impact
3.2.5.1 Experiencing grief
Family members can often still have unanswered questions about BSD, long after the experience is over [14]. Further to this, with the BSD diagnosis happening so quickly, the last image families can have of their family member is of them warm and breathing (due to the ventilator). This can cause people to feel as though they are saying goodbye to their loved one whilst they are still alive [16]. Others did not feel they were able to say goodbye to their family members at all because of the difficult ending as well as not being informed where the patient would be taken to [14].
Moreover, observing BSD testing without a full explanation of their purpose and what they entail can potentially leave families with more distress [13]. Similarly not understanding BSD process was associated with complicated grief symptoms[21].Though, for those who did not observe the BSD testing, not knowing what the procedure included led them to have negative images of what they imagined it to be [13].
Some reported coping by finding meaning in what happened. For example, knowing that if they had survived, they may not have had a good quality of life [14]. However, many families reported wanting further support after their experience in ICU, feeling it would have helped them deal with their grief [14, 16, 19]; “A letter after the event, saying something like, ‘We understand how things are. In the meantime, here is a number.’ You are on your own afterwards. You have got time to think. It would be nice if they would see if you would like to attend a support group or answer questions, to know that you are not on your own. It would be good if they let you know straight away.”[19].
3.2.5.2 Impact on well-being
Tawil et al. [12] and Ormrod et al. [13] measured participant well-being utilizing the Impact of Event Scale (IES) and General Health Questionnaire-12 (GHQ-12). Tawil et al. [12] obtained 41 subjects post measurements (71%): 24 subjects which were randomized to be present for the BSD tests and 17 who were randomized to be absent. The IES and GHQ-12 were similar for both groups. The median IES results for those who were present for the tests was 20.5 and the results of those who were absent were 23.5. Scores exceeding 24 on this test can carry considerable significance, indicating the presence of PTSD symptoms, which is a clinical concern. Individuals with such high scores, even if they do not meet the criteria for full PTSD, may experience partial PTSD or display some symptoms. A score of 23 might suggest the presence of some PTSD symptoms. In addition, the GHQ-12 scores were also similar between the groups. The participants in the group who were present in the tests had a median score of 13 and those who were absent had a median score of 13.6. A score of 11 or 12 is typically considered normal, while scores exceeding 15 may indicate evidence of distress, and scores surpassing 20 are indicative of severe psychological distress. A score of 13 falls close to suggesting the presence of some level of distress.
Ormrod et al. [13] found that the average IES and GHQ-12 scores of the 5 relatives who observed the tests were higher compared to the rest of the participants. These results could suggest that there were higher levels of depression and anxiety in those who observed the tests, though due to the small number of relatives who observed the tests it is difficult to create a meaningful statistical comparison.
4 Discussion
The narrative synthesis highlighted five key common themes across the included studies: The unexpected prognosis, coming to terms with brain death-grieving process, observation of brain stem death testing, impact of staff on families’ experience and the lasting impact.
One of the main findings is that families often do not understand the concept of BSD, what the diagnosis is, and what the implications are. Research suggests that patients only accurately recall around 49% of information communicated to them by healthcare professionals when prompted [24] and that 40–80% of information given by healthcare professionals is often forgotten immediately [25]. This highlights the importance of giving information in multimodal formats as verbal comprehension and recall can be compromised in distress.
A lack of communication and input from staff forces families to have to work out the answers for themselves and considering the wide range of debate surrounding BSD online, time in the ICU with expert professionals presents an opportunity for clarification that families may not receive elsewhere. Research has shown that families in ICU often perceive staff as being busy and unavailable [26], report having to constantly seek out staff to get updated information, being rarely approached by staff to ask if there was anything they needed to know and often not provided with a private space to discuss news with professionals [27]. The findings highlight the importance of staff input on families’ experience and understanding of BSD [22] and need for better family support provision and training for clinical staff.
