Abstract
Background and Aim
The impact of multiple risk factors on COVID-19 mortality has been previously reported in multiple systematic reviews and meta-analyses. The aim of this review is to provide a comprehensive update on the association between hypertension (HTN) and mortality in patients with COVID-19.
Methods
A systematic review and meta-analysis were performed and followed the Preferred Reporting Items for Systematic Reviews (PRISMA) guidelines. A search was achieved using PubMed, Scopus, and Cochrane Databases for research publications on hypertension, COVID-19, and mortality published between December 2019 and August 2022.
Results
A total of 23 observational studies involving 611,522 patients from 5 countries (China, Korea, the UK, Australia, and the USA) were included in our study. The confirmed number of COVID-19 with HTN cases in each study ranged from 5 to 9964. The mortality ranged from 0.17% to 31% in different studies. Pooled results show that the mortality rate of COVID-19 among the included studies ranges from a minimum of 0.39 (95% CI 0.13–1.12) to a maximum of 5.74 (95% CI 3.77–8.74). Out of the 611,522 patients, 3119 died which resulted in an overall mortality prevalence of 0.5%. Subgroup analyses indicated that patients with COVID-19 who have hypertension and male patients had slightly less risk of mortality than female patients [the percentage of men > 50%; OR 1.33: 95% CI (1.01, 1.76); the percentage of men ≤ 50%: OR 2.26; and 95% CI (1.15, 4.48)]. Meta-regression analysis results also showed a statistically significant association between hypertension and COVID-19 mortality.
Conclusion
This systematic review and meta-analysis suggest that hypertension may not be the only risk factor associated with the increased mortality rate during the COVID-19 pandemic. In addition, a combination of other comorbidities and old age appears to increase the risk of mortality from COVID-19.
Graphical Abstract

The impact of hypertension on mortality rate among COVID-19 patients
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Since November 2019, the world has been pushed into a very challenging era due to COVID-19 pandemic [1]. The disease course of people infected with COVID-19 varies from asymptomatic to mild, moderate or severe symptoms, sometimes requiring admission to intensive care units. Some patients may develop severe symptoms led to complications such as pulmonary failure, cytokine storm, and multi-systems failure, eventually contributing to their death. Many conducted studies reveal that there are several factors predisposing COVID-19 patients to the stage of severe infection and death. Among such various risk factors, are older age, male vs. female, and those with various comorbidities [2]. Through the literature, it is evident that arterial hypertension disease is a risk factor that leads to a high risk of morbidity and mortality in patients with COVID-19 [3].
Hypertensive patients are at a higher risk of acquiring COVID-19 infection and experiencing various complications. However, the exact cause of this relationship is still unclear. Several possible reasons have been suggested, including the presence of cardiac damage due to long-standing hypertension, the potential interaction between COVID-19 and widely used medications for hypertension treatment, and the higher incidence of hypertension in the elderly population.
As several studies have been reported, older people are more prone to acquire severe COVID-19 infections and have a higher mortality rate [4]. Furthermore, it has been suggested that hypertension can lead to end-organ damage through physiological changes in the cardiac system such as fibrotic changes in heart muscles and hypertrophy of the left ventricle. This may increase the vulnerability of hypertensive patients’ hearts to COVID-19 [5].
In 2020, Wrapp et al. proposed that COVID-19 led to lung damage and failure as a result of its binding to angiotensin-converting enzyme 2 (ACE2) in pulmonary alveoli via their superficial spike proteins and consequently, lower levels of ACE2 will be obtained [6]. Thus, decreased amounts of ACE2 may result in elevated angiotensin II levels [1,2,3,4,5,6,7]. As angiotensin II is considered an essential factor in the renin–angiotensin–aldosterone system (RAAS) function. Elevated levels of angiotensin II can lead to vasoconstriction, sodium retention, free radical damage, inflammation, and fibrosis, which are known by their role to develop hypertension [7, 8]. The above studies were done at different times during the pandemic and on different sample sizes, thus resulting in a diversity of outcomes in hypertensive patients.
