Abstract
Objective
To evaluate the relationship between the ambulatory arterial stiffness index (AASI) and the degree of coronary stenosis, and assess its predictive value for the presence and severity of coronary artery disease (CAD).
Materials and methods
In total, 619 consecutive patients who presented with exertional anginal symptoms and/or acute coronary syndrome between January 2021 and December 2022 underwent elective non-urgent CAG with no emergency conditions and performed 24-h ambulatory blood pressure monitoring (ABPM) were included in this study and were divided into the control group (n = 68) and CAD group (n = 551) according to the angiography results. Ambulatory Arterial Stiffness Index (AASI) is obtained from the 24-h ABPM recordings, defined as 1 minus the regression slope of diastolic blood pressure on systolic blood pressure values. CAD complexity was determined by the Gensini score (GS). The patients with CAD were stratified according to the tertiles of the Gensini score (GS < 24 versus GS > 48), and GS > 48 is considered severe coronary artery disease. To explore the relationship between AASI and the severity of CAD, Spearman correlation analysis was conducted. Logistic regression analysis was then performed to determine the influence of AASI on CAD as well as severe CAD. Moreover, a Receiver Operating Characteristic (ROC) curve was constructed to assess the predictive value of AASI for CAD and severe CAD.
Results
The CAD group had a substantially higher median AASI than the control group [0.47 (0.4, 0.58) vs.0.32 (0.24, 0.41), P < 0.001]. There was a positive correlation between AASI and Gensini score. Compared to controls, patients in low-, medium-, and high-GS had significantly higher levels of AASI in a rising trend (P < 0.001). Logistic regression demonstrated that AASI was an independent contributor to CAD and severe CAD. The area under the curve (AUC) for AASI in predicting CAD was 0.806 (P < 0.001), and for predicting high-GS CAD was 0.663 (P < 0.001).
Conclusion
AASI was associated with CAD and the severity of coronary stenosis and demonstrated predictive potential for both CAD and severe CAD.
Similar content being viewed by others
1 Introduction
Coronary artery disease (CAD) is a prevalent cardiovascular disorder that arises due to a combination of genetic predisposition and environmental factors. It ranks among the leading causes of mortality worldwide [1]. However, the initial symptoms of CAD frequently exhibit atypical characteristics, which can result in underdiagnosis. Although coronary angiography (CAG) is a reliable method for assessing the severity, location, and extent of coronary artery lesions, its clinical utility is limited due to its complex nature, invasive nature, and associated high costs [2]. In addition, other diagnostic modalities, such as coronary computed tomography angiography, stress echocardiography, or single-photon emission computed tomography, often offer limited information or have drawbacks, including limited availability, high costs, complex protocols, and radiation exposure. Consequently, there is a pressing necessity to explore novel indicators that can effectively identify individuals with CAD, particularly those at high risk.
Ambulatory arterial stiffness index (AASI) is a measure used to evaluate arterial function, assessing arterial elasticity by calculating the variations in systolic blood pressure (SBP) and diastolic blood pressure (DBP) [3]. AASI has been shown to positively correlate with increased cardiovascular mortality and incidence, indicating its predictive value in assessing the occurrence and prognosis of ischaemic cardiovascular disease [4, 5]. It has been observed that AASI is higher in coronary artery disease patients compared to non-coronary artery disease patients [6]. This finding was also observed in the clinical data analysis of patients with combined hypertension and coronary artery disease, particularly in those with essential hypertension and hyperhomocysteinemia [7]. However, to our knowledge, there is conflicting evidence regarding the relationship between AASI and the severity of coronary artery disease [8, 9]. The clinical applicability of AASI remains a subject of debate. Therefore, in this study, we aim to investigate the relationship between AASI and Gensini score, as well as the value in predicting CAD risk and severity.