The review also highlighted the resulting difference between people understanding and accepting BSD. For some, despite understanding the diagnosis and the implications, their hope for their loved one surviving was not waivered. For many, seeing their relatives seemingly alive and breathing gave cause for additional distress and uncertainty. In some instances, observing BSD testing could be helpful in peoples’ movement towards acceptance of death. Many people were pleased to have been present for the testing and to have had the choice and said they would recommend it to future families. With proper communication and explanation from staff, the process was found to provide further explanation of BSD and cement peoples pre-existing understanding. However, without clarification of its purpose and what it would entail, it left some family members further confused. Hodgkinson and liams [28] found that with sudden death of relatives, viewing the body may increase levels of anxiety and distress in the short term, but it lessens the distress for people in the long term. Additionally, Sarti et al. [22] found that being present for BSD testing was beneficial for understanding and closure. Families that were not aware of BSD testing were negatively impacted by additional confusion, stress and grief. Though there is limited research into the effects of observing BSD tests on families’ experience, long term impact, their understanding, acceptance, and grief, nevertheless, these results suggest the importance of integrating the choice for families to observe the tests.
Religion and spirituality are likely to play a role in this experience of holding on to hope vs acceptance. The concept of brain death is less than 100 years old and therefore religions and their many denominations may have various beliefs on whether brain stem death is believed to be ‘death’ [29]. This highlights the importance of involving Chaplaincy or equivalent services in supporting families. Many believe that grief plays a particularly poignant role in the ethical encounter of brain death as it begs the question of what constitutes life and death [30]. We can currently recognise grief through a variety of psychological models. Often, they appear linear as if the journey of grief has an end. However, the Kübler-Ross [23] model looks at 5 stages of grief that one can experience in any order. Kubler-Ross based this understanding on her work within palliative care, the stages include denial, anger, bargaining, depression and acceptance. In many models of grief, the idea of ‘acceptance’ is key.
The allowed time for ‘acceptance’ and understanding of the diagnosis is referred to in BSD literature. In 2014, the Neurocritical Care Society [31] published a toolkit online regarding brain death to help hospitals in the US modernize their policies around the determination of BSD. When considering the communication with family, they refer to a ‘reasonable amount of time’ being allowed for the family to see the relative and come to terms with the diagnosis before the ventilator is removed. This implies that grief can be ‘handled’ by allowing family to spend some time with their family member so that they can come to accept the bereavement.
Some participants described BSD as a ‘suspended death’ [14] describing a discrepancy between what they felt was the time of death and the medicolegal death which they claimed interfered with their grieving process (death anniversaries unknown, for example). Boss identified a new type of loss named ‘Ambiguous Loss’. It occurs when a loved one is physically present but not psychologically, like Dementia. Boss states that because the loved one is here, but seemingly not, grief can be frozen or ‘put on hold’, which leaves people traumatized [32]. It is important to consider the idea of ambiguous loss when thinking about BSD, the family member appearing warm and breathing when told their life is permanently lost.
When considering families well-being scores, [12] found both groups, present and absent for BSD testing, reported their highest IES to be above 26. A moderate or severe impact of trauma requires a score of over 26, with 33 and above being considered as the best representation for a probable PTSD diagnosis. In addition, the group which was present for BSD testing was found to have the highest scores, reaching above 33 (avoidance and intrusion). Furthermore, Ormrod et al. [13] found that observing the tests led to an increase in the likelihood of depression and anxiety. Findings highlight the need for long-term psychological support for families.
5 Strengths and limitations
This review is the first to synthesise families experience of a relative’s brain stem death diagnosis and highlight potential clinical and research opportunities that can better support families. The quality assessment and full text screening was carried out independently by two authors to reduce the level of bias.
It is also important to consider the strengths and limitations of the topic area. The review consisted of 987 participants overall (n = 403 from one study), thus additional research would need to be produced on this topic to ensure a larger sample could be reviewed across a range of settings. In addition, only 3 studies with quantitative data were included and therefore the heterogeneity in study methodology and populations limited a meta-analysis. Furthermore, the quality assessment of the data showed 4/11 studies included had a high risk of bias and low publication quality indicating the need for higher quality research.
The diversity of practice could also be considered a barrier in conducting this review. The wide range of variables including healthcare settings (private, public, understaffed etc.), specific country or state guidelines surrounding BSD, mandatory protocols and tests used to identify BSD are all important variables to consider that will impact a families’ experience which often were not specifically identified within the individual papers themselves.
Moreover, very few studies focused on the cultural impact of both researchers and participants when experiencing BSD, especially given the role of spirituality and religion in the experience of understanding and accepting death. Quality assessment highlighted that cultural or geographical location was not considered when examining peoples experience of BSD, demonstrated through a lack of statement from the authors locating themselves and the lack of demographic information included, with only 2 referencing ethnicities.
