Abstract
Endotheliopathy plays a role in the development of acute kidney and lung injury in COVID-19, probably due to inflammation, endothelial permeability, vascular leakage and edema formation. This study examined alterations in the circulation of patients with mild and severe COVID-19 on in vitro endothelial permeability and its relation to the endothelial angiopoietin/Tie2 system, which is involved in the regulation of endothelial permeability. Plasma was obtained from COVID-19 patients admitted to the ward (n = 14) or ICU (n = 20) at admission and after 1 and 2 weeks and healthy controls (n = 5). Human kidney and lung endothelial cells were exposed to patient plasma and treated with recombinant angiopoietin-1. In vitro endothelial barrier function was assessed using electric cell-substrate impedance sensing. Circulating markers of the angiopoietin/Tie2 system, endothelial dysfunction and glycocalyx degradation were measured by ELISA. Plasma from COVID-19 patients reduced endothelial resistance compared to healthy controls, but COVID-19 plasma-induced drop in endothelial resistance did not differ between ward and ICU patients. Circulating angiopoietin-2, soluble Tie2 and soluble Tie1 levels increased over time in ICU patients, whereas levels remained stable in ward patients. The increase in angiopoietin-2 was able to predict 90-day mortality (AUC = 0.914, p < 0.001). Treatment with recombinant angiopoietin-1 did not restore COVID-19 plasma-induced hyperpermeability. In conclusion, these results suggest that indirect effects of the virus represented in the circulation of COVID-19 patients induced endothelial hyperpermeability irrespective of disease severity and changes in the endothelial angiopoietin/Tie2 system. Nonetheless, angiopoietin-2 might be of interest in the context of organ injury and patient outcome in COVID-19.
Similar content being viewed by others
1 Introduction
Endotheliopathy plays a role in the pathophysiology of Coronavirus disease 2019 (COVID-19) [1]. Common complications of COVID-19 are acute kidney injury (AKI) and acute respiratory distress syndrome (ARDS) and incidence in hospitalized patients is reported to be 33 and 20%, respectively [2,3,4]. Severe acute respiratory distress syndrome coronavirus 2 (SARS-CoV-2), the virus responsible for COVID-19, induces an inflammatory response and combined with a direct effect of the virus on endothelial cells can lead to endothelial dysfunction [5]. Accumulating evidence indicates that SARS-CoV-2 has adverse effects on the endothelium, such as endothelial inflammation, endothelial hyperpermeability, promoting a pro-coagulative state and leukocyte infiltration [6]. Consequently, endothelial dysfunction is considered to contribute to the development of AKI and ARDS [2, 4, 7, 8].
The SARS-CoV-2 virus enters cells via the binding of its spike glycoprotein to angiotensin-converting enzyme 2 (ACE2) [9]. ACE2 is not only very abundant in the lungs, but is also expressed by endothelial cells making it possible for the virus to alter endothelial function directly [10,11,12]. It is shown that the virus is present in the cell membrane of pulmonary [13] and renal endothelial cells [11] in patients who died from COVID-19. However, knowledge on the additional indirect pathophysiological effects of the virus on endothelial cells in COVID-19 patients is still sparse.
Most of our understanding concerning endothelial dysfunction in COVID-19 patients is derived from the evaluation of circulating markers involved in endothelial activation, permeability and injury [6, 14, 15]. Recently, it is shown that plasma from COVID-19 patients induced in vitro endothelial hyperpermeability compared to plasma from healthy controls [16], suggesting that the SARS-CoV-2 virus alters the plasma fingerprint from COVID-19 patients. It is, however, unknown whether these alterations are dependent of disease severity and what might cause these alterations in endothelial permeability.
Barrier function of the endothelial monolayer is regulated by cell–cell and cell–matrix adhesion and different types of junctional complexes keeping endothelial cells together. An important regulator of endothelial barrier function is the endothelial angiopoietin/Tie2 system [17]. The tyrosine kinase receptor Tie2 is primarily expressed by and located on endothelial cells. The activity of Tie2 is regulated by its ligands, angiopoietin-1 and -2. During quiescence, angiopoietin-1 is released from pericytes and functions as a Tie2 agonist. Angiopoietin-1 can phosphorylate and thereby activate Tie2, leading to a well-maintained endothelial barrier. Angiopoietin-2 is a context-dependent antagonist or partial agonist of Tie2. During pathological conditions, angiopoietin-2 is highly released from the Weibel-Palade bodies and antagonistically binds to the Tie2 receptor thus preventing phosphorylation. Consequently, downstream Tie2 signaling is deactivated and cell–cell junctions are weakened, thereby inducing endothelial hyperpermeability and vascular leakage [17, 18]. Disturbances in the endothelial angiopoietin/Tie2 system might therefore contribute to organ injury during critical illness. [18, 19]
In COVID-19 patients, increased levels of angiopoietin-2 have been linked to disease severity and are suggested to predict ICU admission and mortality [20,21,22]. Additionally, we have previously shown that increased circulating levels of angiopoietin-2 are associated with plasma-induced endothelial hyperpermeability in other critically ill patients [23]. Moreover, higher levels of angiopoietin-2 are reported in patients who developed AKI after cardiac surgery compared to patients who did not develop AKI [24]. In ARDS patients, increased angiopoietin-2 levels were associated with increased mortality risk [25]. Interestingly, we have previously shown that pharmacologically targeting the endothelial angiopoietin/Tie2 system reduced vascular leakage and improved microcirculatory perfusion in animal models of critical illness [26, 27]. This suggests the involvement of angiopoietin-2/Tie2 in the development of AKI and ARDS in COVID-19.