2 Materials and Methods
2.1 Study Design and Subjects
This retrospective study was conducted in a single center at the second hospital affiliated with Zhengzhou University. 892 patients presented with exertional anginal symptoms and/or acute coronary syndrome between January 2021 and December 2022 underwent elective non-urgent CAG with no emergency conditions and performed 24-h ambulatory blood pressure monitoring. Individuals with previously or recently discovered left ventricular systolic ejection fraction of less than 30%, had atrial fibrillation, pacemaker, valvular heart disease, autoimmune disease, infectious disease, renal failure, hepatic failure, or malignancy were excluded. Finally, 619 patients participated in this study.
The study protocol was approved by the ethics committee of the second affiliated hospital of Zhengzhou University and conformed to the principles of the Declaration of Helsinki. Informed consent was obtained from all participants.
2.2 Anthropometric and Biochemical Measurements
Trained clinicians collected clinical data including patients’ demographics, medical history, and laboratory tests from the medical records.
The patient’s anthropometric measures and biochemical variables were recorded at admission. Body mass index (BMI) was calculated by measuring all patients’ height and weight according to the formula for weight/height2 (kg/m2). All patients were required to fast the previous night before peripheral venous blood samples were collected for fasting blood glucose (FBG), total cholesterol (TC), triglyceride (TG), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), blood lipids, liver and kidney function, and laboratory indicators related to other function using an Olympus AU270 biochemistry analyzer(Olympus, Tokyo, Japan). Type 2 diabetes mellitus (T2DM) was defined as follows: FBG ≥ 7.0 mM, 2-h PBG ≥ 11.1 mM, and/or HbA1c ≥ 6.5% of the subjects who are using glucose-controlling medicines [10]. Hypertension was defined as having an untreated average systolic blood pressure (SBP) of ≥ 140 mm Hg or diastolic blood pressure (DBP) of ≥ 90 mm Hg, based on three measurements taken on at least two separate days. Individuals with SBP/DBP levels below 140/90 mm Hg were still considered to have hypertension if they had a prior diagnosis of hypertension documented and were currently receiving antihypertensive treatment. For ambulatory blood pressure monitoring (ABPM), the thresholds for defining hypertension were as follows: a 24-h average blood pressure (BP) of ≥ 130/80 mm Hg, a daytime average BP of ≥ 135/85 mm Hg, or a nighttime average BP of ≥ 120/70 mm Hg [11].
2.3 24-h ABPM and AASI
Twenty-four-hour ambulatory blood pressure monitoring (ABPM) was conducted using the MGY-ABP1 (MEIGAOYI, Beijing, China), a non-invasive instrument for ambulatory blood pressure measurement. An automated oscillometric cuff was placed on the non-dominant arm. BP readings were taken at 30-min intervals throughout the day and night. A minimum of 80% of the total readings was considered valid for analysis. Additionally, to ensure the reliability of the records, at least 14 measurements during the daytime period or at least 7 measurements during the night or rest period were required.
The ambulatory arterial stiffness index (AASI) is calculated as 1 minus the regression slope of diastolic blood pressure on systolic blood pressure values derived from the 24-h ABPM recordings [12]. AASI was obtained as follows:
Night-time/daytime dip was calculated by the formula, [(mean BP of daytime − night-time)/mean daytime] multiplied by 100. The morning surge was calculated as the difference between the average BP during the 2 h after awakening (four BP readings) and the lowest nighttime BP.
2.4 Coronary Angiography and Assessment of the Severity of Coronary Artery Disease
All participants in the study underwent coronary angiography, and then the degree of coronary narrowing was analyzed by two cardiologists. The diagnosis of coronary artery disease (CAD) required at least 50% stenosis in one of the four main coronary arteries: left main, anterior descending, left circumflex, and right coronary [13]. The Gensini score was calculated by summing the values for the location and luminal narrowing of each lesion. The severity of coronary artery stenosis was categorized into three forms based on the number of affected coronary arteries: single-vessel (n = 155), double-vessel (n = 174), and triple-vessel (n = 222). The Gensini score (GS) was employed to assess the intensity of CAD. The GS assigns points on a scale that corresponds to the degree of coronary artery narrowing: 1 point for < 25% narrowing, 2 points for 26–50% narrowing, 4 points for 51–75% narrowing, 8 points for 76–90% narrowing, 16 points for 91–99% narrowing, and 32 points for total occlusion [14]. Patients with angiographically confirmed CAD were then divided into three groups based on the tertiles of the GS: low GS, < 24 points (n = 178); medium GS, 24–47 points (n = 193); and high GS, > 48 points (n = 180).
