Abstract
Maternal and paternal age at birth is increasing globally. Maternal age may affect perinatal outcomes, but the effect of paternal age and its joint effect with maternal age are not well established. This prospective, multicenter, cohort analysis used data from the University Hospital Advanced Age Pregnant Cohort Study in China from 2016 to 2021, to investigate the separate association of paternal age and joint association of paternal and maternal age with adverse perinatal outcomes. Of 16,114 singleton deliveries, mean paternal and maternal age (± SD) was 38.0 ± 5.3 years and 36.0 ± 4.1 years. In unadjusted analyses, older paternal age was associated with increased risks of gestational diabetes mellitus (GDM), hypertensive disorders of pregnancy, preeclampsia, placenta accreta spectrum disorders, placenta previa, cesarean delivery (CD), and postpartum hemorrhage, preterm birth (PTB), large-for-gestational-age, macrosomia, and congenital anomaly, except for small-for-gestational-age. In multivariable analyses, the associations turned to null for most outcomes, and attenuated but still significant for GDM, CD, PTB, and macrosomia. As compare to paternal age of < 30 years, the risks in older paternal age groups increased by 31–45% for GDM, 17–33% for CD, 32–36% for PTB, and 28–31% for macrosomia. The predicted probabilities of GDM, placenta previa, and CD increased rapidly with paternal age up to thresholds of 36.4–40.3 years, and then plateaued or decelerated. The risks of GDM, CD, and PTB were much greater for pregnancies with younger paternal and older maternal age, despite no statistical interaction between the associations related to paternal and maternal age. Our findings support the advocation that paternal age, besides maternal age, should be considered during preconception counseling.
Trial Registration NCT03220750, Registered July 18, 2017—Retrospectively registered, https://classic.clinicaltrials.gov/ct2/show/NCT03220750.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The past decades have seen a remarkable increase in proportion of live births to parents of advanced age in many countries, especially among fathers aged 35–39 years [1, 2]. Between 1995 and 2015, the number of live births per 1000 fathers aged 35–39 years raised from 50.4 to 69.1 in the US [2], and from 57.5 to 83.6 in the UK [1]. Although the corresponding figure was unknown in China, the average age of marriages for men increased from 24 years in 1990 to 29 years in 2020 [3], approaching the 30 years for men in the US in 2020 [4].
Most previous studies focused on the effects of paternal age on offspring outcomes [5,6,7], but data about the effects on maternal outcomes are sparse and equivocal [6, 8, 9]. For example, one study in Israel found that paternal age of 35 years or older was associated with a higher risk of preeclampsia compared with paternal age of 25–34 years [8], whereas a study in the US did not observe the association [6], despite both studies conducted with large sample sizes. Furthermore, there was still no biological plausible threshold to define advanced paternal age. Defining reliable threshold requires understanding of whether relationship between paternal age and risk of outcome is linear or non-linear, but such study is lacking. Although maternal and paternal age have been shown to independently affect perinatal outcomes [6, 8, 10], their joint effects were still unclear. There are two studies only reported the joint effects for individual outcomes and the results were inconsistent [11, 12]. One study in the Texas–Mexico border found that paternal age of 35 years or older combined with advanced maternal age was associated with an increased risk of gestational hypertensive disorders, compared to paternal and maternal age younger than 35 years [12]. While the other study focusing on low birth weight, and preterm birth did not found any significant associations [11].
Using data from the University Hospital Advanced Age Pregnant (UNIHOPE) Cohort in China, we aimed to examine the separate association of paternal age, and joint associations of paternal and maternal age with adverse perinatal outcomes in mothers and offspring, and attempted to identify potential threshold for defining advanced paternal age by examining the linear or non-linear relationships between paternal age and adverse outcomes.