6 Implications
6.1 Intensive care unit support protocols
Though countries may differ on their diagnostic criteria for BSD, there is a possibility for a unified perception or method of practice when involving and supporting the families.
Initial care families receive has an impact on grief and that the way families are initially informed of their relatives BSD has a significant impact on their overall understanding. Not only does the explanation of BSD need to be uncomplicated and accessible, but that support is provided throughout each stage and in different formats (verbal and written) so that the explanation can be reiterated to confirm understanding and staff are present for any further questions [33, 34]
Caswell [35] conducted a study of communication between families and staff in end-of-life care. They found that staff could recognise the desire to have more than one conversation with relatives but also acknowledged that they were often reluctant to want to talk about death. Reportedly in most countries, how to speak with patients about death is not included in medical school and allied health professional’s education [36]. Therefore, it is important that professionals have a protocol they can follow to allow for adequate support, consistency in communication and confidence in providing care under these incredibly sensitive circumstances. If meaningful staff involvement is facilitated via implemented care protocols within these settings, family members’ psychological needs can be met, and their grieving process supported.
These protocols could include; private locations in which families can be spoken to regarding the BSD diagnosis and what it entails, psychoeducation, a uniform description that professionals within ICU are familiar with and feel confident in talking through to avoid misinformation or inappropriate language, having an allotted case worker/staff member to whom any questions or concerns can be raised to help the family throughout the process, allowing families time with their relative to give space for acceptance, working with the families to find out what support may be best for them in the future and arranged check-in calls to follow up on any potential mental health support needs and signposting services/resources to support with their grief.
The John Hopkins Hospital, USA created its first Death by Neurological Criteria Team in June 2016. This team’s development means that diagnosis of BSD can happen faster as a result of specific professionals who are experienced in BSD working together to conduct the tests and support the families [37].It is of interest to see the evaluation of such services and how they benefit families.
Given the families’ unique experience of grief, and the apparent confusion and uncertainty surrounding official announcement of BSD, families in this situation require specific grief support to help navigate them throughout this incredibly difficult time. Volpe et al. [38] argued that in order to care for the BSD relatives’ families effectively and manage the inevitable ethical and moral conflicts surrounding the diagnosis, there needs to be further research into new understandings of grief and ways in which that understanding can be incorporated into the communication with these families.
6.2 Trauma-informed support
Kristensen et al. [39] argues that support for those family members who have experienced sudden and violent deaths of loved ones may require different grief support interventions than for loss from natural death. This is because several studies have shown that these sudden bereavements can adversely affect mental health of close ones, with mental health disorders appearing more elevated and with recovery taking longer. Studies also show that peoples initial reactions to the news of sudden death (like denial or guilt for example) can assist professionals in estimating how long or severe the process and progression of grief may be, whether traumatic or pathological [40]. This early identification of traumatic grief can enable appropriate follow up and specific support.
Bolton [41] found that those who grieve after unexpected death are three times more likely to have psychological disorders than those who grieve a natural death. Though the reviewed studies did not explore any potential trauma symptoms associated with the experience of their loved one passing, Tawil et al. [12] demonstrated how this experience could potentially lead to symptoms of PTSD and some participants referenced specific distress surrounding imagery and memories from their hospital experience. For example, though for some witnessing the BSD tests helped with their acceptance of the loved ones diagnosis, some referenced experiencing intrusive memories over a year later and even those who did not witness the tests found the imagined version of them seemingly traumatic,; ‘The most vivid parts of the tests was the cotton wool—I don’t know why but I remember it over and over again.’; ‘I visualise the tests even though I never saw them” [13]. Scott [42] found that social support following a sudden bereavement is associated with reduced depressive and PTSD symptoms. Thus, further research into trauma-informed grief support needs of the family members affected both in the short and long term are needed.
6.3 Cultural Implications
As shown in Siminoff et al. [20] cultural differences can impact the way in which we understand death and are able to accept it. It is important for us to examine the way in which this not only will impact families experience of BSD, but also the way in which professionals may understand it too.
Consequently, additional implications to consider could include providing a safe space for professionals themselves to ask questions. It is important to have a workforce which is knowledgeable and respectful, understanding not only the different beliefs that could exist between their service users, but also within their team, encouraging discussion without judgement to ensure their well-being is also considered. If physicians are well-informed in this way, they can then better manage sensitive discussions with families and reduce confusion [43].
Moreover, working closely with chaplaincy services and religious leaders can increase trust of the medical interventions and help families feel at ease [44].