Hence, the aim of this study was to examine the effect of changes in the circulation of COVID-19 patients with mild and severe symptomatology on renal and pulmonary in vitro endothelial permeability. In addition, we assessed changes in endothelial permeability over time and whether in vitro endothelial barrier function is related to alterations in the endothelial angiopoietin/Tie2 system.
2 Materials and Methods
2.1 Patient Samples
Plasma samples from adult patients with confirmed SARS-CoV-2 infection by PCR were collected in the Amsterdam UMC COVID Biobank. The Amsterdam UMC COVID Biobank contains plasma samples from a large prospective cohort of all confirmed COVID-19 patients admitted to the Amsterdam UMC. The institutional review board and the biobank ethics committee of the Amsterdam UMC approved the biobank study protocol (protocol number 2020_182).
The present study cohort included 34 consecutive patients who were diagnosed with COVID-19 between March 2020 and May 2020. They were divided into two groups: patients with mild symptoms who were hospitalized in medical conventional wards (n = 14) and patients with severe symptoms who were admitted to the ICU (n = 20). Patients admitted to the ICU were depending on invasive mechanical ventilation and intensive monitoring and were therefore classified as severely ill. Plasma from 5 healthy volunteers was included as control.
Patients at the ICU were sampled at admission and, during week 1 and week 2 of ICU admission, whereas patients at the ward were only sampled at admission and during week 1 (Fig. 1). Blood was collected in citrate tubes and immediately centrifuged at 4.000G for 10 min at 4 °C. Plasma supernatant was centrifuged for another 5 min at 12.000G at 4 °C to obtain platelet-free plasma and stored at − 80 °C.
Study design Patients were sampled three times during hospital admission; at admission, during week 1 and week 2*. Blood samples were centrifuged and plasma samples were stored at − 80 °C. In the current study, ECIS and ELISA were performed with the obtained plasma samples. *only if patients were not discharged before week 2
2.2 Study Definitions
Patient demographics and clinical outcome parameters were obtained from electronic medical records. ARDS was assessed according to the Berlin criteria [28]. AKI was defined as an absolute increase in serum creatinine of ≥ 26.5 µmol/L within 48 h, an increase in serum creatinine of ≥ 50% compared to baseline, or urine output of < 0.5 mL/kg/h for > 6 h based on the 2012 Kidney Disease Improving Global Outcomes (KDIGO) Clinical Practice Guideline [29]. Mortality was defined as 90-day mortality either in-hospital or after discharge.
2.3 Renal Endothelial Cells
Human primary kidney glomerular endothelial cells were obtained from Cell Biologics (H-6014G, Cell Biologics Company, Chicago, United States). Cells were cultured on gelatin-coated T25 flasks in complete medium in an atmosphere of 95% air and 5% CO2 at 37 °C.
Complete medium consisted of basal medium H1168 supplemented with endothelial cell medium supplemental kit (1168-Kit, Cell Biologics Company, Chicago, United States) containing fetal bovine serum, endothelial cell supplement, l-glutamine, antibiotic and antimycotic supplement, hydrocortisone, fibroblast growth factor, epidermal growth factor, heparin and vascular endothelial growth factor.
2.4 Pulmonary Endothelial Cells
Human pulmonary microvascular endothelial cells were obtained from Lonza (HMVEC-L, CC-2527, Lonza Group, Basel, Switzerland). Cells were cultured on gelatin-coated T25 flasks in complete medium in an atmosphere of 95% air and 5% CO2 at 37 °C. Complete medium for pulmonary endothelial cells (EGMTM-2 MV, Lonza Group, Basel, Switzerland) consisted of basal endothelial cell medium supplemented with fetal bovine serum, ascorbic acid, antibiotic and antimycotic supplement, hydrocortisone, fibroblast growth factor, epidermal growth factor, insulin-like growth factor, vascular endothelial growth factor.
2.5 Electric-Cell Substrate Impedance Sensing
Electric cell-substrate impedance sensing (ECIS; Applied BioPhysics, Troy, NY, USA) was used to measure resistance of endothelial cells as previously described [23, 30,31,32]. Passage five and six human endothelial cells were transferred to gelatin-coated 96-wells ECIS culture plates (Applied BioPhysics, Troy, NY, United States) pre-treated with 10 mM L-cysteine (Merck, Darmstadt, Germany) and gelatin. The ECIS device was used for continuous, single frequency scanning to confirm a confluent monolayer. After reaching a steady state in impedance, which indicates that a confluent monolayer has been formed, cells were washed with and exposed to 1% human serum albumin (HSA) in bare medium for 60 min followed by addition of 10% platelet-free plasma collected from COVID-19 patients. HSA (1%) was used as time control. All patient plasma samples were measured individually (one patient plasma sample per well). Impedance of the endothelial monolayer was measured at 4000 Hz using ECIS software (210.0 PC; Applied Bio-Physics) until a steady-state was reached (approximately 1 h). Measurements were performed in triplicate and normalized to baseline. Impedance measurements were used to derive resistance of the cells which represents the barrier function of the endothelial cells [30].