2 Methods
2.1 Study design and participants
The multicenter prospective UNIHOPE cohort was conducted in China from July 2016 to June 2021, aiming to explore potential predictors of adverse pregnancy outcomes among women of advanced age (ClinicalTrails.gov: NCT03220750) [13]. The cohort was conducted in eight public referral hospitals located in Beijing, Shanghai, Guangzhou, Shenyang, Wuhan, Chongqing, and Chengdu, scattered through the eastern, central, and western regions of China. Pregnant women were enrolled before 14 weeks of gestation, and followed up at 24–28 weeks, 32–34 weeks of gestation, delivery, and 6–12 weeks postpartum, by obstetrician or nurse in the hospitals. Information on sociodemographic characteristics and lifestyle (maternal and paternal), medical and reproductive history, prenatal care of the current pregnancy, and pregnancy outcomes was collected at enrollment and subsequent follow-ups using a structured questionnaire.
Pregnant women were eligible in the UNIHOPE cohort if they attended regular antenatal care and delivered at the included hospitals. Women would be excluded if they had mental disorders or had no ability to provide informed consent. Initially, a total of 22,822 pregnant women were enrolled in the UNIHOPE cohort. For this study, 6708 women who were ended with spontaneous or induced abortions (n = 818), moved out (n = 1725), had multiple pregnancies (n = 1782), had no birthdate (n = 2), or whose partners had no birthdate (n = 2092) or abnormal age (< 20 or > 70 years, n = 289) were excluded. Finally, 16,114 pregnant women remained in the analysis (Fig. 1).
2.2 Exposures and covariates
The main exposure was paternal age, which was defined as the male partner’s age at the time of conception, calculating as subtracting the partner’s birthdate from the last menstrual period date. Paternal age was used continuously or categorically (< 30, 30–34, 35–39, 40–44, and ≥ 45 years) in this analysis, as appropriate. Maternal age was calculated as subtracting the maternal birthdate from the date of delivery, and categorized into four groups: < 35, 35–39, 40–44, and ≥ 45 years.
Other covariates included paternal occupation, alcohol consumption and smoking, as well as maternal ethnicity, education, occupation, alcohol consumption and smoking within 6 months prior to pregnancy, pre-pregnancy body mass index (BMI), gestational age at enrolment, illness before pregnancy, parity, method of conception, annual household income, and delivery year. Gestational age at enrollment was determined by the last menstrual period for women with regular menstrual cycles or by ultrasound for others.
2.3 Outcomes of interest
Interested maternal outcomes included: (1) gestational diabetes mellitus (GDM), defined as a fasting plasma glucose ≥ 5.1 mmol/L or an OGTT 1 h plasma glucose ≥ 10.0 mmol/L, or an OGTT 2 h plasma glucose ≥ 8.5 mmol/L, that occurs or is first diagnosed during pregnancy [14]; (2) hypertensive disorders of pregnancy (HDP), defined as a spectrum of conditions including preeclampsia, preeclampsia superimposed on chronic hypertension, gestational hypertension, and chronic hypertension; (3) preeclampsia, defined as new-onset blood pressures ≥ 140/90 mmHg after 20 weeks of gestation and combined with albuminuria ≥ 0.3 g [15]; (4) placenta accreta spectrum (PAS) disorders, characterized as abnormal trophoblast invasion of part or all of the placenta into the myometrium of the uterine wall [16]; (5) placenta previa (PP), defined as placenta complete or partial covering the internal orifice of cervix; (6) cesarean delivery (CD), identified by inpatient medical records; and (7) postpartum hemorrhage (PPH), defined as a loss of ≥ 500 ml of blood after vaginal delivery or ≥ 1000 ml after CD within 24 h of birth [17].
Interest offspring outcomes included: (1) preterm birth (PTB) defined as a live birth occurred before 37 completed gestational weeks; (2) large-for-gestational-age (LGA) defined as birthweight of > 90th percentile for gestational age of a China reference population [18]; (3) small-for-gestational-age (SGA) defined as birthweight of < 10th percentile for gestational age; (4) macrosomia defined as a newborn with a birthweight ≥ 4000 g; and (5) congenital anomaly defined as congenital structural anomalies for fetus or infants, such as congenital heart defect, Down’s syndrome, polydactylism, and cleft palate.
