Abstract
Background
This study examines incidence, mortality, medical expenditure and prescription patterns for asthma on a national scale, particularly in Asian countries for asthma is limited. Our aim is to investigate incidence, mortality, prescription patterns and provide a comprehensive overview of healthcare utilization trends for asthma from 2009 to 2018.
Methods
We included patients diagnosed with asthma between 2009 and 2018. We excluded patients with missing demographic data. Our analysis covered comorbidities, including diabetes mellitus, hypertension, allergic rhinitis, eczema, atopic dermatitis, coronary artery disease, congestive heart failure, chronic kidney disease, chronic hepatitis, stroke, and cancer. Investigated medications comprised oral and intravenous steroids, short-acting beta-agonists, inhaled corticosteroids (ICS), combinations of ICS and long-acting beta-agonists, long-acting muscarinic antagonists, and leukotriene receptor antagonists montelukast. We also assessed the number of outpatient visits, emergency visits, and hospitalizations per year, as well as the average length of hospitalization and average medical costs.
Results
The study included a final count of 88,244 subjects from 1,998,311 randomly selected samples between 2000 and 2019. Over the past decade, there was a gradual decline in newly diagnosed asthma patients per year, from 10,140 to 6,487. The mean age annually increased from 47.59 in 2009 to 53.41 in 2018. Over 55% of the patients were female. Eczema was diagnosed in over 55% of the patients. Around 90% of the patients used oral steroids, with a peak of 97.29% in 2018, while the usage of ICS varied between 86.20% and 91.75%. Intravenous steroids use rose from 40.94% in 2009 to 54.14% in 2018. The average annual hospital stay ranged from 9 to 12 days, with a maximum of 12.26 days in 2013. Lastly, the average medical expenses per year ranged from New Taiwan dollars 5558 to 7921.
Conclusions
In summary, both asthma incidence and all-cause mortality rates decreased in Taiwan from 2009 to 2018. Further analysis of medical expenses in patients with asthma who required multiple hospitalizations annually revealed an increase in outpatient and emergency visits and hospitalizations, along with longer hospital stays and higher medical costs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Asthma is a widespread, long-term lung condition that impacts numerous individuals across various nations globally [1]. It is marked by fluctuating signs such as coughing, wheezing, shortness of breath, and chest constriction, alongside inconsistent limitations in the outflow of breath. These symptoms and breathing restrictions typically fluctuate in their severity and occurrence over time. Over the last ten years, advancements have been achieved in asthma management, especially regarding creative strategies that utilize current medications and new treatments for severe cases of asthma. Previously, for mild asthma, guidelines recommended a regimen of long-term low-dose inhaled corticosteroids (ICS) and as-needed short-acting beta-agonists (SABA) [2]. However, many patients with mild asthma show poor adherence to daily ICS due to sporadic symptoms, leading to a heavy reliance on SABA during acute exacerbation. Despite their seemingly mild condition, these patients remain at risk for serious asthma attacks and related fatalities. Additionally, both exclusive SABA treatment and its excessive use are linked to negative disease outcomes. These issues have prompted the asthma care community to explore new strategies and reconsider the existing approach to enhance the management of asthma [3]. A new once-daily fluticasone furoate (FF) was a monotherapy therapy for asthma, and when combined with vilanterol (VI), a novel once-daily inhaled long-acting beta-agonists (LABA), it is being studied for both asthma management and significant airway protection in individuals with asthma [4]. The Salford Lung Study [5] is a comprehensive Phase III trial involving over 4,000 patients across multiple centers. This open-label, randomized controlled trial aims to assess the efficacy and safety of starting treatment with FF/VI to the standard care therapy for asthma over 52 weeks. Patients who began treatment with FF/VI demonstrated better improvements in asthma control compared to those who continued with their regular treatment, which typically includes ICS either alone or in combination with LABA. Tiotropium has proven beneficial as an additional maintenance therapy alongside medium or high-dose ICS, with or without LABA, for asthma treatment [6]. It has gained approval in the USA, countries in Europe for this use. Studies in adults have shown that tiotropium improved lung function and asthma management while safety profile