2.5 Statistical Analysis
All data were analyzed using IBM SPSS Statistics version 26.0 (Chicago, IL, USA), GraphPad Prism 9.4 (San Diego, California, USA). The Shapiro–Wilk test was used to assess the normality of the continuous variable distribution. Normally distributed data were presented as mean and standard deviation, while non-normally distributed data were presented as median with interquartile range. Categorical variables were described as frequency and percentage (%).
To compare continuous variables with a normal distribution, independent samples t test or analysis of variance (ANOVA) was employed. The Mann–Whitney U test or Kruskal–Wallis test was used for continuous variables with non-normal distribution. Categorical variables were analyzed using the chi-squared test or Fisher’s exact test. The association between Gensini score (GS) and Ambulatory Arterial Stiffness Index (AASI) was assessed using Spearman’s correlation analysis.
Univariate logistic regression analysis was performed to analyze the variables, and variables with a P value < 0.05 in the univariate analysis were included in the multivariate logistic regression analysis. The variance inflation factor (VIF) was calculated to address the potential issue of multicollinearity. Variables with a VIF > 10 were excluded from the analysis to mitigate the impact of multicollinearity.
ROC curves were generated for the combined model, adjusted models, and AASI. The optimal cutoff value was determined based on the maximum Youden index. The area under the curve (AUC) was used to compare the diagnostic utility of CAD presence and a high GS. A P value of less than 0.05 was considered statistically significant.
3 Results
3.1 Baseline Patient Characteristics
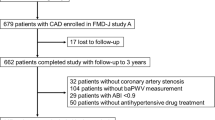
A total of 619 patients were included in this study, with 551 patients belonging to the CAD group (patients with angiographically confirmed CAD) and 68 patients in the control group (patients with normal coronary angiography). The baseline clinical and demographic characteristics of the participants are summarized in Table 1. The specific composition of the patient groups is illustrated in Fig. 1A.
A Subjects: 68 patients without CAD and 551 patients with CAD. The group with CAD was further divided into three subgroups according to Gensini score. Low-score group (n = 178), medium-score group (n = 193), high-score group (n = 180). B AASI levels in CAD group and control group. C Relationship between AASI and the number of coronary artery lesions; *P < 0.05; ****P < 0.0001
The two groups of participants did not differ significantly in terms of gender, smoking, drinking, TG, dsLDL-C, Hb, prealbumin, Average DBP, Average HR, Average MAP, Awake HR, Awake MAP, Nocturnal DBP, Average PP and morning surge.
Meanwhile, the CAD group exhibited a higher prevalence of ST-segment depression. Additionally, the CAD group had higher average age, elevated levels of LDL-C, FBG, HbA1c, Average SBP, Average MAP, Awake SBP, Nocturnal SBP, Nocturnal HR, Nocturnal MAP, Average PP and BMI, as well as lower LVEF, TC, HDL-C, albumin, A/G, and Night-Time Dipping levels (all P < 0.05). Moreover, the CAD group exhibited a significantly higher AASI in comparison to the control group [0.47 (0.4, 0.58) vs. 0.32 (0.24, 0.41), P < 0.001, respectively].
The baseline characteristics of the patients, categorized according to the tertiles of the Gensini score (GS), are presented in Table 2. The table indicates significant differences in various factors including gender, BMI, LVEF, TG, LDL-C, HDL-C, Hb, prealbumin, albumin, A/G, FBG, Nocturnal SBP, Morning surge, Average PP and AASI.
Comparison of AASI between the CAD and control participants.