2.4 Statistical analysis
Differences in paternal and maternal characteristics across paternal age groups were determined using Chi-square tests for categorical variables and one-way analysis of variance with Dunnett corrections for multiple comparisons for continuous variables.
Univariate and multivariable log-binomial regression models were performed to estimate relative risks (RRs) and 95% confidence intervals (95% CIs) of adverse outcomes according to paternal age. Because maternal age was associated with increased risks of maternal and offspring outcomes [10, 19], the joint effects of paternal and maternal age on those adverse outcomes were examined. In analysis of joint effects, pregnant women were categorized into 15 strata according to paternal age (< 30, 30–34, 35–39, 40–44, ≥ 45 years) and maternal age (< 35, 35–39, ≥ 40 years), and women aged < 35 years and paternal age < 30 years were used as the reference category. Whether the associations between paternal age and outcomes differed across maternal age was evaluated by adding a multiplicative interaction term into multivariable models. Additive interaction between paternal age and maternal age was also examined by using Delta method to calculate the relative excess risk due to interaction (RERI) and 95% CI [20].
Multivariable logistic regression with restricted cubic spline were performed to assess the relationships of paternal age with adverse outcomes. The number of knots (between 3 and 7) was determined based on the lowest Akaike information criterion. Adjusted odds of each outcome in 1-year increments of paternal age from 20 to 70 years were calculated, and then transformed to predicted probabilities. The predicted probabilities with 95% confidence intervals (95% CI) were plotted for paternal age to display the relationships visually. If non-linear relationship was observed, segmented model was then used to identify the inflection point [21].
In multivariable analysis, the adjusted covariates included paternal occupation, smoking and alcohol consumption, as well as maternal age, ethnicity, education, occupation, annual household income, smoking, and alcohol consumption within 6 months prior to pregnancy, pre-pregnancy BMI, gestational age at enrolment, illness before pregnancy, parity, method of conception, and delivery year. Missing covariate values were classified into a new category in a dummy variable (0 = not missing; 1 = missing) and included in the models.
To assess the robustness of the results, sensitivity analyses were conducted by using multiply imputed missing values for covariates, or by excluding women who conceived with ART. Additionally, ordinal regression models were used to assess the associations of the paternal and maternal age with perinatal outcomes.
Statistical analyses were performed using SAS software, version 9.4 (SAS Institute, Inc). A 2-sided P < 0.05 was deemed statistically significant.
3 Results
Among 16,114 deliveries included in the analysis, the average paternal age was 38.0 (SD 5.3) years, and the average maternal age was 36.0 (SD 4.1) years. Maternal age increased as increasing paternal age (Table 1). Both paternal and maternal characteristics differed across paternal age groups (Table 1). As compared with paternal age < 30 years group, pregnant women and their partners in older paternal age groups were more likely to be office workers and drink alcohol, and pregnant women were more likely to be overweight or obesity before pregnancy, have illness before pregnancy, to be multipara, and utilize assisted reproductive technology (ART), have higher education level and annual household income (Table 1).
In the unadjusted analysis, pregnant women with older partners were associated with higher risks of all adverse maternal outcomes, as compared with those with partners’ age of < 30 years, and the difference was not significant after adjusting for multiple comparisons (Table 2, Supplementary Table 1). In the analyses adjusted for maternal age and other confounders, the associations turned to null for most outcomes, and attenuated but still significant for GDM and CD. As compared to pregnant women with partners aged < 30 years, those with partners aged 40–44 years (adjusted RR [aRR] 1.45, 95% CI 1.20–1.76) and ≥ 45 years (aRR 1.44, 95% CI 1.17–1.76) had the highest risk of GDM, followed by age 35–39 years (aRR 1.37, 95% CI 1.14–1.64) and 30–34 years (aRR 1.31, 95% CI 1.10–1.56). The risk of CD was highest in women with partners aged ≥ 45 years (aRR 1.33, 95% CI 1.16–1.52), followed by age 40–44 years (aRR 1.26, 95% CI 1.11–1.43), 35–39 years (aRR 1.27, 95% CI 1.12–1.42), and 30–34 years (aRR 1.17, 95% CI 1.04–1.31). In addition, women with partners aged 40–44 years were also had higher risks of PP (aRR 1.49, 95% CI 1.01–2.18) and PPH (aRR 1.48, 95% CI 1.01–2.17), as compared with those with partners aged < 30 years.