2.6 Recombinant Angiopoietin-1
To study the effect of activation of the endothelial Tie2 receptor on plasma-induced alterations in endothelial barrier function, recombinant angiopoietin-1 was added. In a separate experiment, renal and pulmonary endothelial cells were exposed to plasma from ICU (n = 9) and ward (n = 9) COVID-19 patients as described above. After 15 min, recombinant angiopoietin-1 (800 ng/mL; 923-AN, R&D systems, Biotechne, Minneapolis, MN, USA) was added and resistance of endothelial cells was measured with the ECIS as described above. Measurements were performed in duplicate and normalized to baseline.
2.7 Plasma Analysis
Plasma concentrations of several markers of the endothelial angiopoietin/Tie2 system, endothelial injury and glycocalyx degradation were measured using commercially available enzyme-linked immunosorbent assays (ELISA) according to the manufacturer. The following markers were measured in all individual patient plasma samples obtained at admission, week 1, and week 2: angiopoietin-1 (DANG1, R&D systems), angiopoietin-2 (DANG2, R&D systems), soluble Tie1 (DY5907, R&D systems, Biotechne, Minneapolis, MN, USA), soluble Tie2 (DTE200, R&D Systems, Biotechne, Minneapolis, MN, USA)), soluble thrombomodulin (ab46508, Abcam, Cambridge, MA), von Willebrand Factor (vWF) (ab108918, Abcam, Cambridge, MA), and heparan sulfate (SEA565Hu, Cloud-Clone Corp). Delta levels were defined as the difference between the circulating levels at week 1 compared to admission.
2.8 Statistical Analysis
A difference of 12% in in vitro endothelial resistance between mild and severely ill COVID-19 patients was expected. With a significance level (α) of 0.05 and beta of 0.9, group sizes of n = 8 were calculated. To associate circulating angiopoietin-2 levels with in vitro endothelial resistance, a group size of n = 20 was calculated [23, 31].
Data were analyzed using GraphPad Prism 8.2 (GraphPad Software, San Diego, CA, USA) and IBM SPSS statistical software, version 22.0 (IBM Software Group, New York, NY, USA). Continuous data are presented as mean ± standard deviation for normally distributed data, or median with interquartile range for non-parametric data. Normality of the data was checked via histograms and Shapiro–Wilk tests. Changes in endothelial resistance over time in the ICU cohort were calculated using Friedman test with Bonferroni post-hoc analysis, since data were not normally distributed. In patients at the ward, differences in endothelial resistance between admission and week 1 were tested using a Wilcoxon signed-rank test.
Associations between patient outcome and circulating markers and between patient outcome and in vitro endothelial resistance were analyzed using the non-parametric Mann–Whitney U test. Associations with binary outcome data were checked using logistic regression. A receiver operating characteristic (ROC) curve was plotted to test the accuracy of delta angiopoietin-2 as a predictor. Correlations between in vitro endothelial markers and circulating markers were analyzed using a Spearman’s rank correlation test. A p-value < 0.05 was considered as statistically significant.
3 Results
3.1 Patient Characteristics
Patients demographics and clinical parameters are listed in Table 1. Most patients were male (ward 57.1%; ICU 70.0%) and the mean age of ward patients was 65 ± 13 years and 62 ± 10 years of patients at the ICU. The two patient groups were comparable in terms of BMI, smoking behaviour, and the prevalence of hypertension. However, patients at the ICU had a higher incidence of diabetes mellitus type 2 compared to patients admitted to the conventional ward (14.3% vs 50%, p = 0.035).
During admission, 11 out of 20 patients at the ICU developed AKI (55%) and all 20 ICU patients developed ARDS (100%). None of the patients at the ward developed AKI or ARDS nor were transferred to the ICU during our sampling period. Furthermore, ICU patients had an increased length of hospital stay compared to ward patients (p < 0.001). During our sample period, none of the ICU patients were transferred to the ward. Lastly, 90-day mortality was 55% in the ICU cohort.
3.2 Plasma from COVID-19 Patients Induced In Vitro Endothelial Hyperpermeability
Plasma from COVID-19 patients obtained at admission reduced renal and pulmonary endothelial resistance compared to plasma from healthy controls (Fig. 2A, B). Interestingly, renal and pulmonary endothelial resistance did not differ between patients with mild and severe symptomatology at admission (Fig. 2).
COVID-19 plasma-induced endothelial hyperpermeability Human pulmonary (A) and renal (B) endothelial cells were exposed to plasma from COVID-19 patients collected at admission and healthy controls and endothelial resistance was measured over time. Human serum albumin was used as time control. Data represent mean and were tested with a two-way ANOVA with repeated measurements. ** = p < 0.01, *** = p < 0.001
Interestingly, there were differences in endothelial resistance exposed to plasma collected at different time points. The reduction in in vitro pulmonary endothelial resistance was less following exposure with plasma obtained from severely ill patients at the ICU at week 1 and 2 (0.38 [0.37–0.42] vs 0.40 [0.37–0.49] vs 0.72 [0.46–0.93]; p < 0.001; Fig. 3A) and from mildly ill patients at the ward at week 1 (0.37 [0.34–0.38] vs 0.40 [0.37–0.46]; p < 0.01; Fig. 3A).