was similar to placebo [7]. Moreover, clinical trials in children with symptomatic asthma despite received ICS therapy indicate that tiotropium, when used as a supplementary treatment to ICS is safe and effective. It also shows a tendency to improve asthma control, echoing the results observed in adult populations [8]. While the development of innovative relief strategies and treatments for severe asthma marks an exciting advancement, numerous challenges remain. Current clinical trials are in progress, aiming to address and overcome some of these challenges. The International Study of Asthma and Allergies in Childhood (ISAAC) is a standardized asthma survey since 1995 [9]. Global Asthma Network (GAN), began in 2012 [10], after the ISAAC and observed that the prevalence of asthma symptoms was on the rise in several countries, and some disease severities were high. GAN Phase I extends the research of ISAAC by gathering additional data on the prevalence, severity, diagnosis, and management of asthma, along with some allergic disease. It also looks into emergency room visits, hospital admissions, and the usage of essential asthma medications. Taiwan participated in this study, concentrating on a demographic of adolescents aged 13–14 years who completed a questionnaire in 2017. The objective was to explore the current prevalence of asthma in Taiwanese teens. However, the study was limited to only surveying individuals within the 13-14-year age group [11]. The aim of our study utilized nationwide claims data to analyze the yearly patterns of asthma in Taiwan over the period from 2009 to 2018. Additionally, it assessed the trends in the incidence and mortality rates of patients with asthma and examined the medical expenditure, identifying the shifts in these aspects among asthma patients in Taiwan throughout the decade.
2 Materials and methods
2.1 Data Source
On January 1, 1995, the Department of Health of the Executive Yuan formally established the Central Health Insurance Bureau, and on March 1, 1995, the National Health Insurance was officially implemented. So far, the national acceptance rate is as high as 99%. Since 2000, it has provided value-added services to the academic health insurance database on the premise of protecting public privacy and data security to facilitate public health and academic research. The disease coding for National Health Insurance (NHI) database follows the International Classification of Diseases, 9th Revision and 10th Revision, Clinical Modification (ICD-9-CM and ICD-10-CM). This study was approved by the Institutional Review Board of the Research Ethics Committee of China Medical University Hospital (CMUH110-REC1-038(CR-2)).
2.2 Study Population and Variables
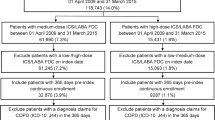
Asthma (ICD-9-CM: 493; ICD-10-CM: J45) patients with at least two outpatient visits or one hospitalization record were identified between January 1, 2009 and December 31, 2018; the date of the first record was defined as the date of asthma diagnosis (index date). The exclusion criteria include those missing age or gender data. Figure 1 was the flow chart of study design. The final number of subjects included was 88,244.
The variables in the study were age group (< 20, 20–29, 30–39, 40–49, 50–59, ≥ 60), gender, comorbidities [diabetes mellitus (ICD-9-CM: 250; ICD-10-CM: E08-E13), hypertension (ICD-9-CM: 401–405; ICD-10-CM: I10-I15), allergic rhinitis (ICD-9-CM: 477; ICD-10-CM: J30), eczema (ICD-9-CM: 692.0-692.6, 692.81, 692.83, 692.89, 692.9; ICD-10-CM: L23-L25, L30.0, L30.2, L30.8, L30.9), atopic dermatitis (ICD-9-CM: 691; ICD-10-CM: L20), dyslipidemia (ICD-9-CM 272; ICD-10-CM: E77, E78), coronary artery disease (ICD-9-CM: 410–414; ICD-10-CM: I20-I25), congestive heart failure (ICD-9-CM: 428.0; ICD-10-CM: I50.2-I50.9), chronic kidney disease (ICD-9-CM: 585; ICD-10-CM: N18.4-N18.9), chronic hepatitis (ICD-9-CM: 571.4; ICD-10-CM: K73), stroke (ICD-9-CM: 430–438; ICD-10-CM: I60-I69), and cancer (ICD-9-CM: 140–208; ICD-10-CM: C00-C99)], medications [oral steroids (anatomical therapeutic chemical (ATC) code: A01AC01, A01AC91, A07EA06, A14AA02, A14AA03, G01AF04, G01AX05, H02AA02, H02AB01, H02AB02, H02AB04, H02AB05, H02AB06, H02AB08, H02AB10, H02BX, H02BX91, M01BA03, S02CA04, S02CA06), intravenous steroids (ATC code: A14AB01, D11AH05, H02AB, H02AB01, H02AB02, H02AB04, H02AB06, H02AB08, H02AB09, H02BX), SABA (ATC code: R03AC), ICS (ATC code: R03BA), ICS/ LABA (ATC code: R03AK), long acting muscarinic antagonists (LAMA) (ATC code: R03BB), and leukotriene receptor antagonists (LTRA) montelukast (ATC code: R03DC)], outpatient department (OPD) visits per year, emergency room (ER) visits per year, hospital admissions per year, average days of hospitalization per year, and average medical costs of asthma care per year.