After accounting for multiple comparisons in unadjusted analyses, older paternal age was associated with increased risks of adverse offspring outcomes except for SGA (Table 3, Supplementary Table 1). In analyses adjusted for maternal age and other confounders, the associations turned to null for most outcomes, and attenuated but still significant for PTB and macrosomia (Table 3). As compare to neonates born to fathers aged < 30 years, those born to fathers aged 30–34 years (aRR 1.32, 95% CI 1.00–1.74]) and 40–44 years (aRR 1.36, 95% CI 1.01–1.84) had a greater risk of PTB; and neonates born to fathers aged 35–39 years (aRR 1.31, 95% CI 1.05–1.63), 40–44 years (aRR 1.28, 95% CI 1.02–1.61), ≥ 45 years (aRR 1.31, 95% CI 1.01–1.68) had a greater risk of macrosomia.
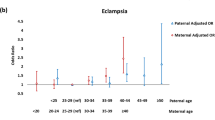
When joint effect of paternal and maternal age was assessed, the highest risks of GDM, CD, PTB, and macrosomia were observed in younger paternal age combined with older maternal age (Table 4), despite no statistical interaction between the associations related to paternal and maternal age (Pinteraction > 0.05) (Supplementary Table 2). For example, the highest risks of GDM (aRR 2.89, 95% CI 1.18–7.08) and CD (aRR 2.53, 95% CI 1.45–4.42) were observed in pregnant women aged ≥ 40 years and with partners aged < 30 years, the highest risk of PTB (aRR 2.28, 95% CI 1.15–4.52) in pregnant women aged ≥ 40 years and with partners aged 30–34 years, and the highest risk of macrosomia (aRR 1.51, 95% CI 1.12–2.04) in women aged ≥ 40 years and with partners aged 35–39 years, as compared with women aged < 35 years and with partners aged < 30 years.
Sensitivity analyses by using multiply imputed missing values for covariates, by excluding women who conceived with ART, or by using ordinal regression models showed similar results (Supplementary Tables 3–11).
Analysis of paternal age as a continuous variable revealed inverted J-shaped relationships with GDM, PP, and CD, linear relationship with PAS, and no relationship with other outcomes (Fig. 2). The predicted probabilities of GDM and PP increased rapidly with paternal age up to thresholds of 38.3 years and 36.4 years then plateaued, and the probabilities of CD increased rapidly until 40.3 years, then decelerated.
Relationships between paternal age and predicted probabilities of adverse outcomes. Predicted probabilities were transformed from the adjusted odds, which were calculated using multivariable logistic regression models with restricted cubic spline, adjustment for paternal factors including occupation, smoking and alcohol consumption, and maternal factors including delivery year, age, ethnicity, education, occupation, annual household income, gestational age at enrolment, pre-pregnancy BMI, smoking and alcohol consumption within 6 months before pregnancy, parity, and method of conception. Dark gray lines indicate predicted probabilities, and the gray bands represent 95% CIs
4 Discussion
This multicenter prospective cohort analysis with 16,114 deliveries showed that older paternal age is associated with increased risks of both maternal and offspring outcomes including GDM, CD, PTB and macrosomia, independently from maternal age and other confounders. However, when taking maternal age into consideration, these risks seem particular high at younger paternal and older maternal age, despite no statistical interaction effect between paternal and maternal age. A critical finding was that there is an inverted J-shaped association of paternal age with risks of GDM, PP and CD, with inflection points around 36–40 years.