Changes in endothelial resistance over time Human pulmonary (A) and renal (B) endothelial cells were exposed to plasma from COVID-19 patients collected at admission, week 1 and week 2 at the ward or intensive care and endothelial resistance was measured. Data represent median with interquartile range and were tested with Friedman test with Bonferroni post-hoc analysis and Wilcoxon signed rank test. * = p < 0.05, ** = p < 0.01, *** = p < 0.001
When using plasma samples obtained from patients at the ICU at week 1 and 2, the decrease in in vitro renal endothelial resistance was smaller compared to plasma obtained at admission. (0.46 [0.43–0.52] vs 0.50 [0.44–0.58] vs 0.77 [0.56–0.86]; p < 0.001; Fig. 3B) and from mildly ill patients at the ward at week 1 (0.45 [0.44–0.50] vs 0.50 [0.45–0.69]; p = 0.039; Fig. 3B).
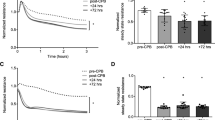
3.3 Treatment with Recombinant Angiopoietin-1
Addition of recombinant angiopoietin-1 did not alter COVID-19 induced reduction in pulmonary and renal endothelial resistance compared to solely plasma from mild and severe COVID-19 patients (Fig. 4)
Endothelial barrier function with recombinant angiopoietin-1 Human pulmonary (A) and renal (B) endothelial cells were exposed to plasma from mild (ward; grey lines) and severe (ICU; black lines) COVID-19 patients collected at admission and treated with recombinant angiopoietin-1 (rAng1; dotted lines). Data represent mean
3.4 Circulating Markers of the Endothelial Angiopoietin/Tie2 System
Patients admitted to the ward showed higher circulating levels of angiopoietin-2, angiopoietin-2/1 ratio, and soluble Tie2 at admission when compared to patients admitted to the ICU (p = 0.015, p = 0.048 and p = 0.025, respectively). Interestingly, patients admitted to the ICU showed an increase in circulating levels of angiopoietin-2 (Fig. 5A), the soluble form of the Tie2 receptor (Fig. 5E) and soluble Tie1 (Fig. 5F) in the first week following admission. Circulating angiopoietin-1 and the angiopoietin-2/1 ratio remained stable over time (Fig. 5C, D). On the contrary, this increase was absent in patients at the ward since circulating levels of angiopoietin-2, angiopoietin-1, soluble Tie2 and soluble Tie1 remained unchanged (Fig. 5A, C, F). Circulating levels of soluble thrombomodulin, von Willebrand Factor, and heparan sulfate, markers of endothelial injury and glycocalyx degradation, showed no changes over time in both patient groups (Additional file 1).
Levels of circulating markers of the angiopoietin/Tie2 system Changes in circulating markers over time in patients diagnosed with COVID-19 admitted to the ICU and ward. Circulating levels of angiopoietin-2 (A), delta angiopoietin-2 (B), angiopoietin-1 (C), angiopoietin-2/1 ratio (D), soluble Tie2 (E) and soluble Tie1 (F) at admission, week 1, and week 2. Data represent median with interquartile range and were tested using Friedman test with Bonferroni post-hoc analysis and Wilcoxon signed rank test. * = p < 0.05, ** = p < 0.01, *** = p < 0.001
No correlations were found between in vitro renal endothelial resistance and circulating markers of the angiopoietin/Tie2 system at admission (Additional file 2). Moreover, correlations were also lacking between circulating markers and pulmonary endothelial resistance (Additional file 3).
3.5 Alterations in the Angiopoietin/Tie2 System and Patient Outcome
The increase in angiopoietin-2 within the first week of admission was associated with an increased likelihood of developing AKI (OR 1.6, 95% CI 1.1–2.4, p = 0.013), developing ARDS (OR 2.1, 95% CI 1.1–3.8, p = 0.017) and 90-day mortality (OR 2.3, 95% CI 1.3–4.0, p = 0.006) in our total study cohort including all 34 COVID-19 patients. Furthermore, an increase in soluble Tie2 and soluble Tie1 between admission and week 1 increased likelihood of developing ARDS (OR 1.6, 95% CI 1.1–2.6, p = 0.028 and OR 1.8, 95% CI 1.0–3.4, p = 0.047 respectively). Delta soluble Tie2 and delta soluble Tie1 were not associated with increased odds of developing AKI and 90-day mortality.
Receiver operating characteristic (ROC) curves with area under the curve (AUC) analysis was generated to determine the prognostic accuracy of the increase in angiopoietin-2 levels for 90-day mortality in our patient group. Delta angiopoietin-2 showed good discrimination for 90-day mortality (AUC = 0.914, 95% CI = 0.807–1.000, p < 0.001) as shown in Fig. 6.
4 Discussion
In the present study, we examined the effect of changes in the circulation of COVID-19 patients with mild and severe symptomatology on renal and pulmonary in vitro endothelial permeability. In addition, we assessed changes in endothelial permeability over time and whether in vitro endothelial barrier function is related to alterations in the endothelial angiopoietin/Tie2 system.
