Abstract
Background
Lebanon endured its worst economic and financial crisis in 2020–2021. To minimize the impact of COVID-19 pandemic, it is important to improve the overall COVID-19 vaccination rate. Given that vaccine hesitancy among health care workers (HCWs) affects the general population’s decision to be vaccinated, our study assessed COVID-19 vaccine acceptance among Lebanon HCWs and identified barriers, demographic differences, and the most trusted sources of COVID-19 information.
Methods
A cross-sectional study was conducted between January and May 2021 among HCWs across nine hospitals, the Orders of Physicians, Nurses, and Pharmacists in Lebanon. Descriptive statistics were performed to evaluate the COVID-19 vaccine acceptance, and univariate and multivariable to identify their predictors.
Results
Among 879 participants, 762 (86.8%) were willing to receive the COVID-19 vaccine, 52 (5.9%) refused, and 64 (7.3%) were undecided. Males (226/254; 88.9%) and those ≥ 55 years (95/100; 95%) had the highest rates of acceptance. Of the 113 who were not willing to receive the vaccine, 54.9% reported that the vaccine was not studied well enough. Participants with a previous SARS-CoV-2 infection and those who did not know if they had a previous infection (p = 0.002) were less likely to accept the vaccine compared to those with no previous infection. The most trusted COVID-19 sources of information were WHO (69.3%) and healthcare providers (68%).
Conclusion
Lebanese HCWs had a relatively high acceptance rate for COVID-19 vaccination compared to other countries. Our findings are important in informing the Lebanese health care authorities to establish programs and interventions to improve vaccine uptake among HCWs and the general population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The coronavirus disease-2019 (COVID-19) pandemic has resulted in more than 500 million confirmed cases and over 6.2 million deaths (as of May 2022) [1]. While the COVID-19 pandemic has had detrimental health, cultural, and socioeconomic effects across all countries, low- and middle-income countries (LMICs), such as Lebanon, are at greater risk of infection [2]. The first case of COVID-19 in Lebanon was confirmed on February 21st, 2020, and since then, the number of cases and deaths has significantly grown [3, 4].
Enormous international efforts have been put in the development and distribution of COVID-19 vaccines. The COVID-19 Vaccines Global Access Facility (COVAX) was launched [5], in collaboration with the World Health Organization (WHO), with a goal of administering at least two billion COVID-19 vaccine doses across LMICs by 2022 [6,7,8]. In Lebanon, the Ministry of Public Health (MOPH) launched its vaccination rollout on February 14th, 2021, starting with the Pfizer-BioNTech mRNA vaccine. An additional 1.5 million doses were reserved from Oxford-AstraZeneca to speed up the distribution of vaccines [7]. However, the success of immunization campaigns depends on acceptance of newly introduced vaccines, particularly during pandemics [9]. Vaccine hesitancy remains a pertinent issue across the general populations as well as among health care workers (HCWs), globally. Vaccine acceptance is known to vary with time and context [10]. Therefore, vaccine acceptance of a newly developed vaccines, especially as novel technology (e.g., mRNA vaccines) is being implemented, has historically been a concern [11].
Due to the limited vaccine supply across the world, priority was given to HCWs and other front-line workers to be immunized first. One of the major concerns was the level of vaccine acceptance across these HCWs [12]. An international survey on COVID-19 vaccine acceptance, conducted from June 16 to June 20, 2020, showed that at least 30% would be hesitant to take the vaccine [11]. A survey conducted in April 2020 in the United States (US) estimated refusal of COVID-19 vaccination in at least one third of the participants [13]. A national survey conducted between October and December 2020 in the Kingdom of Saudi Arabia (KSA) showed that the acceptance of COVID-19 vaccine among HCWs was around 65%, with the main reason for hesitance being fear of possible side effects [14]. In addition to several other vaccine acceptance studies [15,16,17,18,19,20], the KSA study highlighted the need to understand the factors that were likely to impact the decision of HCWs to receive the vaccine, especially with the expectation that new strains will continuously evolve and vaccine efficacy may decline—making new vaccine uptake a major contributor to herd immunity over time [10].