Our findings support a large body of literature examining increased risks of some maternal and offspring outcomes following older paternal age, with the highest risks in the oldest ages [6, 9, 22, 23]. A large cohort study using data from 40,529,905 births in the US showed that pregnant women had an increased risk of 16–34% for GDM when their partners aged ≥ 35 years as compared with those partners aged 25–34 years [6]. In our study, the risks of GDM increased by 31–45% in older partner groups as compared with partners aged < 30 years.
Our findings are consistent with previous studies based on a registry of birth data which reported that advancing paternal age was associated with higher risk of CD. A study of 12,589,415 births in the US found that the risks of CD were 24–49% higher in pregnant women with partners aged ≥ 30 years compared with those partners aged 20–29 years [23]. Another study including 15,218 births of nulliparous singleton pregnancies in Lebanon showed that the risk increased by 10–40% in pregnant women with partners aged ≥ 30 years compared with those partners aged < 30 years [22]. In our study, the risks of CD increased by 17–33% in pregnant women with partners aged ≥ 30 years compared with partners aged < 30 years.
Our findings on PTB are in line with several large cohort studies from different nations [6, 24, 25]. For example, a retrospective cohort study in the US showed infants born to fathers aged ≥ 35 years had 6–25% higher risks of preterm as compared with those born to fathers aged 25–34 years [6]. In our study, the risks of PTB increased by 28–36% in infants born to fathers aged ≥ 30 years compared with those born to fathers aged < 30 years.
Studies of paternal age and birth weight showed diverse results [6, 26, 27]. In our study, the risks of macrosomia increased by 28–31% in infants born to fathers aged ≥ 35 years compared with those born to fathers aged < 30 years, similar to the findings from a Korean study [26]. However, a negative relationship between paternal age and birth weight was reported in a US study [26], and no significant association between paternal age and macrosomia was observed in a Turkish study [27].
Studies regarding other maternal complications such as PP and PPH were limited. A retrospective cohort study in the US showed that the incidence of PP increased with increasing partners’ age [9]. In our study, the risks of PP and PPH increased by 48% − 49% in pregnant women with partners aged 40–44 years as compared with partners aged < 30 years. Some studies reported that older paternal age was associated with increased risk of congenital defects [5, 28], which was not observed in our study.
Of note, our study revealed inverted J-shaped associations between paternal age and risks of GDM, PP and CD, with apexes at 36–40 years, thereafter the risks started to plateau or decelerate. These findings indicated that 36–40 years might be the thresholds to define advanced paternal age.
A potential explanation for our findings is the epigenetic link between the aging paternal genome and placental development [29]. RNA sequencing of trophoblast tissues demonstrated that paternal gene expression has a predominant influence on the process of placentation [30]. Male aging-related epigenetic changes (e.g., DNA methylation, chromosomal abnormalities, increased oxidative stress) that occur within spermatocytes lead to enlargement of placenta [31, 32], which was associated with increased risks for adverse maternal outcomes, such as GDM and CD[33, 34]. However, on the other hand, a larger placenta was associated with a greater birthweight and thus a higher risk of macrosomia[35]. Male aging-related epigenetic changes could also result in cell senescence, affect decidua attachment to the placenta, and then increase preterm risk [36, 37]. Additionally, the number of mutations increased with paternal age, partially contributing to the increased preterm risk [38].
Interesting findings were observed in the joint association of paternal and maternal age with adverse perinatal outcomes. We found that pregnancies with younger paternal age combining with older maternal age had greater risks of adverse outcomes including GDM, CD, and PTB. The joint effects of younger paternal and older maternal age could be due to economic and psychological disadvantages that pregnant women suffer from families with younger male partners [39]. However, we have to admit that we did not observe the statistical interaction effect between paternal and maternal age. Further research is needed to determine their joint effects on perinatal outcomes.