Herein, we present a systematic review and meta-analysis of the available literature to analyze the mortality rate of COVID-19 in hypertensive patients. Our aim is to provide the readers with the necessary information to predict the potential outcomes of the disease and assist in developing management plans.
2 Methods
This meta-analysis was performed following the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines [9].
2.1 Search Strategy
A comprehensive search was performed in PubMed, Cochrane, and Scopus databases published up to Jan 1st, 2019, and Feb 1st, 2022 using the terms COVID-19 OR SARS-CoV-2, Mortality OR Death AND Hypertension OR Hypertensive patients. We focused on published prospective, retrospective, cross-sectional, case–control, and cross-sectional keywords used for the Medical Subject Heading [MeSH] search included: (“SARS-CoV-2” [MeSH]) or “COVID-19” [MeSH]) or “coronavirus disease 2019” [MeSH]) “nCoV-2019” [MeSH]) or “coronavirus”” [MeSH]) and “Hypertension” [MeSH]) or “HTN” [MeSH]) and “Mortality” [MeSH]. Research, and preprints papers, that have been accepted for publication were also taken into consideration because there is currently a lack of evidence.
2.2 Eligibility Criteria and Study Selection
The following criteria were used to determine which studies will be included in this review; (a) adult patients greater than 18 years; (b) hypertension as a comorbidity; (c) who was proven infected with the COVID-19 virus; (d) studies reporting mortality rates in these patients either prospective, retrospective, case–control or cross-sectional. The criteria included the above with the main interest in mortality in patients with hypertension, (e) English report publication. These were the exclusion criteria: (a) duplicate reports (including same patients’ information); (b) insufficient data; (c) reviews, and reports.
Three authors AA, DMS, and HA independently evaluated complete texts of articles and filtered them by the inclusion criteria. Where there were disagreements, discussions were made with senior authors ARA and RMZ until a consensus was established.
2.3 Data Extraction
Three authors extracted variables from the information provided (first name of the author, study design, publication year, sample size, country, age, sex distribution, etc.) and according to the main stratification variable, author, country, data source, mean age, age range, study timeframe, baseline population group, total sample, mortality rate, and others.
2.4 Statistical Analysis
Statistical analysis was done using STATA software version 17 and used the odds ratio (OR) or with a 95% confidence interval (CI) to estimate the correlation between mortality in patients with COVID-19 and hypertension. Cochran’s Q test was used to determine whether there was heterogeneity in effect sizes; a significant Q value suggests that there is heterogeneity rather than homogeneity. Using the I2 statistic, it was assessed what percentage of the overall variation may be attributed to study heterogeneity [10]. Funnel plots with the Egger regression test were used for assessing publication bias [11]. To graphically display the effect estimates from the included research, we used forest plots. Statistical significance was defined as p 0.05 at both ends.
2.5 Ethics
The protocol for this systematic review was registered in the International Prospective Register of Systematic Reviews (PROSPERO) with unique No. of CRD42022358448.
3 Result
3.1 Study Selection
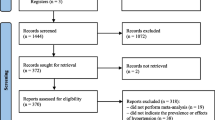
There were 203 studies found in the literature review. Out of them, 180 were excluded due to inclusion criteria not being met (wrong exposure, and wrong outcome). The remaining 23 were incorporated into our research study (Fig. 1).
3.2 Assessment of Risk of Bias
Included studies were evaluated by the authors for external and internal validity using the bias assessment in incidence and prevalence studies [12]. The assessment of the risk of bias was conducted for all 23 papers included in the quantitative analysis. The result is reported in Table 1. From the 23 studies, 1 was found of moderate risk of bias, and the remaining 22 were found of low risk of bias.