Detailed variable settings were described as follows. Comorbidities were identified before the asthma diagnosis, evaluating 5-year intervals before the index date. The medication regimen was identified during the first year since the asthma diagnosis. The OPD visits per year are defined and calculated as the total number of OPD visits during the first year since the asthma diagnosis. ER visits per year are defined and calculated as the total number of ER visits during the first year since the asthma diagnosis. Hospital admissions per year are defined and calculated as the total number of hospitalizations during the first year since the asthma diagnosis. The average days of hospitalization per year are defined and calculated as the total days of hospitalizations during the first year since the asthma diagnosis. The medical costs for the OPD visit, ER visit, and hospitalization were available, and all were recorded with the new Taiwan dollar (NTD) in the database. The average medical costs per year were defined and calculated as the total costs for asthma care (OPD, ER, and hospitalization) during the first year since the asthma diagnosis.
2.3 Statistical Analysis
The demographic characteristics of patients diagnosed with asthma in each year from 2009 to 2018 were analyzed. The patient’s age, gender, comorbidities, medications, OPD visits per year, ER visits per year, hospitalizations per year, length of hospitalization per year, and medical costs per year are estimated. Categorical variables were represented by numbers and percentages, while continuous variables were represented by mean and standard deviation (SD). The all-cause mortality rate of asthma per year is calculated by dividing the total number of all-cause deaths of patients with asthma in a certain year (2009–2018) by the total population (the same mid-year), resulting in a rate per 1000 person-years. The incidence rate of asthma per year is determined by dividing the total number of newly diagnosed asthma in a certain year (2009–2018) by the total population (the same mid-year), resulting in a rate per 1000 person-years. All statistical analysis were performed by SAS software, version 9.4 (SAS Institute Inc., Cary, NC).
3 Results
The baseline characteristics of patients diagnosed with asthma from 2009 to 2018 are displayed in Table 1, including age, gender, and comorbidities. Over the past decade, there has been a gradual decline in the number of patients, decreasing from 10,140 to 6487. The mean age annually varied from 47.59 (SD = 21.13) to 53.41 (SD = 17.67) years. Throughout these ten years, over half of the patients were female. More than 55% of the patients were diagnosed with eczema, persisting for the entire decade. The second most common comorbidity was allergic rhinitis.
Table 2 presents the seven common asthma medications, including oral steroids, intravenous steroids, SABA, ICS, ICS/ LABA, LAMA, and LTRA. Despite the yearly decrease in the number of asthma diagnoses, about 90% were treated with oral steroids, peaking at 97.29% in 2018. ICS usage also remained high, ranging from 86.20 to 91.75%. Additionally, the use of intravenous steroids increased from 40.94% in 2009 to 54.14% in 2018.
Table 3 shows the average number of OPD visits, ER visits, and hospitalizations, as well as the average days of hospitalization and medical costs for asthma patients per year over the past decade. Figure 2 shows the trend of OPD visits, ER visits, and hospitalizations in patients with asthma by years. From 2009 to 2018, the average annual OPD visits were approximately 2–3, while ER visits and hospitalizations were about 1. Figure 3 shows the average days that patients spend in hospital per year. The average length of stay in hospital varied from 9 to 12 days, reaching a maximum of 12.26 days (SD = 16.80) in 2013. Lastly, the average medical expenses per year ranged from NTD 5558 to 7922.