Our study has strengths. First, this is the largest multicenter prospective cohort study to date examining adverse outcomes in mothers and offspring in the context of increasing paternal and maternal age in China. Second, this is the first study assessing whether clinical threshold identifying advanced paternal age exists. Third, this study prospectively collected data including parental baseline characteristics, maternal sociodemographic characteristics, medical conditions of prior or current pregnancy, which increased the internal validity of our estimates.
Our study also has several limitations. First, our study population was overwhelmingly recruited from public referral hospitals where women are more likely to be complicated pregnancy, possibly leading to overestimated effects of older paternal age on adverse outcomes. Second, due to insufficient sample size for < 25 and > 50 years paternal age groups, their associations with perinatal outcomes could not be reliably estimated. Third, this study had limited statistical power to detect the differences in risks of some outcomes across paternal age groups, especially for the 30–34 group. Fourth, the unmeasured paternal disease history might introduce potential bias into the associations, and confounding effect of maternal age might not fully adjust. Finally, caution is needed when generalizing the threshold of paternal age derived from this study which warrant to be verified using data from different countries.
5 Conclusions
Our findings indicated that older paternal age is independently associated with greater risks of GDM, CD, PTB, and macrosomia, and the risks seem particularly pronounced at pregnancies with younger paternal but older maternal age. An inverted J-shaped association of paternal age with risks of GDM, PP and CD was observed, with the inflection points around 36–40 years. Preconception counseling guidelines might need to be updated to warn potential risks associated with delaying fatherhood, particularly given the still increasing paternal age. Future studies focusing on the health effects of extremely younger or extremely older paternal age are warranted.
Availability of Data and Materials
Data in this study are not publicly available for ethical and legal reasons. Requests for data should be directed to the corresponding author.
Abbreviations
- aRR:
-
Adjusted relative risk
- 95% CI:
-
95% Confidence interval
- UNIHOPE:
-
University Hospital Advanced Age Pregnant
- BMI:
-
Body mass index
- GDM:
-
Gestational diabetes mellitus
- HDP:
-
Hypertensive disorders of pregnancy
- PAS:
-
Placenta accreta spectrum disorders
- CD:
-
Cesarean delivery
- PPH:
-
Postpartum hemorrhage
- LGA:
-
Large-for-gestational-age
- SGA:
-
Small-for-gestational-age
- RERI:
-
Relative excess risk due to interaction
References
Office of National Statistics. Births by parents’ characteristics. 2021 https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/livebirths/datasets/birthsbyparentscharacteristics. Accessed 1 July 2023.
Martin JA, Hamilton BE, Osterman MJ, Driscoll AK, Mathews T. Births: final data for 2015. Natl Vital Stat Rep. 2017;66:1–65.
Office of the Leading Group of the State Council for the Seven National Population Census. China Population Census Yearbook. Beijing: China Statistics Press; 2020. p. 2020.
Statista. Estimated median age of Americans at their first wedding in the United States from 1998 to 2021, by sex. 2022 https://www.statista.com/statistics/371933/median-age-of-us-americans-at-their-first-wedding/. Accessed 1 July 2023.
Joinau-Zoulovits F, Bertille N, Cohen JF, Khoshnood B. Association between advanced paternal age and congenital heart defects: a systematic review and meta-analysis. Hum Reprod. 2020;35:2113–23.
Khandwala YS, Baker VL, Shaw GM, Stevenson DK, Lu Y, Eisenberg ML. Association of paternal age with perinatal outcomes between 2007 and 2016 in the United States: population based cohort study. BMJ. 2018;363: k4372.
Gao Y, Yu YF, Xiao JY, Luo JJ, Zhang YW, Tian Y, et al. Association of grandparental and parental age at childbirth with autism spectrum disorder in children. JAMA Netw Open. 2020;3: e202868.
Harlap S, Paltiel O, Deutsch L, Knaanie A, Masalha S, Tiram E, et al. Paternal age and preeclampsia. Epidemiology. 2002;13:660–7.
Alio AP, Salihu HM, McIntosh C, August EM, Weldeselasse H, Sanchez E, et al. The effect of paternal age on fetal birth outcomes. Am J Mens Health. 2012;6:427–35.