3.3 The study Included Characteristics
A total of 23 studies (18 were retrospective, 2 were observational, 1 was cross-section, 1 was a nested case–control, and 1 was prospective) involving 6,11,522 patients from 4 countries (14 from china, 1 from Korea, 3 from the UK, 1 from Australia, and 4 from the USA) were included in our study. The studies were published from 2020 to 2021(Table 2). The confirmed number of COVID-19 with HTN cases in each study ranged from 5 to 9964. The mortality ranged from 0.17% to 31% in different studies.
3.4 Characteristics of the Included Patients
The characteristics of the studies included in the analysis are summarized in Table 2. A total of 6,11,522 patients were included, with males representing 50.7% of the study population, resulting is a male-to-female ratio of approximately 1.1:1. The age range of the patients was 33–81 years. Of the total 23 studies that included severity as part of the composite endpoint, the reasons were defined as follows: pre-defined criteria (11 studies); ICU requirement (7 studies); ventilation requirement (4 studies); ARDS (1 study).
3.5 Hypertension with COVID-19 Mortality
Patients who had both COVID-19 and hypertension were found to have an increased risk of mortality to those who only had COVID-19. The odds ratio (OR) was 1.28 with a 95% confidence interval (CI) of 1.20–1.39. There were higher heterogeneity in the studies, with a Q value of 105.93 p < 0.001, and I-squared (I2) value of 84% (Fig. 2). From this plot, the mortality rate in the included studies ranged from a minimum of 0.39 (95% CI 0.13–1.12) [26] to a maximum of 5.74 (95% CI 3.77–8.74) [36]. Out of the total of 6,11,522 patients, 3119 died, resulting in an overall mortality prevalence of 0.5%.
The results of subgroup analyses suggest that male patients with hypertension with COVID-19 had a slightly lower risk of mortality than female patients. This was observed in patients where the percentage of men was greater than 50% (OR 1.33; 95% CI 1.01–1.76) and in patients where the percentage of men was less than or equal to 50% (OR 2.26; 95% CI 1.15–4.48) (Table 3). In terms of geography, China had a significantly higher mortality rate [OR 2.07; 95% CI (1.22, 3.50)] compared to other countries [OR 1.52; 95% CI (1.07, 1.25)]. Meta-regression analysis also showed a significant impact of countries on the association between hypertension and mortality in COVID-19 patients (β − 0.265; p = 0:018). However, studies with a sample size of ≤ 1000 reported a stronger association between hypertension and COVID-19 mortality [OR 1.78; 95% CI (1.10, 2.87)] compared to studies with a sample size of > 1000 [OR 1.26; 95% CI (0.95, 1.69)].
3.6 Publication Bias
No publication bias was detected in the current meta-analysis, although slight asymmetries were observed in the funnel plots (Fig. 3); we used Egger’s linear regression test to see the publication bias β − 0.02; (p = 0.980) which is not statistically significant.
4 Discussion
Since the emergence of COVID-19 as a pandemic, there has been an increased prevalence of cases, which has led to a rise in mortality rates among patients with non-communicable disease. During the COVID-19 pandemic, many countries have recommended that people stay at home, and hospital services have also been limited with a primary focus on COVID-19 patients and emergency cases to limit exposure to the virus and its spread. As a result, there has been a decrease in care for non-communicable disease patients who have been diagnosed with hypertension. This change in level of care may lead to an increase in the mortality rate among these patients.
Studies have indicated that COVID-19 infections have a greater impact on older males with comorbidities, leading to increased mortality rates in this group [37, 38]. It is interesting to note that MERS and SARS infections have been reported to be more prevalence in males than females [39,40,41]. This may be due to differences in the types and levels of sex hormones between the genders, which could increase the susceptibility to COVID-19 infection. However, our analysis revealed that male patients had a slightly lower risk of mortality compared to female patients. Several studies have shown that individuals with high blood pressure are at a higher risk of severe infection and death from COVID-19 than healthy individuals [13, 40, 42, 43]. In addition, based on the literature, there are other risk factors that increase COVID-19 mortality, such as patients who have been diagnosed with more than one non-communicable disease; including such as diabetes, CVDs, respiratory disease, cancer, and others [44].
