Abstract
Background
Despite significant efforts to contain the Coronavirus Disease 2019 (COVID-19) pandemic through mass vaccination, numerous nations throughout the world have recorded breakout infections. The incidence and severity of COVID-19 breakthrough infections in the United Arab Emirates (UAE) remain unknown despite extensive COVID-19 vaccine coverage. The goal of this research is to establish the characteristics of COVID-19 breakthrough infections in the UAE’s vaccinated population.
Methods
Between February and March 2022, we conducted a descriptive cross-sectional study in the UAE with 1533 participants to examine the characteristics of COVID-19 breakthrough infection among the vaccinated population.
Results
The vaccination coverage was 97.97%, and the COVID-19 breakthrough infection rate was 32.1%, requiring hospitalization in 7.7% of cases. The bulk of the 492 COVID-19 breakthrough infections reported was among young adults (67%), with the majority experiencing mild to moderate symptoms (70.7%) or remaining asymptomatic (21.5%).
Conclusions
COVID-19 breakthrough infection were reported in younger age, male sex, non-healthcare professions, vaccination with inactivated whole virus vaccine (Sinopharm), and not receiving a booster dose. Information on breakthrough infection in the UAE might influence public health decisions and motivate measures such as providing additional booster doses of the vaccines to the people.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Since the start of the coronavirus disease 2019 (COVID-19) pandemic, dedicated efforts have been put towards developing vaccines that can protect the human host, slow down the spread of the virus and end its worldwide burden. In December 2020, the United Arab Emirates (UAE) approved the use of BBIBP-CorV (Sinopharm) inactivated whole COVID-19 virus vaccine after its proven efficacy of 79% in Phase III clinical trials conducted in the country in July 2020 [1]. The effectiveness of the vaccine in preventing hospital admissions and death following infection was then found to be up to 80% and 97% respectively, as demonstrated in a large-scale retrospective study conducted in Abu Dhabi, UAE [2]. In May 2021, the Pfizer-BioNTech messenger RNA vaccine was approved for use in the UAE, based on the Food and Drug Authority’s (FDA) announced efficacy of 95% [3]. Alongside Sinopharm and Pfizer BioNTech, three more COVID-19 vaccines Moderna, Oxford/AstraZeneca, and Sputnik were also distributed among the UAE population promptly, reaching around 97.97% of fully vaccinated individuals in May 2022 [4]. COVID-19 vaccine booster doses, specifically Pfizer BioNTech and Sinopharm, were advised 6 months after the original two doses to complete the vaccination regimen and be declared fully immunized.
With this high coverage of vaccination in the UAE population which is around 10 million, the rate of hospitalization, deaths, and severity in infection has significantly dropped from a peak of 3167 diagnosed cases and 13 deaths on the 14th February 2021 to 321 cases with no deaths by the 23rd May 2022 [4]. As anticipated, while the COVID-19 vaccine was highly effective in reducing coronavirus disease, deaths, infectivity, severity, asymptomatic infections and hospital admissions [5,6,7,8], vaccine breakthrough infection started to be reported worldwide [9, 10]. A COVID-19 breakthrough infection is defined as a positive test for COVID-19 in a person at least two weeks after becoming fully vaccinated [10, 11]. A person is fully vaccinated 2 weeks after receiving all recommended doses in the primary series of their COVID-19 vaccination and a person is considered up to date with their COVID-19 vaccination if they have received all recommended doses in the primary series and one booster when eligible [12].
More than 2.8 million breakthrough infections had been reported to the Centers for Disease Control and Prevention (CDC) in the United States as of December 2021 [7]. Breakthrough cases occur because no vaccine is 100% effective and in COVID-19 the variants such as the delta and omicron were the common etiology [13,14,15]. Breakthrough infections remains a threat to the COVID-19 pandemic. Vaccinated persons who get breakthrough infections may be asymptomatic or have minor symptoms, but they can still spread the virus to the rest of the community. In addition, people do not report the majority of breakthrough cases, thus the total number of reported breakthrough cases likely represents an undercount.
Breakthrough infections, despite their small numbers, can be misinterpreted as a failure of vaccine protection in some situations; yet, in reality they actually indicate that the vaccine is working properly. Furthermore, the incidence of breakthrough infections could be on the rise due to the decline in neutralizing antibody level in the host [16].