Sheen JJ, Wright JD, Goffman D, Kern-Goldberger AR, Booker W, Siddiq Z, et al. Maternal age and risk for adverse outcomes. Am J Obstet Gynecol. 2018;219(390):e1–15.
Tough SC, Faber AJ, Svenson LW, Johnston DW. Is paternal age associated with an increased risk of low birthweight, preterm delivery, and multiple birth? Can J Public Health. 2003;94:88–92.
Ortiz C, Rondeau NU, Moore LE, Mulla ZD. Parental age and the risk of gestational hypertension and preeclampsia. South Med J. 2018;111:544–8.
Peking University. University Hospital Advanced Age Pregnant Cohort (UNIHOPE). 2017 https://clinicaltrials.gov/ct2/show/NCT03220750. Accessed 18 July 2023.
Committee ADAPP. Classification and diagnosis of diabetes: standards of medical care in diabetes—2022. Diabetes Care. 2021;45:S17–38.
Erez O, Romero R, Jung EJ, Chaemsaithong P, Bosco M, Suksai M, et al. Preeclampsia and eclampsia: the conceptual evolution of a syndrome. Am J Obstet Gynecol. 2022;226:S786–803.
Einerson BD, Gilner JB, Zuckerwise LC. Placenta accreta spectrum. Obstet Gynecol. 2023;142:31–50.
Bulletins-Obstetrics C. Practice bulletin no. 183: Postpartum hemorrhage. Obstet Gynecol. 2017;130:e168–86.
The Coordinating Study Group of Nine Cities on the Physical Growth and Development of Children. Growth standard curves of birth weight, length and head circumference of Chinese newborns of different gestation. Chin J Pediatric. 2020;58:738–46.
Frederiksen LE, Ernst A, Brix N, Braskhoj Lauridsen LL, Roos L, Ramlau-Hansen CH, et al. Risk of adverse pregnancy outcomes at advanced maternal age. Obstet Gynecol. 2018;131:457–63.
Correia K, Williams PL. Estimating the relative excess risk due to interaction in clustered-data settings. Am J Epidemiol. 2018;187:2470–80.
Liu C, Zu C, Meng Q, Li R, Zhang Y, He P, et al. Inflection points in blood pressure trajectories preceding hypertension onset in different age groups. J Am Heart Assoc. 2023;12: e028472.
El Rafei R, Ghandour L, Assaf G, Charafeddine L, Al Bizri A, Alameh M, et al. Children born to mothers in their 20s and fathers in their 40s: evidence for an increased low birth weight and Cesarean Section deliveries in Lebanon. Ann Epidemiol. 2018;28:368–71.
Faro R, Santolaya-Forgas J, Canterino JC, Oyelese Y, Ananth CV. Paternal age and risk for cesarean delivery. J Matern Fetal Neonatal Med. 2012;25:2713–6.
Astolfi P, De Pasquale A, Zonta LA. Paternal age and preterm birth in Italy, 1990 to 1998. Epidemiology. 2006;17:218–21.
Goisis A, Remes H, Barclay K, Martikainen P, Myrskyla M. Paternal age and the risk of low birth weight and preterm delivery: a Finnish register-based study. J Epidemiol Community Health. 2018;72:1104–9.
Chung YH, Hwang IS, Jung G, Ko HS. Advanced parental age is an independent risk factor for term low birth weight and macrosomia. Medicine. 2022;101: e29846.
Donma MM. Macrosomia, top of the iceberg: the charm of underlying factors. Pediatr Int. 2011;53:78–84.
Oldereid NB, Wennerholm UB, Pinborg A, Loft A, Laivuori H, Petzold M, et al. The effect of paternal factors on perinatal and paediatric outcomes: a systematic review and meta-analysis. Hum Reprod Update. 2018;24:320–89.
Parks JC, Tignanelli MD, McCubbin NI, McCallie BR, Schoolcraft WB, Katz-Jaffe M. Advanced paternal age directly impacts placental epigenetic mechanisms. Fertil Steril. 2017;108:E24–5.