The CAD group presented a significantly higher AASI compared to the control group [0.47 (0.4, 0.58) vs.0.32 (0.24, 0.41), P < 0.0001, respectively] (Fig. 1B). Subgroup analysis was then conducted in CAD patients based on the number of diseased vessels using the Kruskal–Wallis test, revealing a significant difference among the one-, two-, and three-vessel diseased groups (P < 0.001) (Fig. 1C). Further multiple group comparison was calculated by the Dunn-Bonferroni test. As depicted in Fig. 1C, significantly higher AASI levels were observed in the three-vessel diseased group [median (quartile): 0.524 (0.434–0.612)] and the two-vessel diseased group [0.485 (0.412–0.573)] compared to the one-vessel diseased group [0.409 (0.364–0.475)] (P < 0.0001). And the AASI was higher in the three-vessel diseased group than in the two-vessel diseased group (P = 0.011). The levels of AASI exhibited a progressive increase with a higher number of diseased coronary arteries.
3.2 Association between AASI and Gensini scores
The Gensini score is an angiographic tool utilized to assess the extent and severity of coronary artery disease (CAD). In comparison to the control group, patients in the low, medium, and high Gensini score groups exhibited significantly higher levels of Ambulatory Arterial Stiffness Index (AASI) in an increasing trend (Kruskal–Wallis test, P < 0.001). However, no statistically significant difference was observed among the medium-, and high-GS group followed by Dunn’s multiple comparisons test, possibly due to the limitations of the sample volume (Fig. 2A).
To further elucidate the relationship between AASI levels and the extent of coronary artery lesions, Spearman’s correlation analysis was used to examine the correlations of the AASI with GS in patients with CAD. As shown in Fig. 2B, a significantly positive correlation was established between the two factors (AASI vs. Gensini score, R = 0.375, P < 0.001). Interestingly, the correlation between AASI and Gensini score in low, medium, and high groups did not increase gradually (R = 0.283, P = 0.001; R = 0.024, P = 0.738; R = 0.039, P = 0.605) (Table 3).
3.3 Univariate and Multivariate Analyses of Factors Associated with CAD and Severe CAD
Univariate analysis revealed that several factors were associated with the presence of CAD, including AASI, HDL-C, LDL-C, TG, Albumin, A/G, FBG, HbA1c, Average SBP; Average PP, Night‑Time Dipping, LVEF, ST-segment depression, diabetes mellitus and hypertension. (Table 4).
Multivariate logistic regression analysis demonstrated that AASI, HDL-C and LDL-C remained significant after adjusting for confounders. These associations remained significant (all P < 0.001) even after controlling for gender and age (Model I), or after considering additional characteristics such as gender, age, BMI, smoking status, diabetes, and hypertension (Model II). For each standard deviation increase in AASI, the adjusted odds ratio (95% CI) was 4.04 (2.79, 5.84).
Logistic regression analysis of the severe CAD risk for the high-GS group using low and medium GS groups as the control group showed that, the following factors were associated with the presence of the high-GS group: AASI, HDL-C, LDL-C, Prealbumin, A/G, HbA1c, morning surge, BMI; Average SBP; ST-segment depression; LVEF; gender and hypertension. (Table 5).
Multivariate logistic regression analysis demonstrated that AASI, HDL-C, LDL-C, morning surge, and BMI remained significant after adjusting for confounders. These associations remained significant (all P < 0.001) even after controlling for gender and age (Model I). Furthermore, after adjusting for traditional CAD risk factors including age, sex, hypertension, diabetes mellitus, and smoking, significant differences were still observed (Model II). For each standard deviation increase in AASI, the adjusted odds ratio (95% CI) was 1.73 (1.30, 2.28).
3.4 The Predictive Performance of AASI for CAD and Severe CAD
Figure 3 illustrates the ROC curves of Ambulatory Arterial Stiffness Index (AASI) for predicting the presence of coronary artery disease (CAD) and severe CAD. Comparing AASI with other models based on ROC curves, it was observed that the AUC for Model II was greater. The ROC analysis revealed that the optimal cutoff value for AASI in predicting CAD was 0.423, corresponding to a sensitivity of 68.1% and a specificity of 80.9% (Fig. 3A and Table 6). Moreover, an AASI value of 0.451 was identified as the optimal cutoff point for detecting high Gensini score (GS), with a sensitivity of 54.2% and a specificity of 75.6% (Fig. 3B and Table 7).