Table 4 presents the characteristics of asthma patients with more than two hospitalizations per year. Since 2011, the number of patients has consistently exceeded 100, peaking at 171 in 2015, with over half being female. This group of patients with asthma experienced more than two hospitalizations (acute exacerbations) per year, indicating they may have a more severe form of asthma (difficult to control with the current treatment). The overall number of OPD visits, ER visits, and hospitalizations, as well as the length of hospital stay and medical costs, have increased.
Table 5 details the dosages of asthma prescriptions for SABA, ICS, ICS/ LABA, and LAMA. The dosages of SABA < 75 mg comprised about 72%, while over 90% of the ICS dosages were < 3750 µg. The dosages of ICS/ LABA < 6304, 6304–16,500, > 16,500 µg were evenly distributed. From 2009 to 2013, most LAMA dosages exceeded 583,200 µg, but after 2014, dosages of < 4,500 µg accounted for about half.
Table 6 shows the all-cause mortality rate of asthma per year. The mortality was calculated by dividing the total number of all-cause deaths of patients with asthma in a year by the total population in the same mid-year. All-cause mortality rates for the total asthma population, as well as for males and females, decreased annually. All-cause mortality rates of total asthma population, males, and females per 1000 were 0.46, 0.51, and 0.41 during 2009–2018, respectively.
Table 7 shows the incidence rate of asthma during the study period. The incidence rates for total asthma population, as well as males and females, also decreased annually. The incidence rates per 1000 were 4.93 for overall, 4.28 for males, and 5.58 for females during 2009–2018, respectively.
4 Discussion
Our data indicates a declining trend in asthma incidence rates from 2009 to 2018 for overall, male, and female populations. The total incidence rates of asthma per 1000 persons for overall, male, and female are 4.93, 4.28, and 5.58, respectively. Additionally, the data reveals that the average annual OPD visits ranged from 2 to 3, with ER visits and hospitalizations typically around 1. The duration of hospital stays fluctuated between 9 and 12 days per year. Furthermore, the annual mortality rates for the overall, male, and female populations have been decreasing. The overall mortality rates per 1000 asthma patients were 0.46 for the total population, 0.51 for males, and 0.41 for females.
Many studies provide substantial evidence of a connection between allergic rhinitis and asthma, consistently showing they often occur together. Findings reveal that allergic rhinitis are present in 28–78% of patients with asthma [12,13,14], markedly more than the 5–20% rate found in the general population [15]. A guideline report that as many as 38% of people with allergic rhinitis are also affected by asthma, while between 6% and 85% of those with asthma report experiencing nasal symptoms [16]. In our data, we conducted a 10-year follow-up and found that 42–49% of patients with asthma also had allergic rhinitis, which is consistent with findings from previous studies. The presence of allergic rhinitis significantly impacts severe asthma, elevating its incidence among both older and younger populations. This link between allergic rhinitis and heightened asthma severity has been documented in studies involving both children and adults, as noted by several researchers [17,18,19,20].
Atopic dermatitis and eczema, persistent inflammatory skin conditions often linked with respiratory allergies, stand as prevalent skin disorders seen in those with asthma. Asthma, eczema, and atopic dermatitis share numerous comorbidities and are associated with one another, potentially due to immunological disruption, especially the expression of Th2 cytokines [21]. The prevalence of eczema in asthma patients varies, indicating a significant overlap between eczema and other allergic conditions, including asthma. Atopic dermatitis, the most common form of eczema, is strongly linked to a personal or family history of asthma and other allergic diseases, suggesting a high rate of co-occurrence. Previous studies, including one by Pourpak et al. [22], indicate that asthma occurs more frequently in patients with atopic dermatitis, though the exact causative factors are unclear. According to Pourpak et al. [22], 27.5% of patients with atopic dermatitis were found to have asthma. However, there is limited information regarding the prevalence of eczema and atopic dermatitis in patients with asthma. Nonetheless, our data highlight a significant correlation between eczema and asthma, particularly among individuals with asthma and the association between eczema and varying degrees of asthma severity warrants further investigation.