The study by Kampaniyets et al. found that younger patients (aged 18–39) had a higher risk of severe COVID-19 cases, while older patients had a lower risk [24]. Similarly, Klang et al. found that younger patients with a BMI ≥ 40 were associated with higher mortality rates [20]. The study by Gao et al. compared hypertensive patients who took antihypertensive medications to those who did not. The study found that those who did not take antihypertensive medications had an increased risk of mortality, possibly due to their ACE2 levels. In addition, the study found that there was no statistically significant difference in mortality rate, COVID-19 severity, and ventilation requirements between hypertensive patients treated with RAAS inhibitors and those treated with non-RAAS inhibitors [21]. However, Sun et al. suggested that antihypertensive drugs like ACE2 inhibitors should be used with caution in patients infected with COVID-19 [17].
4.1 Strength and Limitation
To our knowledge, this is the first systematic review and meta-analysis that quantifies the effect of hypertension on COVID-19 mortality. Also, we reviewed the hypertension prevalence among COVID-19 patients with a large sample size. We employed a rigorous review procedure and followed PRISMA principles. We employed a rigorous approach to identifying papers, extracting data, and appraising data after searching different electronic databases. We also established operational definitions for the results, separating them using simple and repeatable formulas. We also avoided using duplicate publications, which could have skewed the interpretation of the prevalence incidence values and to reduce the effect of multiple-publication bias in the study. This review has some restrictions as well. We eliminated non-English papers due to a lack of resources. Moreover, substantial heterogeneity makes a debate about whether pooling prevalence is a worthy procedure to do.
5 Conclusion
In conclusion, the meta-analysis suggests that hypertensive patients who get infected with COVID-19 have a significantly higher death probability compared to those without hypertension. However, hypertension may not be the only risk factor, and as a combination of other comorbidities and age also seem to increase the risk of mortality. The findings of the current systematic review and meta-analysis could aid hospitals in identifying high-risk patients and to reassessing their priorities for managing chronic diseases and minimize the adverse effects of future pandemics.
Data Availability Statement
All data analyzed during this study are included in this article, and further inquiries can be directed to the corresponding author.
Abbreviations
- COVID-19:
-
Coronavirus disease of 2019
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-analyses
- ACE2:
-
Angiotensin-converting enzyme 2
- RAAS:
-
Renin–angiotensin–aldosterone system
References
WHO. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). Chennai: WHO; 2020.
Xu J, Yang X, Yang L, Zou X, Wang Y, Wu Y, et al. Clinical course and predictors of 60-day mortality in 239 critically ill patients with COVID-19: a multicenter retrospective study from Wuhan, China. Crit Care. 2020;24(1):394.
Liang W, Guan W, Chen R, Wang W, Li J, Xu K, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335–7.
Kulkarni S, Jenner BL, Wilkinson I. COVID-19 and hypertension. J Renin Angiotensin Aldosterone Syst. 2020;21(2):1470320320927851.
Tadic M, Cuspidi C, Grassi G, Mancia G. COVID-19 and arterial hypertension: hypothesis or evidence? J Clin Hypertens (Greenwich). 2020;22(7):1120–6.
Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh CL, Abiona O, et al. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367(6483):1260–3.
South AM, Diz DI, Chappell MC. COVID-19, ACE2, and the cardiovascular consequences. Am J Physiol Heart Circ Physiol. 2020;318(5):H1084–90.
Al-Qudimat AR, Al Darwish MB, Elaarag M, Al-Zoubi RM, Rejeb MA, Ojha LK, et al. COVID-19 effect on patients with noncommunicable diseases: a narrative review. Health Sci Rep. 2023;6(1): e995.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Comparison of two methods to detect publication bias in meta-analysis. JAMA. 2006;295(6):676–80.
Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934–9.