4 Discussion
In 2006, Li [15] first proposed the concept of “Ambulatory Arterial Stiffness Index (AASI)”. AASI is an index that was projected as a surrogate measure of arterial stiffness through statistical regression analysis based on 24-h dynamic blood pressure parameters. There was a significant positive correlation with PWV, which is currently recognized as an evaluation of arteriosclerosis (r = 0.51, P < 0.01). The values of AASI range from 0 to 1, with values closer to 0 indicating better arterial elasticity and values closer to 1 indicating poorer arterial function. The principle of AASI is mainly related to the compliance of blood vessels, which can be determined by the elasticity of the vessel wall. When risk factors such as hypertension, hyperlipidemia, and smoking act on the blood vessels, arterial elasticity decreases and vascular compliance decreases. This decrease in compliance leads to a faster wave reflection, causing the reflected wave to appear earlier at the end of the systolic phase of the arterial pressure wave, increasing systolic blood pressure, while at the same time, during the diastolic phase, due to the loss of synergy of the reflected wave that should have appeared during the diastolic phase, the pressure decay increases, which leads to a decrease in diastolic blood pressure. Thus, the functional relationship between systolic and diastolic blood pressure can reflect the degree of arterial sclerosis, and AASI is based on this principle [16]. AASI has been found to have application value in the fields of hypertension, cerebrovascular disease, and coronary artery disease. In studies examining the correlation between AASI and hypertension, researchers have found associations with blood pressure variability, target organ damage in hypertension, and assessment of antihypertensive medication efficacy [17,18,19]. In the field of cerebrovascular disease, significant results have also been obtained, such as a positive correlation between AASI and the incidence of acute ischemic stroke [20], as well as a significant correlation with the cerebral vascular function score (a novel indicator for assessing cerebral embolism) [21] However, there is no statistically significant correlation between AASI and the incidence of acute intracerebral hemorrhage. Nevertheless, there is limited and controversial research regarding the predictive value of AASI for coronary artery disease and its assessment of coronary artery lesions [6, 7, 9]. The main focus of this study is to explore the correlation between AASI and Gensini score in patients with suspected coronary artery disease and their predictive value for coronary artery disease and severe coronary artery disease.
In this study, the AASI of coronary artery disease (CAD) patients was significantly higher than that of the control group without coronary artery lesions. Moreover, there was a statistically significant increasing trend in AASI across the low, moderate, and high Gensini score groups. A positive correlation was observed between AASI and Gensini score, which was evident in the CAD group. However, this correlation was not observed within different Gensini score subgroups, possibly due to a small sample size and further subdivision of the groups. Additionally, the calculation of the GS considered only two factors: the severity score and the regional multiplying factor for each lesion. However, it did not take into account the additional third parameter, which is the effect of the severity score adjustment factor on collateral modification [22]. As a result, the complexity of measuring CAD with GS is overestimated in patients with total collateral coronary artery occlusion. Therefore, in CAD patients, AASI may reflect the extent of coronary artery lesions, and monitoring AASI could provide a non-invasive and convenient method for predicting coronary artery disease. Additionally, in this study, coronary artery disease patients had higher age, BMI, LDL-C, FBG, and HbA1c levels compared to non-coronary artery disease patients. The proportion of hypertensive and diabetic patients was also higher in the coronary artery disease group, which is consistent with previous research findings [23, 24]. The demographic characteristics of our study population are similar to those in previous studies, which enhances the generalizability of our research results.