The incidence and severity of COVID-19 breakthrough infections in the UAE remain understudied, despite the widespread vaccination of the population. We believe such data is essential to describe these infections and inform public health decisions including delivering additional vaccine doses, adjusting vaccination tactics, continuing infection control methods, and managing the COVID-19 pandemic successfully.
2 Materials and Methods
The study was performed after obtaining the necessary institutional ethics approval (REC-22-02-01). A descriptive cross-sectional study design was used in conjunction with a convenience sample strategy for all vaccinated individuals living in the UAE from February to March 2022.
A questionnaire consisting of 18 questions, divided into 3 different sections: demographics, COVID-19 vaccination, and COVID-19 breakthrough infection was administered through email and social media platforms such as WhatsApp group chats, Instagram and Twitter. The questionnaire was bilingual in English and Arabic and the questions were close-ended, in the form of single-choice and multiple-choice answers (appendix 1). A participant information sheet was presented before starting the questionnaire, and the agreement to fill out the questionnaire indicated the consent of the participants to join the study. Data was processed in python-3 using the Matplotlib-v3.3.4, pandas-v1.2.4, and statsmodels-v0.12.2 packages for analysis and interpretation. Given the categorical nature of all the variables, multivariate analyses were used to identify significant predictors. A p value of less than 0.05 was considered significant.
3 Results
3.1 Demographics
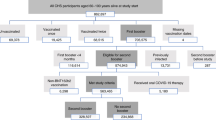
A total of 1544 individuals participated in the study of which 1533 responses were included in the analysis. Among the 1533 respondents, 863/1533 (56.3%) were males and 184/1533 (12%) reported to have comorbidities. As for the vaccination rates, 488/1533 (31.8%) of the respondents received 2 doses of the Pfizer vaccine, while 327/1533 (21.3%) received 2 doses of the Sinopharm vaccine followed by 2 booster doses of the Pfizer vaccine. Overall, 776/1533 (50.6%) of the sample were infected with COVID-19 at least once (Table 1).
3.2 COVID-19 Breakthrough Infection & Hospitalization
Of the 1533 participants, 492 (32.1%) reported having a breakthrough COVID-19 infection, of which 38 (7.7%) required hospitalization. Figure 1 shows how the participants were divided according to infection and hospitalization rates. All age groups had a breakthrough infection rate of over 25%, with the age groups 31–40 years and 41–50 years reporting the highest infection rates of 48.9% and 40.9%, respectively. The COVID-19 breakthrough infection rates among healthcare workers were 34.7% (42/121) and people with comorbidities such as diabetes, asthma, immunodeficiency and other chronic disorders was 33.5% (61/182).
Surprisingly, individuals who received three doses of Sinopharm had the highest breakthrough rate (45.6%, 77/169), with roughly one out of every two infections, becoming a breakthrough infection (Fig. 2). When compared to people who were fully vaccinated (completed primary series) or up to date (primary + booster) with the Pfizer vaccine, the rate of COVID-19 breakthrough infections among people who received Sinopharm vaccine only or two doses of Sinopharm (primary doses) and a booster with Pfizer remains relatively high, at 37% (84/227) and 36.4% (28/77), respectively (Table 1 and Fig. 2).
Of the 492 COVID-19 breakthrough infections reported, the majority were seen among young adults (67%, 329/492), male sex (55%, 269/492) and most of these cases either experienced mild to moderate symptoms (70.7%, 348/492) or remained asymptomatic (21.5%, 106/492). Mild to moderate symptoms included fever, cough, sore throat, loss of taste, smell and other constitutional symptoms such as diarrhea, fatigue and body aches, which did not require hospitalization. Despite the subtlety of the clinical presentation, virus transmission to close contacts remains high (74.6%, 367/492) (Table 2).
4 Discussion
COVID-19 breakthrough infections pose a significant concern worldwide, despite the widespread efforts at eradicating infection through vaccination. In this study, among the 1533 individuals who participated, 492 reported COVID-19 breakthrough infection. Such infections are attributed to a number of factors, ranging from the emerging COVID-19 variants to insufficient immune response to vaccination. Prior to the emergence of the Delta variant, in April and May of 2021, breakthrough cases numbered around 48,000 in the US [7]. In comparison, over 1.8 million breakthrough infections were reported during the predominance of the variant between July and November 2021. This rise in breakthrough cases may be due to the reduced effectiveness of vaccines against the Delta variant, where an effectiveness of 88% against the variant was reported with the Pfizer-BioNTech vaccine compared to an effectiveness of 93.7% against the Alpha variant [17]. In addition, the high transmissibility, high viral load, and shorter incubation period of the Delta variant may have contributed to the elevation in breakthrough cases [18].