Huang S, Wang J, Liu F, Liu J, Cao G, Yang C, et al. COVID-19 patients with hypertension have more severe disease: a multicenter retrospective observational study. Hypertens Res. 2020;43(8):824–31.
Yan X, Li F, Wang X, Yan J, Zhu F, Tang S, et al. Neutrophil to lymphocyte ratio as prognostic and predictive factor in patients with coronavirus disease 2019: a retrospective cross-sectional study. J Med Virol. 2020;92(11):2573–81.
Yuan M, Yin W, Tao Z, Tan W, Hu Y. Association of radiologic findings with mortality of patients infected with 2019 novel coronavirus in Wuhan, China. PLoS ONE. 2020;15(3): e0230548.
Fu L, Fei J, Xiang H-X, Xiang Y, Tan Z-X, Li M-D, et al. Influence factors of death risk among COVID-19 patients in Wuhan, China: a hospital-based case-cohort study. medRxiv. 2020:2020.03.13.20035329.
Sun H, Ning R, Tao Y, Yu C, Deng X, Zhao C, et al. Risk factors for mortality in 244 older adults with COVID-19 in Wuhan, China: a retrospective study. J Am Geriatr Soc. 2020;68(6):E19-e23.
Hui DS, Azhar EI, Madani TA, Ntoumi F, Kock R, Dar O, et al. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health—the latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis. 2020;91:264–6.
Shi S, Qin M, Cai Y, Liu T, Shen B, Yang F, et al. Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019. Eur Heart J. 2020;41(22):2070–9.
Klang E, Kassim G, Soffer S, Freeman R, Levin MA, Reich DL. Severe obesity as an independent risk factor for COVID-19 mortality in hospitalized patients younger than 50. Obesity (Silver Spring). 2020;28(9):1595–9.
Gao C, Cai Y, Zhang K, Zhou L, Zhang Y, Zhang X, et al. Association of hypertension and antihypertensive treatment with COVID-19 mortality: a retrospective observational study. Eur Heart J. 2020;41(22):2058–66.
Marjot T, Moon AM, Cook JA, Abd-Elsalam S, Aloman C, Armstrong MJ, et al. Outcomes following SARS-CoV-2 infection in patients with chronic liver disease: an international registry study. J Hepatol. 2021;74(3):567–77.
Joy M, Hobbs FR, Bernal JL, Sherlock J, Amirthalingam G, McGagh D, et al. Excess mortality in the first COVID pandemic peak: cross-sectional analyses of the impact of age, sex, ethnicity, household size, and long-term conditions in people of known SARS-CoV-2 status in England. Br J Gen Pract. 2020;70(701):e890–8.
Kompaniyets L, Pennington AF, Goodman AB, Rosenblum HG, Belay B, Ko JY, et al. Underlying medical conditions and severe illness among 540,667 adults hospitalized with COVID-19, March 2020–March 2021. Prev Chronic Dis. 2021;18:E66.
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–62.
Meng Y, Lu W, Guo E, Liu J, Yang B, Wu P, et al. Cancer history is an independent risk factor for mortality in hospitalized COVID-19 patients: a propensity score-matched analysis. J Hematol Oncol. 2020;13(1):75.
Yu C, Lei Q, Li W, Wang X, Liu W, Fan X, et al. Clinical characteristics, associated factors, and predicting COVID-19 mortality risk: a retrospective study in Wuhan. China Am J Prev Med. 2020;59(2):168–75.
Wang K, Zuo P, Liu Y, Zhang M, Zhao X, Xie S, et al. Clinical and laboratory predictors of in-hospital mortality in patients with coronavirus disease-2019: a cohort study in Wuhan. China Clin Infect Dis. 2020;71(16):2079–88.
Chilimuri S, Sun H, Alemam A, Mantri N, Shehi E, Tejada J, et al. Predictors of mortality in adults admitted with COVID-19: retrospective cohort study from New York City. West J Emerg Med. 2020;21(4):779–84.