In the multivariate analysis, multiple influencing or confounding factors were comprehensively considered. Further analysis revealed that AASI was an independent predictor for the presence of coronary artery disease (CAD) and high Gensini score. Additionally, apart from the well-established CAD predictors such as HDL-C, LDL-C, and BMI, we identified independent predictors for high Gensini score (morning surge). The morning surge were found to be associated with the severity of coronary artery lesions [25, 26]. However, despite the strong correlation between AASI and Average PP, the univariate analysis did not reveal a significant association between Average PP and the presence of CAD and in the high-GS group. These results may be potentially influenced by the limitations imposed by the sample size. Subsequent ROC curve analysis showed that the area under the ROC curve for AASI in predicting coronary artery disease was 0.806 (95% CI 0.751–0.861, P < 0.001), and for predicting high Gensini score was 0.663 (95% CI 0.615–0.712, P < 0.001) (Table 7). This suggests that AASI has a certain predictive value for coronary artery disease and severe coronary artery disease, and when combined with other independent risk factors and traditional coronary artery disease risk factors in our study, the predictive ability of the model was further enhanced. Therefore, AASI can be considered as a novel predictive reference index for CAD, providing evidence for the prediction, screening, and assessment of the severity of coronary artery lesions.
Coronary angiography has long been used as the gold standard for diagnosing coronary artery disease, but its application has been limited by the high price of the measurement equipment and the high professionalism required of the operators. AASI is derived from 24 h-ABPM, and ambulatory blood pressure monitoring is a straightforward and easily executed procedure, and studies have confirmed that there is a positive correlation between AASI and Pulse Wave Velocity (PWV), and that AASI can be used to assess arteriosclerosis. AASI as a test indicator is non-invasive, and has the advantage of being convenient, economical and reliable, and can be accepted by a broader spectrum of patients, and its advantages provide a new choice for the diagnosis of coronary artery disease. Ambulatory blood pressure monitoring, a non-invasive blood pressure measurement method, bears no absolute contraindications and is predominantly employed for hypertension monitoring and diagnosis. And the findings of this study suggest that AASI holds predictive value in diagnosing patients presenting with suspected symptoms of angina, especially those with high GS confirmed after coronary angiography.
Therefore, in clinical practice, 24-h ambulatory blood pressure monitoring can be used to screen patients with asymptomatic and suspected coronary heart disease, especially those patients who refuse coronary angiography due to economic time and other reasons, but this does not mean that these patients do not need to undergo coronary angiography. It is difficult to obtain AASI through continuous and accurate blood pressure monitoring in clinical practice, which makes this index prone to fluctuations, and may be poor in stability and repeatability. In addition, there is not enough evidence to show that coronary arteries change before AASI is slightly elevated, and more in-depth basic research is needed in order to obtain accurate evidence in this regard.
This study has several limitations that should be acknowledged. Firstly, it is a small-sample cross-sectional study conducted at a single center, which may introduce bias and limit the generalizability of the findings. The small sample size reduces the statistical power and may affect the reliability of the results. Secondly, the exclusion of patients with severe coronary artery disease, such as those with heart failure or previous revascularization therapy, may underestimate the predictive efficacy of AASI for coronary artery disease. Including these patients in future studies would provide a more comprehensive understanding of AASI’s predictive value. Therefore, further research with larger sample sizes, multicenter collaborations, and comprehensive analysis of influencing factors is needed to provide a solid theoretical basis for the prediction of coronary artery disease and severe coronary artery disease using AASI.
5 Conclusions
In conclusion, the findings of this study indicate that AASI is increased in patients with coronary artery disease and shows a positive correlation with the severity of coronary artery lesions. AASI is identified as a valuable predictor for the presence and severity of CAD. Therefore, our study suggests that incorporating AASI into the assessment of patients with suspected coronary artery disease can help identify individuals who are more likely to have severe and significant CAD, thereby potentially reducing the need for invasive coronary angiography. Thus, these findings suggested that the AASI exerted a predictive potential for both CAD and severe CAD. It serves as a simple, inexpensive, and timely predictor for both conditions.