From our data, we found that over 90% of patients with asthma had at some point received oral steroids, and more than 50% had received intravascular steroids after 2015. The trend for both oral and intravascular steroids use has been increasing. This may suggest that many asthma patients have poor control or frequent acute exacerbations, necessitating systemic steroids treatment. Despite a 2010 study showing that adding LAMA to inhaled corticosteroids can improve symptoms and lung function in patients with inadequately controlled asthma, the percentage of asthma patients receiving LAMA treatment remains low.
The provision to exempt extended prescriptions for chronic diseases after a visit to the outpatient department was designed to reduce unnecessary outpatient visits for medication refills in Taiwan. Patients with stable chronic conditions can utilize this exemption to receive free medications for up to 60 days after obtaining a 30-day supply from the hospital. After receiving this initial supply from the hospital’s outpatient department, most patients can directly acquire an additional 60 days of outpatient prescription drugs from pharmacy stores. Patients with good adherence to their chronic disease management typically need to visit the hospital four times a year. According to our data, the average number of outpatient department visits for patients with asthma was 3.39 in 2018. This suggests that there is room for improvement in asthma treatment adherence.
Observational and database research has shown that patients with asthma who have a history of frequent exacerbations or eosinophilic inflammation face an increased risk of subsequent acute exacerbation [23,24,25].
Patients identified in respective US and UK databases were found to have varying experiences based on their asthma severity. Those with severe asthma, a history of two or more exacerbations compared to fewer than two, and severe uncontrolled asthma versus non-severe asthma experienced the highest rates of asthma-related emergency department visits and hospital readmissions within 30 days [26]. We analyzed our patients with asthma who had more than two hospitalizations per year. Since 2011, the number of patients in this group has consistently exceeded 100, reaching a peak of 171 in 2015, with over half being female. Their mean age ranged from 58 to 67, and they needed to OPD visits an average of 8 times per year, with an average of 2 ER visits annually. The length of their hospital stays ranged from 19 to 31 days per year. This group incurred significantly higher medical costs compared to the general asthma population.
Drawing from the 2019 Global Burden of Disease study, research outlined spatial and temporal patterns in asthma incidence and mortality worldwide and in 204 countries from 1990 to 2019. Over this period, asthma incidence declined from 6.01 per 1,000 to 4.78 per 1,000, while asthma mortality rates fell from 8.60 per 100,000 to 5.96 per 100,000 [27]. Our data show comparable trends. Between 2009 and 2018, the incidence rates and mortality in patients with asthma for the overall population, as well as for males and females, have consistently decreased each year. Specifically, the total incidence rates for the overall population, males, and females are 4.93, 4.28, and 5.58 per 1,000 persons, respectively.
There was a widespread trend of observing lower age-standardized asthma mortality rates in developed countries, while undeveloped countries exhibited higher mortality rates. This difference implies that unequal access to preventive and treatment services among socioeconomically disadvantaged groups could impede continuous advancements in reducing asthma-related deaths. In numerous low-income and lower-middle-income countries, issues like underdiagnosis, misdiagnosis, and insufficient treatment lead to many preventable asthma incidents and fatalities [28].
The study encountered several limitations. One primary issue was the reliance on physician diagnoses for asthma without a universally accepted physiological benchmark. The precision of asthma incidence measurements was influenced by access to healthcare. Furthermore, the analysis of incidence was based on estimated cross-sectional data from the population at mid-year. On the positive side, a major strength of this study lies in its national scale, employing a comprehensive insurance database that covers more than 99% of the population in Taiwan. This broad reach provides a strong foundation for the credible observation of a decreasing asthma incidence and mortality trend in Taiwan.
5 Conclusion
In summary, both asthma incidence and mortality rates decreased in Taiwan from 2009 to 2018. There is potential to improve adherence among asthma patients. The utilization of LAMA can be increased in patients with asthma who continue to experience symptoms and poor control despite receiving ICS/ LABA treatment. Patients with asthma who are hospitalized twice a year incur higher medical costs compared to the general asthma population.