Similarly, in the month of December 2021, as the Omicron variant was beginning to emerge worldwide, more than 900,000 breakthrough cases were reported in the US [7]. This is parallel to the rise in the number of cases in the UAE during the period of Omicron predominance, peaking at 3020 in mid-January, a sharp increase from under 100 cases the month before [19]. Surprisingly, the upsurge occurred during a period where 93.5% of the UAE’s population was fully vaccinated, where the majority of cases were likely to be breakthrough [20]. The main vaccines distributed among the UAE citizens are the Sinopharm and Pfizer-BioNTech vaccines, whose effectiveness against the Omicron variant was shown to decline. Neutralizing antibodies against the Omicron variant were only detected in up to 24% of individuals who received the primary 2 doses of the Pfizer-BioNTech vaccine in a trial study, and in another study, vaccine effectiveness dropped from 65.5% at 2 to 4 weeks to 8% at 25 weeks or more after the two doses [21, 22]. Similar findings were seen in Sinopharm-vaccinated individuals, where the levels of neutralizing antibodies against Omicron were reduced by 53% almost 26 weeks after the administration of a third shot following the primary two-dose regimen [23]. To ameliorate the burden of breakthrough infections, an mRNA-based booster vaccine was shown to remarkably raise the levels of antibodies and B and T cell responses against the variant, following administration of the primary doses of either Pfizer-BioNTech and Sinopharm BIBP [24].
In this study, 45.6% (77/169) of individuals who received two doses of Sinopharm BIBP followed by a Sinopharm CNBG booster vaccine developed a breakthrough infection, making up the greatest proportion of breakthroughs among all the vaccine regimens. While those who received two doses of Pfizer-BioNTech followed by a booster with the same Pfizer-BioNTech vaccine reported a relatively low breakthrough infection rate of 29.4% (42/143). In-between, were the heterologous vaccination, two doses of Sinophram and a Pfizer-BioNTech booster and two doses of Sinophram and two doses of Pfizer-BioNTech booster, reported breakthrough rates of 36.4% and 33.3%, respectively. Studies have indicated that mRNA vaccines, such as those made by Pfizer and Moderna, provide far better protection than those made by AstraZeneca and Janssen, which utilize a more standard viral vector formula [25] and in our case an inactivated viral vaccine such as Sinopharm BIBP. Combination of COVID-19 vaccination practice such as primary dosing with an inactivated vaccine followed by a booster dose with an mRNA vaccine has potentially increased protection against SARS-CoV-2 variants such as Omicron by augmenting the levels of specific antibodies and B and T cell responses [24] but has not eliminated the occurrence of breakthrough infections.
There has been a noticeable surge in hospital admissions due to COVID-19 infections worldwide. A rate of 5.8% of all patients with a confirmed COVID-19 infection in the United States were hospitalized [26]. In contrast, hospital admissions following a breakthrough COVID-19 infection fell dramatically below 1% as reported by the New York State Department of Health [27]. However, in this study, 38 of the 492 COVID-19 breakthrough infection cases (7.7%) required hospitalization, which is towards the higher side. Advanced age and having comorbidities were the two common factors consistently associated with patients requiring hospitalization. This is in line with a reported observation that the vast majority of the hospitalizations were in individuals aged 65 and above (69%) and having comorbidities [28]. Interestingly, in this study, the rates of breakthrough infections among individuals suffering from comorbidities and individuals without were comparable. As a result, we believe the etiology of breakthrough infections in our study is linked to the developing Omicron variant and its associated immune evasion, rather than the loss in vaccine effectiveness due to comorbidities.