We showed that COVID-19 patient plasma-induced renal and pulmonary endothelial hyperpermeability as measured with an in vitro bioassay. This COVID-19 plasma-induced endothelial hyperpermeability occurred irrespective of disease severity. Interestingly, plasma-induced endothelial hyperpermeability was less severe after one week of hospital and ICU admission. The endothelial angiopoietin/Tie2 system, which is involved in regulation of endothelial permeability, was dysbalanced as represented by increased circulating angiopoietin-2 and soluble Tie2 levels over time in severely ill patients, but not in mildly ill patients. Both circulating angiopoietin-2 and soluble Tie2 levels were not associated with in vitro endothelial permeability. Moreover, treatment with recombinant angiopoietin-1 did not restore COVID-19 plasma-induced endothelial hyperpermeability. However, the increase in circulating angiopoietin-2 was associated with the development of AKI and ARDS and was able to predict 90-day mortality. These results suggest that the indirect effects of the SARS-CoV-2 virus, as represented by changes in the circulation, results in endothelial hyperpermeability independent of disease severity and alterations in the endothelial angiopoietin/Tie2 system. Nonetheless, circulating angiopoietin-2 might be of interest in the context of organ injury and patient outcome in COVID-19.
ECIS is an in vitro technique to quantify real-time behaviour of cells within a monolayer [30]. An important aspect of endothelial physiology is the formation and maintenance of the endothelial barrier. ECIS measures changes in impedance as endothelial cells form a monolayer and establish tight junctions between cells. In case of a disruption of the endothelial barrier, a decrease in impedance is detected. Endothelial hyperpermeability is increasingly recognized in the pathophysiology of COVID-19. However, this parameter is clinically limited to the evaluation of fluid overload as a consequence of vascular leakage or by the evaluation of circulating markers involved in the regulation of endothelial barrier function. In the present study, we showed that COVID-19 patient plasma-induced in vitro renal and pulmonary endothelial hyperpermeability was not different between mildly and severely ill COVID-19 patients. These results are in agreement with those obtained by Michalick and colleagues [16]. In addition, these results are also in alignment with findings previously reported by our group in critically ill patients in which plasma from patients following hemorrhagic shock and cardiac surgery impaired endothelial barrier function compared to plasma from healthy controls or preoperative plasma measurements [23, 31, 32].
It is, however, unexpected that disease severity would not affect plasma-induced endothelial hyperpermeability as earlier research suggested a relationship with disease severity in COVID-19 patients [6, 8]. The absence of an effect of disease severity might be explained by the fact that our study examines indirect effects of the virus on endothelial cells. In the current in vitro setting, impaired vascular tone, dysregulation of coagulation and complement activation factors that have been proven to be involved in COVID-19 pathophysiology, were not taken into account. Moreover, although not the focus of our research and therefore not fully studied, circulating markers related to glycocalyx degradation and endothelial injury did not differ between mildly and severely ill patients at admission. Also, time till hospital or ICU admission since COVID-19 infection was comparable between mild and severely ill patients. Taken together, COVID-19 plasma-induced in vitro renal and pulmonary endothelial hyperpermeability was independent of disease severity and improved over time.
Knowledge of the pathophysiological mechanism leading to endothelial hyperpermeability in patients with COVID-19 is scarce. In severely ill COVID-19 patients, increased circulating levels of angiopoietin-2 are reported [1, 14, 20, 21, 33] and reduced gene expression of the endothelial Tie2 receptor was found in renal post-mortem biopsies [34]. Unexpectedly, we found higher circulating levels of angiopoietin-2 in ward patients compared to ICU patients at admission. This finding is contrary to previous studies which have reported a positive relation between disease severity and circulating angiopoietin-2 levels [1, 14, 20, 21, 33]. This result may be explained by the fact that we were unfortunately not able to correct for hematocrit in our patient cohort since no data were available at admission. On the other hand, we have increased circulating angiopoietin-2 and soluble Tie2 levels, which is indicative for increased shedding of the Tie2 receptor, in severely ill COVID-19 patients. This increase was absent in COVID-19 patients with mild symptoms. This suggests that endothelial the angiopoietin/Tie2 system is more dysregulated in severely ill COVID-19 patients compared to COVID-19 patients with mild symptoms.
Although we previously have shown that increased angiopoietin-2 levels were associated with plasma-induced endothelial hyperpermeability from patients undergoing cardiac surgery with cardiopulmonary bypass [23], we did not find this relation using plasma from COVID-19 patients in the current study. Moreover, this relation was also not found using plasma from traumatic hemorrhagic shock patients [31]. The absence of this direct relation is supported by the finding that angiopoietin-2 itself could not induce in vitro endothelial hyperpermeability or vascular leakage in mice, but seems to need an additional barrier disruptive agent such as thrombin or a cytokine [35, 36]. In addition, treatment with recombinant angiopoietin-1 did not restore COVID-19 plasma-induced endothelial hyperpermeability. It was previous shown that exposing endothelial cells to plasma from severe ill COVID-19 patients did not affect Tie2 gene expression [37], which might explain the lack of treatment with recombinant angiopoietin-1 on endothelial permeability. However, within the same study the authors showed that stimulation of Tie2 attenuated COVID-19 plasma-induced alterations in thromboinflammatory gene expression and procoagulant activity [37]. An important methodological difference is that they have pretreated the cells with recombinant angiopoietin-1, while we have treated the cells after exposure to patient plasma which is from a clinical perspective a more relevant moment. To summarize, the endothelial angiopoietin/Tie2 system is dysregulated in critically ill COVID-19 patients, however, this is not directly associated with in vitro plasma-induced endothelial hyperpermeability.