7 Conclusion
This review highlights the psychological impact of a relative's diagnosis of brain stem death (BSD) on families. Specifically, it underscores the families' persistent lack of understanding of the diagnosis, even months after their relative has passed, and the longer-term psychological distress they endure. It emphasizes the importance of establishing specific BSD protocols to facilitate a consistent approach, improve communication with families, and ensure the pacing and repetition of discussions. Additionally, it stresses the importance of having the confidence to invite families to be present for BSD testing. Further research into ways in which families can be supported throughout this process is essential to mitigate adverse consequences and psychological distress.
Data availability
No datasets were generated or analysed during the current study.
References
Yuan F, Zhang W, Wen W, Li H, Wu S, Wang L. Variability across countries for brain stem death determination in adults. Brain Inj. 2020;37:461–7.
Greer D, Shemie SD, Lewis A, et al. Determination of brain death/death by neurologic criteria: the world brain death project. JAMA. 2020;324(11):1078–97.
Smith M. Brain death: the United kingdom perspective. Semin Neurol. 2015;35(2):145–51.
Dwyer R, Motherway C, Phelan D. Diagnosis of Brain Death in Adults; Guidelines. Intensive Care Society of Ireland, 2016.
Birchwood M, Smith J, Cochrane R. Specific and non-specific effects of educational intervention for families living with schizophrenia. A comparison of three methods. Br J Psychiatry. 1992;160:806–14.
Wijdicks EFM. Brain death worldwide: accepted fact but no global consensus in diagnostic criteria. Neurology. 2002;58(1):20–5.
Youngner SJ, Landefeld CS, Coulton CJ, Juknialis BW, Leary M. “Brain death” and organ retrieval. A cross-sectional survey of knowledge and concepts among health professionals. JAMA. 1989;261(15):2205–10.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PRISMA. 2021;372:71.
Ryan R. Cochrane Consumers and Communication Review Group: data synthesis and analysis. Cochrane Consumers and Communication Review Group. 2013.
Noblit GW, Hare RD. Meta-ethnography: synthesizing qualitative studies. Thousand Oaks: SAGE Publications, Inc; 1988.
The Joanna Briggs Institute. Joanna Briggs Institute reviewers’ manual. 2nd ed. Adelaide: The Joanna Briggs Institute; 2014.
Tawil I, et al. Family presence during brain death evaluation: a randomized controlled trial*. Crit Care Med. 2014;42(4):934–42.
Ormrod JA, et al. Experiences of families when a relative is diagnosed brain stem dead: understanding of death, observation of brain stem death testing and attitudes to organ donation. Anaesthesia. 2005;60(10):1002–8.
Frid I, Bergbom I, Haljamae H. No going back: narratives by close relatives of the braindead patient. Intensive Crit Care Nurs. 2001;17(5):263–78.
Frid I, et al. Brain death: close relatives’ use of imagery as a descriptor of experience. J Adv Nurs. 2007;58(1):63–71.
Kentish-Barnes N, et al. Being convinced and taking responsibility: a qualitative study of family members’ experience of organ donation decision and bereavement after brain death. Crit Care Med. 2019;47(4):526–34.
Kesselring A, Kainz M, Kiss A. Traumatic memories of relatives regarding brain death, request for organ donation and interactions with professionals in the ICU. Am J Transplant. 2007;7(1):211–7.
Kompanje EJ, et al. A national multicenter trial on family presence during brain death determination: the FABRA study. Neurocrit Care. 2012;17(2):301–8.
Lloyd-Williams M, Morton J, Peters S. The end-of-life care experiences of relatives of brain dead intensive care patients. J Pain Symptom Manage. 2009;37(4):659–64.
Siminoff LA, Mercer MB, Arnold R. Families’ understanding of brain death. Progress Transplant. 2003;13:218–24.
Kentish-Barnes N, et al. Grief symptoms in relatives who experienced organ donation requests in the ICU. Am J Respir Crit Care Med. 2018;198(5):751–8.
Sarti AJ, et al. Death determination by neurologic criteria-what do families understand? Can J Anaesth. 2023;70(4):637–50.
Kübler-Ross E. On Death and Dying (1st ed.). Routledge. 1969. https://doi.org/10.4324/9780203010495.