In the multivariate analysis, we found that breakthrough infections were more common in younger age groups, such as 67% (25 years old) and 28% (25–50 years old), compared to 5.5% in older age groups (> 50 years old), which we attribute to young people’s social behavior, higher social contacts, and work-related contacts, which is consistent with other cohorts’ reported data [29,30,31]. Similarly, reinfections rates were higher than a single episode of breakthrough infection especially during the wave of the Omicron variant peak [32]. Another interesting observation was, despite being exposed to COVID-19 patients on a daily basis, healthcare workers were found to have a decreased chance of developing a breakthrough infection when compared to a non-healthcare worker. This could indicate that healthcare workers were better protected with higher vaccine coverage and practiced infection control measures especially at work [29, 33].
In this study, despite the fact that the majority of patients with a breakthrough infection were asymptomatic or had mild to moderate symptoms, they were able to spread the infection to close relatives and friends (74.6%). This is concerning because breakthrough infections have contributed to increased case numbers and pandemic extension at a time when vaccine effectiveness is diminishing, lockdowns, infection control measures, and social restrictions are being lifted.
The small cohort size of our study, despite vaccine coverage of nearly 97% of the UAE population, is one of the study’s potential drawbacks. The lack of antibody titer specifically the anti-S level data and its link with breakthrough infections is another limitation. It is evident that post-COVID-19 vaccination antibody titer wanes off with time and has been directly correlated with the occurrence of breakthrough infections [34]. We do have a plan to address both these limitations in a future study linking the antibody titer measurements with breakthrough infections in a bigger cohort size.
In conclusion, this study found that younger age, male sex, non-healthcare professionals, vaccination with inactivated whole virus vaccine (Sinopharm), and not obtaining a booster dose were all linked with an elevated risk of COVID-19 breakthrough infection.
Data Availability
Data will be available from the corresponding author on reasonable request.
Abbreviations
- COVID-19:
-
Coronavirus Disease 2019
- UAE:
-
United Arab Emirates
References
Suliman DM, Nawaz FA, Mohanan P, Modber MAKA, Musa MK, Musa MB, et al. UAE efforts in promoting COVID-19 vaccination and building vaccine confidence. Vaccine. 2021;39(43):6341–5.
Hosani FIA, Stanciole AE, Aden B, Timoshkin A, Najim O, Zaher WA, et al. (2021) Sinopharm’s BBIBP-CorV vaccine effectiveness on preventing hospital admission and deaths: results from a retrospective study in the Emirate of Abu Dhabi, United Arab Emirates (UAE). United Arab Emirates (UAE)
Pfizer-BioNTech COVID-19 Vaccines. Available from: https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/pfizer-biontech-covid-19-vaccines. Accessed 14 Feb 2022.
CORONAVIRUS (COVID-19) UPDATES U. Available from: https://covid19.ncema.gov.ae/en. Accessed 23 May 2022
Haas EJ, Angulo FJ, McLaughlin JM, Anis E, Singer SR, Khan F, et al. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data. Lancet. 2021;397(10287):1819–29.
Regev-Yochay G, Amit S, Bergwerk M, Lipsitch M, Leshem E, Kahn R, et al. Decreased infectivity following BNT162b2 vaccination: a prospective cohort study in Israel. Lancet Reg Health Eur. 2021;7: 100150.
Johnson AG. COVID-19 incidence and death rates among unvaccinated and fully vaccinated adults with and without booster doses during periods of Delta and Omicron variant emergence—25 US Jurisdictions, April 4–December 25, 2021. MMWR Morb Mortal Wkly Rep. 2022;71:132.
Moghadas SM, Vilches TN, Zhang K, Wells CR, Shoukat A, Singer BH, et al. The impact of vaccination on coronavirus disease 2019 (COVID-19) outbreaks in the United States. Clin Infect Dis. 2021;73(12):2257–64.
Tyagi K, Ghosh A, Nair D, Dutta K, Bhandari PS, Ansari IA, et al. Breakthrough COVID19 infections after vaccinations in healthcare and other workers in a chronic care medical facility in New Delhi, India. Diabetes Metab Syndr. 2021;15(3):1007–8.
Covid CD, Team VB, Birhane M, Bressler S, Chang G, Clark T, Dorough L, Fischer M, Watkins LF, Goldstein JM, Kugeler K. COVID-19 vaccine breakthrough infections reported to CDC—United States, January 1–April 30, 2021. Morb Mortal Wkly Rep. 2021;70(21):792.