Lee JY, Kim HA, Huh K, Hyun M, Rhee JY, Jang S, et al. Risk factors for mortality and respiratory support in elderly patients hospitalized with COVID-19 in Korea. J Korean Med Sci. 2020;35(23): e223.
Vyas VK, Clarkson GJ, Wills M. Sulfone group as a versatile and removable directing group for asymmetric transfer hydrogenation of ketones. Angew Chem, Int Ed. 2020;59:14265–9 (Copyright (C) 2022 American Chemical Society (ACS). All Rights Reserved).
Atkins JL, Masoli JAH, Delgado J, Pilling LC, Kuo CL, Kuchel GA, et al. Preexisting comorbidities predicting COVID-19 and mortality in the UK Biobank Community Cohort. J Gerontol A Biol Sci Med Sci. 2020;75(11):2224–30.
Du RH, Liang LR, Yang CQ, Wang W, Cao TZ, Li M, et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study. Eur Respir J. 2020;55(5):2000524.
Bhatia KS, Sritharan HP, Ciofani J, Chia J, Allahwala UK, Chui K, et al. Association of hypertension with mortality in patients hospitalised with COVID-19. Open Heart. 2021;8(2):e001853.
Xu PP, Tian RH, Luo S, Zu ZY, Fan B, Wang XM, et al. Risk factors for adverse clinical outcomes with COVID-19 in China: a multicenter, retrospective, observational study. Theranostics. 2020;10(14):6372–83.
Yu S. Enabling the “made in China 2025” strategy of China’s smart logistics development. J Commer Econ. 2020;14:108–11.
Su VYF, Yang Y-H, Yang K-Y, Chou K-T, Su W-J, Chen Y-M, et al. The risk of death in 2019 novel coronavirus disease (COVID-19) in Hubei Province. SSRN Electron J 2020.
Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, Yan YQ, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan China. Allergy. 2020;75(7):1730–41.
Channappanavar R, Fett C, Mack M, Ten Eyck PP, Meyerholz DK, Perlman S. Sex-based differences in susceptibility to severe acute respiratory syndrome coronavirus infection. J Immunol. 2017;198(10):4046–53.
Badawi A, Ryoo SG. Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): a systematic review and meta-analysis. Int J Infect Dis. 2016;49:129–33.
Alwani M, Yassin A, Al-Zoubi RM, Aboumarzouk OM, Nettleship J, Kelly D, et al. Sex-based differences in severity and mortality in COVID-19. Rev Med Virol. 2021;31(6): e2223.
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–33.
Mertz D, Kim TH, Johnstone J, Lam PP, Science M, Kuster SP, et al. Populations at risk for severe or complicated influenza illness: systematic review and meta-analysis. BMJ. 2013;347: f5061.
Parohan M, Yaghoubi S, Seraji A, Javanbakht MH, Sarraf P, Djalali M. Risk factors for mortality in patients with Coronavirus disease 2019 (COVID-19) infection: a systematic review and meta-analysis of observational studies. Aging Male. 2020;23(5):1416–24.
Acknowledgements
We thank Dr. Osama Amer for assistance in data cleaning. The publication of this article was funded by Qatar National Library.
Funding
Open Access funding provided by the Qatar National Library. There was financial support for this study to declare. Open access of this article is funded by Qatar National Library.
Author information
Authors and Affiliations
Contributions
AA, DMS, and HA performed the literature search, and collected and interpreted the data. AA, DMS, HA, AT, ME, and ARA drafted the work and contributed to the writing of this manuscript. ARA and KS performed the meta-analysis. ARA and RMZ edited and drafted the final version of this manuscript. OMA reviewed the final version to be published.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Not applicable.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Al-Qudimat, A.R., Ameen, A., Sabir, D.M. et al. The Association of Hypertension with Increased Mortality Rate During the COVID-19 Pandemic: An Update with Meta-analysis. J Epidemiol Glob Health 13, 495–503 (2023). https://doi.org/10.1007/s44197-023-00130-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44197-023-00130-3