An increase in circulating angiopoietin-2 over time was associated with AKI and ARDS development in our total cohort. This finding supports the role of angiopoietin-2 in organ injury in critically ill patients. However, caution must be applied, as this study is not able to show causality between an increase in angiopoietin-2 and the development of ARDS and AKI. Additionally, delta angiopoietin-2 was able to predict 90-day mortality in our total cohort. This is in line with the results from Villa et al. stating that the three-day angiopoietin-2 course is a strong predictor of in-hospital mortality [22]. Although these results should be interpreted with caution due to the low sample size, angiopoietin-2 seems to be of considerable importance in the clinical course of patients with COVID-19 and worth further investigation. Taken together, these results indicate that circulating angiopoietin-2 is not directly related to in vitro endothelial hyperpermeability, however, the increase of angiopoietin-2 over time might be used as a marker for adverse outcome in COVID-19 patients.
4.1 Limitations
We acknowledge several limitations of the present study. First, clinical outcome parameters such as the development of AKI and ARDS and mortality were not our primary outcome. The predictive value of angiopoietin-2 might, therefore, be underpowered. Nonetheless, we found significant associations despite the small sample size making it an interesting marker in COVID-19 patients for future research. Secondly, relatively ‘healthy’ endothelial cells were used to study the effect of plasma in an in vitro setting. Many hospitalized COVID-19 patients, especially at the ICU, present with comorbidities including hypertension, diabetes, and cardiovascular diseases often accompanied by vascular dysfunction [38, 39]. However, the representability of this in vitro model for endothelial barrier function has been confirmed in previous studies [23, 30,31,32].
5 Conclusions
In conclusion, we report that COVID-19 patient plasma induced renal and pulmonary endothelial hyperpermeability irrespective of disease severity. Interestingly, plasma-induced endothelial hyperpermeability improved over time. The endothelial angiopoietin/Tie2 system was dysbalanced in severely ill, but not mildly ill, patients, however, were not associated with in vitro endothelial permeability. Moreover, treatment with recombinant angiopoietin-1 did not restore COVID-19 plasma-induced endothelial hyperpermeability. The increase in circulating angiopoietin-2 was associated with the development of AKI and ARDS and able to predict 90-day mortality. These results suggest that the indirect effects of the SARS-CoV-2 virus, as represented by changes in the circulation, results in endothelial hyperpermeability independent of disease severity and alterations in the endothelial angiopoietin/Tie2 system. Nonetheless, circulating angiopoietin-2 might be of interest in the context of organ injury and patient outcome in COVID-19.
Availability of Data and Materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- AKI:
-
Acute kidney injury
- ARDS:
-
Acute respiratory distress syndrome
- SARS-CoV-2:
-
Severe acute respiratory distress syndrome coronavirus 2
- ACE2:
-
Angiotensin-converting enzyme 2
- ICU:
-
Intensive care unit
- PCR:
-
Polymerase chain reaction
- KDIGO:
-
Kidney disease improving global outcomes
- ECIS:
-
Electric cell-substrate impedance sensing
- ELISA:
-
Enzyme-linked immunosorbent assay
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the curve
- vWF:
-
Von Willebrand factor
- BMI:
-
Body mass index
References
Pine AB, Meizlish ML, Goshua G, et al. Circulating markers of angiogenesis and endotheliopathy in COVID-19. Pulm Circ. 2020;10(4):2045894020966547.
Nadim MK, Forni LG, Mehta RL, et al. COVID-19-associated acute kidney injury: consensus report of the 25th acute disease quality initiative (ADQI) workgroup. Nat Rev Nephrol. 2020;16(12):747–64.
Tzotzos SJ, Fischer B, Fischer H, et al. Incidence of ARDS and outcomes in hospitalized patients with COVID-19: a global literature survey. Crit Care. 2020;24(1):516.
Gupta A, Madhavan MV, Sehgal K, et al. Extrapulmonary manifestations of COVID-19. Nat Med. 2020;26(7):1017–32.
Brodin P. Immune determinants of COVID-19 disease presentation and severity. Nat Med. 2021;27(1):28–33.
Jin Y, Ji W, Yang H, et al. Endothelial activation and dysfunction in COVID-19: from basic mechanisms to potential therapeutic approaches. Signal Transduct Target Ther. 2020;5(1):293.
Vassiliou AG, Kotanidou A, Dimopoulou I, et al. Endothelial damage in acute respiratory distress syndrome. Int J Mol Sci. 2020;21(22):8793.
Teuwen LA, Geldhof V, Pasut A, et al. COVID-19: the vasculature unleashed. Nat Rev Immunol. 2020;20(7):389–91.