Laws MB, Lee Y, Taubin T, Rogers WH, Wilson IB. Factors associated with patient recall of key information in ambulatory specialty care visits: Results of an innovative methodology. PLoS ONE. 2018. https://doi.org/10.1371/journal.pone.0191940.
Kessels RPC. Patients’ memory for medical information. J R Soc Med. 2003;96(5):219–22.
Dunne K, Sullivan K. Family experiences of palliative care in the acute hospital setting. Int J Palliat Nurs. 2000;6:170–8.
Robinson J, Gott M, Ingleton C. Patient and family experiences of palliative care in hospital: what do we know? An integrative review. Palliat Med. 2014;28:18–33.
Hodgkinson PE, Joseph S, Yule W, Williams R. Viewing human remains following disaster: helpful or harmful? Med Sci Law. 1993;33:197–202.
Chiramel FD, Kalavampara VS, Ali MM, Singh B, Mohamed ZU. The view of major religions of india on brain stem death and organ donation. Amrita J Med. 2020;16(82):6.
Friedrich AB. More than “spending time with the body”: the role of a family’s grief in determinations of brain death. Bioethical Inquiry. 2019;16:489–99.
Brain Death Toolkit. Neurocritical Care Society. 2014. Retrieved June 3, 2022, from https://learn.neurocriticalcare.org/courses/1223.
Boss P. The trauma and complicated grief of ambiguous loss. Pastor Psychol. 2010;59:137–45.
Pearson A, Robertson-Malt S, Walsh K, Fitzgerald M. Intensive care nurses’ experiences of caring for brain dead organ donor patients. J Clin Nurs. 2001;2001(10):132–9.
Reid M. The presence of relatives during brainstem death testing in an intensive care unit. Intensiv Care Soc. 2013;14(4):324.
Caswell G, Pollock K, Harwood R, Porock D. Communication between family carers and health professionals about end-of-life care for older people in the acute hospital setting: a qualitative study. BMC Palliat Care. 2015;1(14):35.
Güven BB, Maden Ö, Satar AD, et al. Factors affecting the emotional reactions of patient relatives who receive news of death: a prospective observational study. BMC Psychol. 2022;10:58.
Nitkin K. The challenges of defining and diagnosing brain death, Johns Hopkins Medicine. Available at: https://www.hopkinsmedicine.org/news/articles/2017/11/the-challenges-of-defining-and-diagnosing-brain-death#:~:text=To%20help%20clinicians%20make%20a,that%20caused%20extensive%20brain%20injury. 2017. Accessed 03 Jun 2021.
Volpe R, Crites JS, Kirschner KL. Temporizing after spinal cord injury. Hastings Cent Rep. 2015;45(2):8–10.
Kristensen P, Weisaeth L, Heir T. Bereavement and mental health after sudden and violent losses: a review. Psychiatry: Interpers Biol Process. 2012;75:75–97.
Simon NM, Wall MM, Keshaviah A, Dryman MT, LeBlanc NJ, Shear MK. Informing the symptom profile of complicated grief. Depress Anxiety. 2011;28(2):118–26.
Bolton JM, Wendy A, Leslie WD, Martens PJ, Enns MW, Roos LL, et al. Parents bereaved by offspring suicide: a population-based longitudinal case-control study. JAMA Psychiat. 2013;70(2):158–67.
Scott HR, Pitman A, Kozhuharova P, Lloyd-Evans B. A systematic review of studies describing the influence of informal social support on psychological wellbeing in people bereaved by sudden or violent causes of death. BMC Psychiatry. 2020;20(1):265.
Lancet T. Religion, organ transplantation, and the definition of death. Lancet. 2011;377(9762):271.
Stahl D, Tomlinson T. Death by neurological criteria: caring for families amid tragedy. Linacre Quart. 2019;86(4):394–403.
Author information
Authors and Affiliations
Contributions
ECS executed the search strategy, carried out the title and abstract screening, carried out the full text screening, extracted the data, carried out the quality assessment and completed the write up LM screened all papers at full text stage, carried out the quality assessment and assisted in final write up MS resolved any discrepancies at screening and quality assessment stages, updated the search and provided feedback on final manuscript and conducted the revisions. SW and MK reviewed the manuscript and contributed to the agreement of themes.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shaikh, M., Cade-Smith, E., Mackay, L. et al. Brain stem death diagnosis: a systematic review of families’ experience. Discov Psychol 4, 73 (2024). https://doi.org/10.1007/s44202-024-00183-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44202-024-00183-w