Availability of Data and Materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- AASI:
-
Ambulatory arterial stiffness index
- CAD:
-
Coronary artery disease
- GS:
-
Gensini score
- ABPM:
-
Ambulatory blood pressure monitoring
- ROC:
-
Receiver operating characteristic
- CAG:
-
Coronary angiography
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- BMI:
-
Body mass index
- LVEF:
-
Left ventricular ejection fraction
- STD:
-
ST-segment depression
- HTN:
-
Hypertension
- DM:
-
Diabetes mellitus
- TC:
-
Total cholesterol l
- TG:
-
Triglyceride
- LDL-C:
-
Low-density lipoprotein-cholesterol
- HDL-C:
-
High-density lipoprotein-cholesterol
- sdLDL-C:
-
Small dense low-density lipoprotein cholesterol
- Hct:
-
Hematocrit
- Hb:
-
Hemoglobin
- A/G:
-
Albumin/globulin ratio
- Dbil:
-
Direct bilirubin
- Ibil:
-
Indirect bilirubin
- FBG:
-
Fasting blood glucose
- HbA1c:
-
Hemoglobin A1c
- Fib:
-
Fibrinogen
- IMA:
-
Ischemia-modified albumin
- HR:
-
Heart rate
- MAP:
-
Mean blood pressure
- PP:
-
Pulse pressure
References
Butnariu LI, Florea L, Badescu MC, Țarcă E, Costache I-I, Gorduza EV. Etiologic puzzle of coronary artery disease: how important is genetic component? Life Basel Switz. 2022;12:865.
Ngam PI, Ong CC, Chai P, Wong SS, Liang CR, Teo LLS. Computed tomography coronary angiography - past, present and future. Singapore Med J. 2020;61:109–15.
Kikuya M, Asayama K, Ohkubo T. Blood pressure variability and arterial stiffness parameters derived from ambulatory blood pressure monitoring. Kardiol Pol. 2019;77:509–14.
Bastos JM, Bertoquini S, Polónia J. Prognostic significance of ambulatory arterial stiffness index in hypertensives followed for 8.2 years: its relation with new events and cardiovascular risk estimation. Rev Port Cardiol Orgao Of Soc Port Cardiol Port J Cardiol Off J Port Soc Cardiol. 2010;29:1287–303.
Boos CJ, Thiri-Toon L, Steadman CD, Khambekar S, Jordan A, Carpenter JP. The relationship between ambulatory arterial stiffness index and cardiovascular outcomes in women. Cardiol Res. 2021;12:161–8.
Yan X-P, Peng J-T. Correlation analysis between ambulatory arterial stiffness index and coronary atherosclerosis in patients with coronary heart disease. J Clin Cardiol (China). 2010;9:654–6.
Dong L, Liu J, Qin Y, Yang W-J, Nie L, Liu H-N, et al. Relationship between ambulatory arterial stiffness index and the severity of angiographic atherosclerosis in patients with H-type hypertension and coronary artery disease. Clin Exp Hypertens N Y N. 1993;2023(45):2228517.
Boos CJ, Toon L-T, Almahdi H. The relationship between ambulatory arterial stiffness, inflammation, blood pressure dipping and cardiovascular outcomes. BMC Cardiovasc Disord. 2021;21:139.
Di Raimondo D, Casuccio A, Di Liberti R, Musiari G, Zappulla V, D’Angelo A, et al. Ambulatory arterial stiffness index (AASI) is unable to estimate arterial stiffness of hypertensive subjects: role of nocturnal dipping of blood pressure. Curr Hypertens Rev. 2017;13:121–31.
American Diabetes Association Professional Practice Committee. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2022. Diabetes Care. 2022;45:S17–38.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertens Dallas Tex. 1979;2018(71):e13–115.
Dolan E, Li Y, Thijs L, McCormack P, Staessen JA, O’Brien E, et al. Ambulatory arterial stiffness index: rationale and methodology. Blood Press Monit. 2006;11:103–5.
Saraste A, Knuuti J. ESC 2019 guidelines for the diagnosis and management of chronic coronary syndromes: Recommendations for cardiovascular imaging. Herz. 2020;45:409–20.
Gensini GG. A more meaningful scoring system for determining the severity of coronary heart disease. Am J Cardiol. 1983;51:606.
Li Y, Wang J-G, Dolan E, Gao P-J, Guo H-F, Nawrot T, et al. Ambulatory arterial stiffness index derived from 24-hour ambulatory blood pressure monitoring. Hypertens Dallas Tex. 1979;2006(47):359–64.