Wang Q, Zhang Y, Wu L, et al. Structural and functional basis of SARS-CoV-2 entry by using human ACE2. Cell. 2020;181(4):894-904.e9.
Sluimer JC, Gasc JM, Hamming I, et al. Angiotensin-converting enzyme 2 (ACE2) expression and activity in human carotid atherosclerotic lesions. J Pathol. 2008;215(3):273–9.
Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417–8.
Hamming I, Timens W, Bulthuis MLC, et al. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203(2):631–7.
Ackermann M, Verleden SE, Kuehnel M, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med. 2020;383(2):120–8.
Rovas A, Osiaevi I, Buscher K, et al. Microvascular dysfunction in COVID-19: the MYSTIC study. Angiogenesis. 2021;24(1):145–57.
Dupont A, Rauch A, Staessens S, et al. Vascular endothelial damage in the pathogenesis of organ injury in severe COVID-19. Arterioscler Thromb Vasc Biol. 2021;41(5):1760–73.
Michalick L, Weidenfeld S, Grimmer B, et al. Plasma mediators in patients with severe COVID-19 cause lung endothelial barrier failure. Eur Respir J. 2021;57(3):2002384.
Parikh SM. Angiopoietins and Tie2 in vascular inflammation. Curr Opin Hematol. 2017;24(5):432–8.
Sack KD, Kellum JA, Parikh SM. The Angiopoietin-Tie2 pathway in critical illness. Crit Care Clin. 2020;36(2):201–16.
Juffermans NP, van den Brom CE, Kleinveld DJB. Targeting endothelial dysfunction in acute critical illness to reduce organ failure. Anesth Analg. 2020;131(6):1708–20.
Smadja DM, Guerin CL, Chocron R, et al. Angiopoietin-2 as a marker of endothelial activation is a good predictor factor for intensive care unit admission of COVID-19 patients. Angiogenesis. 2020;23(4):611–20.
Vassiliou AG, Keskinidou C, Jahaj E, et al. ICU admission levels of endothelial biomarkers as predictors of mortality in critically ill covid-19 patients. Cells. 2021;10(1):186.
Villa E, Critelli R, Lasagni S, et al. Dynamic angiopoietin-2 assessment predicts survival and chronic course in hospitalized patients with COVID-19. Blood Adv. 2021;5(3):662–73.
Dekker NAM, van Leeuwen ALI, van Strien WWJ, et al. Microcirculatory perfusion disturbances following cardiac surgery with cardiopulmonary bypass are associated with in vitro endothelial hyperpermeability and increased angiopoietin-2 levels. Crit Care. 2019;23(1):117.
Jongman RM, van Klarenbosch J, Molema G, et al. Angiopoietin/Tie2 dysbalance is associated with acute kidney injury after cardiac surgery assisted by cardiopulmonary bypass. PLoS ONE. 2015;10(8): e0136205.
Li F, Yin R, Guo Q. Circulating angiopoietin-2 and the risk of mortality in patients with acute respiratory distress syndrome: a systematic review and meta-analysis of 10 prospective cohort studies. Ther Adv Respir Dis. 2020;14:1753466620905274.
Trieu M, van Meurs M, van Leeuwen ALI, et al. Vasculotide, an angiopoietin-1 mimetic, restores microcirculatory perfusion and microvascular leakage and decreases fluid resuscitation requirements in hemorrhagic shock. Anesthesiology. 2018;128(2):361–74.
Dekker NAM, van Meurs M, van Leeuwen ALI, et al. Vasculotide, an angiopoietin-1 mimetic, reduces pulmonary vascular leakage and preserves microcirculatory perfusion during cardiopulmonary bypass in rats. Br J Anaesth. 2018;121(5):1041–51.
Ranieri VM, Rubenfeld GD, Thompson BT, et al. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307(23):2526–33.
Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120(4):c179–84.
Szulcek R, Bogaard HJ, van Nieuw Amerongen GP. Electric cell-substrate impedance sensing for the quantification of endothelial proliferation, barrier function, and motility. J Vis Exp. 2014;85:51300.
van Leeuwen ALI, Naumann DN, Dekker NAM, et al. In vitro endothelial hyperpermeability occurs early following traumatic hemorrhagic shock. Clin Hemorheol Microcirc. 2020;75(2):121–33.
Koning NJ, Overmars MAH, van den Brom CE, et al. Endothelial hyperpermeability after cardiac surgery with cardiopulmonary bypass as assessed using an in vitro bioassay for endothelial barrier function. Br J Anaesth. 2016;116(2):223–32.
Abou-Arab O, Bennis Y, Gauthier P, et al. Association between inflammation, angiopoietins, and disease severity in critically ill COVID-19 patients: a prospective study. Br J Anaesth. 2021;126(3):e127–30.
Volbeda M, Jou-Valencia D, van den Heuvel MC, et al. Comparison of renal histopathology and gene expression profiles between severe COVID-19 and bacterial sepsis in critically ill patients. Crit Care. 2021;25(1):202.
van der Heijden M, van Nieuw Amerongen GP, van Bezu J, et al. Opposing effects of the angiopoietins on the thrombin-induced permeability of human pulmonary microvascular endothelial cells. PLoS ONE. 2011;6(8): e23448.