Data Availability
No datasets were generated or analysed during the current study.
Abbreviations
- ATC:
-
Anatomical therapeutic chemical
- ER:
-
Emergency room
- FF:
-
Fluticasone furoate
- GAN:
-
Global Asthma Network
- ICD-9-CM:
-
International Classification of Diseases, 9th Revision, Clinical Modification
- ICD-10-CM:
-
International Classification of Diseases, 10th Revision, Clinical Modification
- ICS:
-
Inhaled corticosteroids
- ISAAC:
-
International Study of Asthma and Allergies in Childhood
- NHI:
-
National Health Insurance
- OPD:
-
Outpatient department
- SABA:
-
Short-acting beta-agonists
- LABA:
-
Long-acting beta-agonists
- LAMA:
-
Long-acting muscarinic antagonists
- LTRA:
-
Leukotriene receptor antagonist
- VI:
-
Vilanterol
References
Asher MI, Rutter CE, Bissell K, et al. Worldwide trends in the burden of asthma symptoms in school-aged children: global Asthma Network Phase I cross-sectional study. Lancet. 2021;398:1569–80.
Myers TR. Guidelines for asthma management: a review and comparison of 5 current guidelines. Respir Care. 2008;53:751–67.
Reddel HK, Bacharier LB, Bateman ED, et al. Global Initiative for Asthma Strategy 2021: executive summary and rationale for key changes. Am J Respir Crit Care Med. 2022;205:17–35.
Oliver A, Quinn D, Goldfrad C, van Hecke B, Ayer J, Boyce M. Combined fluticasone furoate/vilanterol reduces decline in lung function following inhaled allergen 23 h after dosing in adult asthma: a randomised, controlled trial. Clin Transl Allergy. 2012;2:11.
Albertson TE, Murin S, Sutter ME, Chenoweth JA. The Salford Lung Study: a pioneering comparative effectiveness approach to COPD and Asthma in clinical trials. Pragmat Obs Res. 2017;8:175–81.
Peters SP, Kunselman SJ, Icitovic N, Moore WC, Pascual R, Ameredes BT, et al. Tiotropium bromide step-up therapy for adults with uncontrolled asthma. N Engl J Med. 2010;363:1715–26.
Hamelmann E, Vogelberg C, Szefler SJ. Tiotropium for the treatment of asthma in adolescents. Expert Opin Pharmacother. 2017;18:305–12.
Vogelberg C, Moroni-Zentgraf P, Leonaviciute-Klimantaviciene M, Sigmund R, Hamelmann E, Engel M, Szefler S. A randomised dose-ranging study of tiotropium Respimat® in children with symptomatic asthma despite inhaled corticosteroids. Respir Res. 2015;16:20.
Asher MI, Keil U, Anderson HR, Beasley R, Crane J, Martinez F, Mitchell EA, Pearce N, Sibbald B, Stewart AW, et al. International Study of Asthma and allergies in Childhood (ISAAC): rationale and methods. Eur Respir J. 1995;8:483–91.
Ellwood P, Asher MI, Billo NE, Bissell K, Chiang CY, Ellwood EM, El-Sony A, García-Marcos L, Mallol J, Marks GB, Pearce NE, Strachan DP. The Global Asthma Network rationale and methods for phase I global surveillance: prevalence, severity, management and risk factors. Eur Respir J. 2017;49:1601605.
Su KW, Yan DC, Ou LS, Lin LL, Wu CY, Huang SJ, Yao TC, Yeh KW, Huang JL. Prevalence, associated factors, and impact of adolescent asthma in Taiwan: Global Asthma Network phase I survey. World Allergy Organ J. 2023;16(7):100794.
Blair H. Natural history of childhood asthma: 20-year follow-up. Arch Dis Child. 1977;52:613–9.
Smith JM. Epidemiology and natural history of asthma, allergic rhinitis and atopic dermatitis (eczema). In: Middleton E, editor. Allergy, principles and practice. 3rd ed. St. Louis, Mo.: CV Mosby Co.; 1988.