Wang X, Miller DC, Harman R, Antczak DF, Clark AG. Paternally expressed genes predominate in the placenta. P Natl Acad Sci USA. 2013;110:10705–10.
Vincenz C, Lovett JL, Wu W, Shedden K, Strassmann BI. Loss of imprinting in human placentas is widespread, coordinated, and predicts birth phenotypes. Mol Biol Evol. 2019;37:429–41.
Matoba S, Nakamuta S, Miura K, Hirose M, Shiura H, Kohda T, et al. Paternal knockout of Slc38a4/SNAT4 causes placental hypoplasia associated with intrauterine growth restriction in mice. P Natl Acad Sci USA. 2019;116:21047–53.
Madhuri K, Jyothi I. A study on placental morphology in gestational diabetes. J Evid Based Med Healthc. 2017;4:71–5.
Burkhardt T, Schaffer L, Schneider C, Zimmermann R, Kurmanavicius J. Reference values for the weight of freshly delivered term placentas and for placental weight-birth weight ratios. Eur J Obstet Gynecol Reprod Biol. 2006;128:248–52.
Strom-Roum EM, Haavaldsen C, Tanbo TG, Eskild A. Paternal age, placental weight and placental to birthweight ratio: a population-based study of 590,835 pregnancies. Hum Reprod. 2013;28:3126–33.
Cha JM, Aronoff DM. A role for cellular senescence in birth timing. Cell Cycle. 2017;16:2023–31.
Dutta EH, Behnia F, Boldogh I, Saade GR, Taylor BD, Kacerovsky M, et al. Oxidative stress damage-associated molecular signaling pathways differentiate spontaneous preterm birth and preterm premature rupture of the membranes. Mol Hum Reprod. 2016;22:143–57.
Kong A, Frigge ML, Masson G, Besenbacher S, Sulem P, Magnusson G, et al. Rate of de novo mutations and the importance of father’s age to disease risk. Nature. 2012;488:471–5.
Merikangas AK, Calkins ME, Bilker WB, Moore TM, Gur RC, Gur RE. Parental age and offspring psychopathology in the Philadelphia Neurodevelopmental Cohort. J Am Acad Child Adolesc Psychiatry. 2017;56:391–400.
Acknowledgements
We are grateful to all health care workers who contributed to the data collection and the participants who supplied the data from the West China Second University Hospital, The Third Affiliated Hospital of Guangzhou Medical University, Shengjing Hospital, First Affiliated Hospital of Chongqing Medical University, Tongji Hospital, Obstetrics & Gynecology Hospital of Fudan University, Peking University Third Hospital, Peking University First Hospital.
Funding
This study was supported by the National Key Research and Development Program of China (2021YFC270150001), the Clinical Projects of Peking University Third Hospital (BYSYZD2022008), the Capital’s Funds for Health Improvement and Research (2022-2G-4099), and the Opening fund of NHC Key Laboratory of Reproductive Health.
Author information
Authors and Affiliations
Contributions
SHY and YBZ led the conceptualization, methodology design, and formal analysis, validation of the results, and contributed to writing and editing the manuscript. CZ managed data curation and drafted parts of the manuscript. JY and PBY were responsible for data curation and project supervision. YYZ, HBQ and YW were involved in the project’s conceptualization, supervision, administration, and funding acquisition. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Ethics Approval and Consent to Participate
This study was approved by the Institutional Review Board of Peking University Third Hospital (IRB00006761-2016145). All participants provided written informed consents.
Consent for Publication
The participant has consented to the submission of their data to the journal.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yin, S., Zhou, Y., Zhao, C. et al. Association of Paternal Age Alone and Combined with Maternal Age with Perinatal Outcomes: A Prospective Multicenter Cohort Study in China. J Epidemiol Glob Health 14, 120–130 (2024). https://doi.org/10.1007/s44197-023-00175-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44197-023-00175-4