Covid C, Team VBCI, Birhane M, Bressler S, Chang G, Clark T, et al. COVID-19 vaccine breakthrough infections reported to CDC—United States, January 1–April 30, 2021. Morb Mortal Wkly Rep. 2021;70(21):792.
Stay Up to Date with Your COVID-19 Vaccines C. Available from: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/stay-up-to-date.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fvaccines%2Ffully-vaccinated.html. Accessed 23 May 2022
Zhou R, To KK, Peng Q, Chan JM, Huang H, Yang D, Lam BH, Chuang VW, Cai JP, Liu N, Au KK. Vaccine‐breakthrough infection by the SARS‐CoV‐2 omicron variant elicits broadly cross‐reactive immune responses. Clin Transl Med. 2022;12(1).
Jolly B, John N, Bhoyar RC, Majeed N, Senthivel V, Fairoz C, et al. Genomic survey of SARS-CoV-2 vaccine breakthrough infections in healthcare workers from Kerala. India J Infect. 2021;83(2):237–79.
Kustin T, Harel N, Finkel U, Perchik S, Harari S, Tahor M, et al. Evidence for increased breakthrough rates of SARS-CoV-2 variants of concern in BNT162b2-mRNA-vaccinated individuals. Nat Med. 2021;27(8):1379–84.
Khoury DS, Cromer D, Reynaldi A, Schlub TE, Wheatley AK, Juno JA, et al. Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection. Nat Med. 2021;27(7):1205–11.
Lopez Bernal J, Andrews N, Gower C, Gallagher E, Simmons R, Thelwall S, Stowe J, Tessier E, Groves N, Dabrera G, Myers R. Effectiveness of Covid-19 vaccines against the B. 1.617. 2 (Delta) variant. N Engl J Med. 2021;385(7):585–94.
Wang Y, Chen R, Hu F, Lan Y, Yang Z, Zhan C, et al. Transmission, viral kinetics and clinical characteristics of the emergent SARS-CoV-2 Delta VOC in Guangzhou. China EClinicalMedicine. 2021;40: 101129.
Coronavirus Pandemic Country Profile U. Available from: https://ourworldindata.org/coronavirus/country/united-arab-emirates#how-many-tests-are-performed-each-day. Accessed 23 May 2022
Coronavirus (COVID-19) Vaccinations U. Available from: https://ourworldindata.org/covid-vaccinations?country=ARE. Accessed 23 May 2022
Andrews N, Stowe J, Kirsebom F, Toffa S, Rickeard T, Gallagher E, Gower C, Kall M, Groves N, O’Connell AM, Simons D. Covid-19 vaccine effectiveness against the Omicron (B. 1.1. 529) variant. N Engl J Med. 2022;386(16):1532–46.
Lu L, Mok BW, Chen LL, Chan JM, Tsang OT, Lam BH, Chuang VW, Chu AW, Chan WM, Ip JD, Chan BP. Neutralization of severe acute respiratory syndrome coronavirus 2 omicron variant by sera from BNT162b2 or CoronaVac vaccine recipients. Clin Infect Dis. 2022;75(1):e822–6.
Wang J, Deng C, Liu M, Liu Y, Li L, Huang Z, Shang L, Jiang J, Li Y, Mo R, Zhang H. Four doses of the inactivated SARS-CoV-2 vaccine redistribute humoral immune responses away from the Receptor Binding Domain. MedRxiv. 2022:2022-02.
Zuo F, Abolhassani H, Du L, Piralla A, Bertoglio F, de Campos-Mata L, Wan H, Schubert M, Cassaniti I, Wang Y, Sammartino JC. Heterologous immunization with inactivated vaccine followed by mRNA-booster elicits strong immunity against SARS-CoV-2 Omicron variant. Nat commun. 2022;13(1):2670.
Kuhlmann C, Mayer CK, Claassen M, Maponga T, Burgers WA, Keeton R, Riou C, Sutherland AD, Suliman T, Shaw ML, Preiser W. Breakthrough infections with SARS-CoV-2 omicron despite mRNA vaccine booster dose. Lancet. 2022;399(10325):625–6.