Benest AV, Kruse K, Savant S, et al. Angiopoietin-2 is critical for cytokine-induced vascular leakage. PLoS ONE. 2013;8(8): e70459.
Schmaier AA, Pajares Hurtado GM, Manickas-Hill ZJ, et al. Tie2 activation protects against prothrombotic endothelial dysfunction in COVID-19. JCI Insight. 2021;6(20): e151527.
Guan W-J, Ni Z-Y, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–20.
Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region Italy. JAMA. 2020;323(16):1574–81.
Acknowledgements
We would like to thank all medical, paramedical, laboratory and nursing staff involved in the care of the COVID-19 patients for making it possible to build the Amsterdam UMC COVID-19 Biobank in The Netherlands. The Amsterdam UMC COVID-19 Biobank Study Group: M.A. van Agtmael2, A.G. Algera1, R. van Amstel1, B. Appelman2, F.E.H.P. van Baarle1, D.J.C. Bax3, M. Beudel4, H.J. Boogaard5, M. Bomers2, P.I. Bonta5, L.D.J. Bos1, M. Botta1, J. de Brabander2, G.J. de Bree2, S. de Bruin1, M. Bugiani5, D. Buis1, E.B. Bulle1, O. Chouchane2, A.P.M. Cloherty3, M.C.F.J. de Rotte12, M. Dijkstra12, D.A. Dongelmans1, R.W.G. Dujardin1, P.E. Elbers1, L.M. Fleuren1, S.E. Geerlings2, T.B.H. Geijtenbeek3, A.R.J. Girbes1, A. Goorhuis2, M.P. Grobusch2, F.M.J. Hafkamp3, L.A. Hagens1, J. Hamann7, V.C. Harris2, R. Hemke8, S.M. Hermans2, L.M.A. Heunks1, M.W. Hollmann6, J. Horn1, J.W. Hovius2, M.D. de Jong9, R. Koning4, E.H.T. Lim1, N. van Mourik1, J.F. Nellen2, E.J. Nossent5, F. Paulus1, E. Peters2, D. Piña-Fuentes4, T. van der Poll2, B. Preckel6, J.M. Prins2, S.J. Raasveld1, T.D.Y. Reijnders2, M. Schinkel2, F.A.P. Schrauwen12, M.J. Schultz1, A.R. Schuurman10, J. Schuurmans1, K. Sigaloff1, M.A. Slim1,2, P. Smeele5, M.R. Smit1, C. Stijnis2, W. Stilma1, C.E. Teunissen11, P. Thoral1, A.M. Tsonas1, P.R. Tuinman1, M. van der Valk2, D.P. Veelo6, C. Volleman1, H. de Vries1, L.A. van Vught1,2, M. van Vugt2, D. Wouters12, A.H. Zwinderman13, M.C. Brouwer4, W.J. Wiersinga2, A.P.J. Vlaar1, D. van Beek4. 1Department of Intensive Care, Amsterdam UMC, Amsterdam, The Netherlands; 2Department of Infectious Diseases, Amsterdam UMC, Amsterdam, The Netherlands; 3Experimental Immunology, Amsterdam UMC, Amsterdam, The Netherlands; 4Department of Neurology, Amsterdam UMC, Amsterdam Neuroscience, Amsterdam, The Netherlands; 5Department of Pulmonology, Amsterdam UMC, Amsterdam, The Netherlands; 6Department of Anesthesiology, Amsterdam UMC, Amsterdam, The Netherlands; 7Amsterdam UMC Biobank Core Facility, Amsterdam UMC, Amsterdam, The Netherlands; 8Department of Radiology, Amsterdam UMC, Amsterdam, The Netherlands; 9Department of Medical Microbiology, Amsterdam UMC, Amsterdam, The Netherlands; 10Department of Internal Medicine, Amsterdam UMC, Amsterdam, The Netherlands; 11Neurochemical Laboratory, Amsterdam UMC, Amsterdam, The Netherlands; 12Department of Clinical Chemistry, Amsterdam UMC, Amsterdam, The Netherlands; 13Department of Clinical Epidemiology, Biostatistics and Bioinformatics, Amsterdam UMC, Amsterdam, The Netherlands.
Funding
CEvdB is financially supported by the European Society of Intensive Care Medicine (Levi-Montalcini Award 2017), the Dutch Society of Anesthesiology (Young Investigator Grant 2017), and the Dutch Research Council (Veni 2019). The remaining authors are financially supported by their department. No financial support was provided from industrial companies.
Author information
Authors and Affiliations
Consortia
Contributions
CEvdB and APJV were responsible for the conception and design of the study. CV, CEvdB, APJV and RI were responsible for the acquisition and analysis of the data. CV and CEvdB were responsible for the interpretation of the data. CV and CEvdB drafted the manuscript. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethics Approval and Consent to Participate
The institutional review board and the biobank ethics committee of the Amsterdam UMC approved the biobank study protocol (protocol number 2020_182) on the 9th of January 2021.
Consent for Publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Volleman, C., Ibelings, R., Vlaar, A.P.J. et al. Endothelial Permeability and the Angiopoietin/Tie2 System Following Mild and Severe COVID-19. Artery Res 29, 83–93 (2023). https://doi.org/10.1007/s44200-023-00036-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44200-023-00036-2