Pedersen PA, Weeke ER. Asthma and allergic rhinitis in the same patients. Allergy. 1983;38:25–9.
Settipane GA. Allergic rhinitis—update. Otolaryngol Head Neck Surg. 1986;94:470–5.
Brożek JL, Bousquet J, Agache I, Agarwal A, Bachert C, Bosnic-Anticevich S, et al. Allergic Rhinitis and its impact on Asthma (ARIA) guidelines-2016 revision. J Allergy Clin Immunol. 2017;140:950–8.
Tohidinik HR, Mallah N, Takkouche B. History of allergic rhinitis and risk of asthma; a systematic review and meta-analysis. World Allergy Organ J. 2019;12:100069.
Oka A, et al. Ongoing allergic rhinitis impairs asthma control by enhancing the lower airway infammation. J Allergy Clin Immunol Pract. 2014;2:172–8.
To M, et al. Persistent asthma from childhood to adulthood presents a distinct phenotype of adult asthma. J Allergy Clin Immunol Pract. 2020;8:1921–7.
Deliu M, et al. Impact of rhinitis on asthma severity in school-age children. Allergy. 2014;69:1515–21.
Yaneva M, Darlenski R. The link between atopic dermatitis and asthma- immunological imbalance and beyond. Asthma Res Pract. 2021;7:16.
Pourpak Z, Mozaffari H, Gharagozlou M, Daneshmandi Z, Moin M. Asthma in patients with atopic dermatitis. Indian J Pediatr. 2008;75:139–41.
Schatz M, Meckley LM, Kim M, Stockwell BT, Castro M. Asthma exacerbation rates in adults are unchanged over a 5-year period despite high-intensity therapy. J Allergy Clin Immunol Pract. 2014;2:570–4. e571.
Miller MK, Lee JH, Miller DP, Wenzel SE. Recent asthma exacerbations: a key predictor of future exacerbations. Respir Med. 2007;101:481–9.
Zeiger RS, Schatz M, Li Q, Chen W, Khatry DB, Gossage D, Tran TN. High blood eosinophil count is a risk factor for future asthma exacerbations in adult persistent asthma. J Allergy Clin Immunol Pract. 2014;2:741–50.
Suruki RY, Daugherty JB, Boudiaf N, et al. The frequency of asthma exacerbations and healthcare utilization in patients with asthma from the UK and USA. BMC Pulm Med. 2017;17:74.
Cao Y, Chen S, Chen X, Zou W, Liu Z, Wu Y, Hu S. Global trends in the incidence and mortality of asthma from 1990 to 2019: an age-period-cohort analysis using the global burden of disease study 2019. Front Public Health. 2022;10:1036674.
Holgate ST, Wenzel S, Postma DS, Weiss ST, Renz H, Sly PD, Asthma. Nat Rev Dis Primers. 2015;1:15025.
Acknowledgements
We are grateful to the MOHW Health and Welfare Data Science Center at China Medical University for providing administrative and technical support.
Funding
The study was supported by Taiwan Ministry of Health and Welfare Clinical Trial Center (MOHW112-TDU-B-212-144004), China Medical University Hospital (DMR-111-105, DMR-112-087, DMR-113-009, DMR-113-156).
Author information
Authors and Affiliations
Contributions
KML, PJC, YTH, TJH, FJT drafted the manuscript. YTH, TJH, FJT collected and analyzed the data. KML and TCS commented on the data analysis and interpretation of results. YTH, TJH, FJT participated in the data preparation and provided important comments on the manuscript. All authors contributed to the article and approved the submitted version. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of the Research Ethics Committee of China Medical University Hospital (CMUH110-REC1-038(CR-2)). This study was performed in accordance with the ethical standards established in the 1964 Declaration of Helsinki and its later amendments. This study conducted by NHI database, and all the individual information data are de-identified, we could not obtain informed consent from study population.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liao, KM., Chen, PJ., Hung, YT. et al. The Incidence, Mortality and Medical Expenditure in Patients with Asthma in Taiwan: Ten-year Nationwide Study. J Epidemiol Glob Health (2024). https://doi.org/10.1007/s44197-024-00230-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44197-024-00230-8