COVID Data Tracker C. Available from: https://www.covid.cdc.gov/COVID-data-tracker/#new-hospital-admissions. Accessed 23 May 2022
COVID-19 Breakthrough Data C. Available from: https://www.coronavirus.health.ny.gov/covid-19-breakthrough-data. Accessed 23 May 2022
Jercich K NtobC-ispthsnTd. Available from: https://www.healthcareitnews.com/news/nine-15-breakthrough-covid-19-infections-send-patients-hospital-says-new-truveta-data. Accessed 23 May 2022
Stouten V, Hubin P, Haarhuis F, van Loenhout JA, Billuart M, Brondeel R, et al. Incidence and risk factors of COVID-19 vaccine breakthrough infections: a prospective cohort study in Belgium. Viruses. 2022;14(4):802.
Liu C, Lee J, Ta C, Soroush A, Rogers JR, Kim JH, Natarajan K, Zucker J, Weng C. A retrospective analysis of COVID-19 mRNA vaccine breakthrough infections–risk factors and vaccine effectiveness. Medrxiv. 2021.
Uschner D, Bott M, Lagarde WH, Keating J, Tapp H, Berry AA, Seals AL, Munawar I, Schieffelin J, Yukich J, Santacatterina M. Breakthrough SARS-CoV-2 infections after vaccination in North Carolina. Vaccines. 2022;10(11):1922.
Mallapaty S. COVID reinfections surge during Omicron onslaught. Nature. 2022;10.
Würtz AM, Kinnerup MB, Pugdahl K, Schlünssen V, Vestergaard JM, Nielsen K, Cramer C, Bonde JP, Biering K, Carstensen O, Hansen KK. Healthcare workers’ SARS-CoV-2 infection rates during the second wave of the pandemic: prospective cohort study. medRxiv. 2021:2021–11.
Aldridge RW, Yavlinsky A, Nguyen V, Eyre MT, Shrotri M, Navaratnam AM, Beale S, Braithwaite I, Byrne T, Kovar J, Fragaszy E. Waning of SARS-CoV-2 antibodies targeting the Spike protein in individuals post second dose of ChAdOx1 and BNT162b2 COVID-19 vaccines and risk of breakthrough infections: analysis of the Virus Watch community cohort. MedRxiv. 2021:2021–11.
Acknowledgements
We thank the participants of the study for their generosity in providing the required information to complete the study.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation and data collection were performed by AAO, HQC, RQ and SE. Statistical analyses were performed by KAS. The first draft of the manuscript was written by NRD and HJB, all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no competing interest to declare.
Ethical Approval
The study was approved by the Research Ethics Committee of the University of Sharjah (REC-22-02-01) and written informed consent from all the participants was taken.
Consent for Publication
Informed consent was obtained from all participants.
Appendices
Appendix 1
English version
COVID-19 Breakthrough Infections in Vaccinated Population
We are a group of medical students at the University of Sharjah conducting a research project about the COVID-19 breakthrough infections in vaccinated populations.
You have been randomly selected to participate in this study and your participation is strictly voluntary. If you agree to participate, you will be asked to fill out a questionnaire that will take no more than 4–7 min of your time.
There are no risks or benefits associated with participation in this study. Your identity will remain unknown, and we assure you that your responses will be confidential and will be usedonly for research purposes.
You have the right to withdraw from the study at any time during filling out the questionnaire,but you cannot withdraw after submitting it since it will be unidentifiable.
Please note that no incentives will be given for the completion of this survey.
If you have any questions regarding this study or would like to be informed about its results,please feel free to contact our research supervisors Dr. Hiba Barqawi at hbarqawi@sharjah.ac.ae or Dr. Nihar Dash at ndash@sharjah.ac.ae.
For any ethical concerns, you may contact the Research Ethics Committee at the University ofSharjah—rec@sharjah.ac.ae.
Filling out this questionnaire indicates your agreement to participate in this study.
اﻹﺟﺎﺑﺔ اﻹﺳﺗﺑﯾﺎن ﺑﺎﻟﻠﻐﺔ اﻟﻌرﺑﯾﺔ اﺿﻐط ھن
https://forms.gle/YSX4zkX9PyS7f85A9
*Required.
COVID-19 Vaccination.





















Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dash, N.R., Barqawi, H.J., Obaideen, A.A. et al. COVID-19 Breakthrough Infection Among Vaccinated Population in the United Arab Emirates. J Epidemiol Glob Health 13, 67–90 (2023). https://doi.org/10.1007/s44197-023-00090-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44197-023-00090-8