Stergiou GS, Kollias A, Rarra VC, Nasothimiou EG, Roussias LG. Arterial stiffness index based on home (HASI) vs. ambulatory (AASI) blood pressure measurements. Hypertens Res Off J Jpn Soc Hypertens. 2010;33:731–6.
Gómez-Marcos MA, Recio-Rodríguez JI, Patino-Alonso MC, Gómez-Sánchez L, Agudo-Conde C, Gómez-Sánchez M, et al. Ambulatory arterial stiffness indices and target organ damage in hypertension. BMC Cardiovasc Disord. 2012;12:1.
Bahrainwala J, Patel A, Diaz KM, Veerabhadrappa P, Cohen DL, Cucchiara A, et al. Ambulatory arterial stiffness index and circadian blood pressure variability. J Am Soc Hypertens JASH. 2015;9:705–10.
Jin Y, Thijs L, Richart T, Li Y, Dolan E, Wang J-G, et al. Responses of the ambulatory arterial stiffness index and other measures of arterial function to antihypertensive drugs. Hypertens Res Off J Jpn Soc Hypertens. 2011;34:489–95.
Hoshide S, Tomitani N, Kario K. Maximum ambulatory daytime blood pressure and risk of stroke in individuals with higher ambulatory arterial stiffness index: the JAMP study. Hypertens Res Off J Jpn Soc Hypertens. 2023;46:84–90.
Yue Y, He J-T, Chen Y, Deng C, Jia S-Y, Li B. The correlation between cerebrovascular function scores and ambulatory blood pressure parameters in patients with primary hypertension. China Prev Med. 2019;20:118–23.
Rampidis GP, Benetos G, Benz DC, Giannopoulos AA, Buechel RR. A guide for Gensini Score calculation. Atherosclerosis. 2019;287:181–3.
Zamorano JL, García-Moll X, Ferrari R, Greenlaw N. Demographic and clinical characteristics of patients with stable coronary artery disease: results from the CLARIFY registry in Spain. Rev Espanola Cardiol Engl Ed. 2014;67:538–44.
Boyer NM, Laskey WK, Cox M, Hernandez AF, Peterson ED, Bhatt DL, et al. Trends in clinical, demographic, and biochemical characteristics of patients with acute myocardial infarction from 2003 to 2008: a report from the american heart association get with the guidelines coronary artery disease program. J Am Heart Assoc. 2012;1: e001206.
Harbalıoğlu H, Kaypaklı O. Morning blood pressure surge is associated with the severity of stable coronary artery disease in hypertensive patients. Clin Exp Hypertens N Y N. 1993;2021(43):334–40.
Gao X-Y, Zhou B-Y, Zhang M-Z, Zhao X, Qing P, Zhu C-G, et al. Association between fibrinogen level and the severity of coronary stenosis in 418 male patients with myocardial infarction younger than 35 years old. Oncotarget. 2017;8:81361–8.
Acknowledgements
The authors thank for Dr. Liu Shichao and Dr. Li Zheng for assistance in data retrieval at our hospital and to Dr. Li Zheng for his assistance in patient follow-up.
Funding
The study was supported by Henan Provincial Science and Technology Research Project (Project Number: LHGJ20210382).
Author information
Authors and Affiliations
Contributions
JLG conceived and supervised the study; QXT and YQG: designed experiments; QXT, YQG, ZYD, JP, JXT and YZ: contributed to data collection and manuscript editing; QXT and YQG: analyzed data; QXT: wrote the manuscript; QXT and YQG: made manuscript revisions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Ethics Approval and Consent to Participate
The study protocol was approved by the ethics committee of the second affiliated hospital of Zhengzhou University and conformed to the principles of the Declaration of Helsinki. Informed consent was obtained from all participants. Consent for publication.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Qin, X., Yin, Q., Zhang, Y. et al. Ambulatory Arterial Stiffness Index is Associated with the Presence and Severity of Coronary Artery Disease. Artery Res (2024). https://doi.org/10.1007/s44200-023-00043-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44200-023-00043-3