Many factors, including widely spread misinformation, can be important contributors, adversely affecting vaccine acceptance [12]. Because HCWs are regarded as a trusted source of information and advice to their patients and acquaintances, it is crucial to highlight their role in spreading awareness and advocating for vaccine acceptance [21]. While various findings have been disseminated regarding the COVID-19 vaccine, factors associated with vaccine refusal have not been studied well among HCWs in Lebanon. Halabi et al. reported a refusal rate of 40% among the Lebanese general population, with female gender, marriage status, and history of vaccine hesitancy being the most influencing factors [22].
Understanding the potential reasons for COVID-19 vaccine refusal among HCWs in Lebanon may help in identifying ways to overcome vaccine gaps in the health care sector and the general population, and improve strategic plans in containing the Severe Acute Respiratory Syndrome-Coronavirus-2 (SARS-CoV-2) [22]. Given the paucity of information about Lebanese HCWs’ acceptance of COVID-19 vaccines and associated demographic factors, we conducted a survey among HCWs from several Lebanese health care institutions to examine COVID-19 vaccine acceptance and identify factors leading to COVID-19 vaccine refusal.
2 Methods
2.1 Program Description and Setting
Between January and May 2021, we used selective sampling to conduct a cross-sectional survey using an electronic questionnaire via Qualtrics® (Qualtrics, Provo, UT). HCWs at nine participating hospitals across different provinces in Lebanon were invited as well as other HCWs registered in Orders of Physicians, Nurses, and Pharmacists.
The survey was distributed to HCWs by email, WhatsApp message, or Short Message Service (SMS). The eligibility requirements to participate in the study included being a HCW, 18 years or older, read English or Arabic, and have access to the Internet. Participants had the option to choose English or Arabic. E-consent was required prior to data collection. Our target population included approximately 20,000 physicians, residents, fellows, medical students, nurses (practical and registered nurses), dietitians, dentists, optometrists, psychologists, respiratory therapists, physical therapists, occupational therapists, behavioral therapists, social workers, infection control workers, pharmacists, laboratory and radiology technicians, research assistants and coordinators, and administrative personnel. Based on our previous work and published study [20], and considering the Lebanese HCW population at approximately 40,000 [23], with a vaccine acceptance of 50% and margin of error of 4% (95% CI 46–54%), we calculated a sample size of 592 individuals.
2.2 Measures and Variables
Our survey was redesigned from a previously published work conducted by Malik et al.[20], and included 20 questions (Supplementary Material). Basic demographic information, in addition to information pertaining to participants’ country of origin and religious association were collected. We asked participants to identify factors such as religious barriers, concerns about side effects, lack of trust in vaccine production, and disbelief in vaccine potency that might influence their decision when answering “No” or “Don’t know” about their willingness to receive COVID-19 vaccine once available. Lastly, HCWs were asked about their confidence in organizations and healthcare providers and reliability in media sources as it pertains to disseminating COVID-19 information, with these variables being assigned a value of either 0 or 1 (0 = Very Little/Little/Some/Don’t Know; 1 = Much/Very Much).
The Institutional Review Boards (IRB) at Yale University (IRB protocol number: 2000029237), and at American University of Beirut Medical Center (IRB protocol number: SBS-2020-0563) approved this study, in line with the Code of Ethics of the World Medical Association, the Declaration of Helsinki [24]. After we informed the subjects about the purpose of the study, E-consent was required prior to data collection. Participants were also informed that there will be no risks or direct benefits from their collaboration to this study. The participation was completely voluntary and enrolled subjects retained right to withdraw at any time throughout the study. In addition, to maintain confidentiality, the research team do not have access to their names or contact details. Data were secured on a password protected computer and will only be accessible to the research team members, after which the data will be deleted once the legal retention period expired.
2.2.1 Statistical Analysis
Collected data were coded and entered in the software Statistical Package for Social Sciences (SPSS) version 25 (SPSSTM Inc., Chicago, IL United States). Descriptive statistics were conducted to identify the sample demographic characteristics. Moreover, we calculated the frequency and percentage of responses to questions related to COVID-19 vaccine acceptance, reasons for refusal to accept a COVID-19 vaccine, reliability of media sources, and confidence in organizations and healthcare providers.
Finally, univariate analyses were conducted. The explanatory variables were first tested 1 by 1 against the dependent variable for the presence of a significant association using the binomial logistic regression. In the multivariable logistic regression model, we included variables reported in the literature to be associated with COVID-19 vaccine acceptance considering them as potential confounders, such as age, gender, religious association, and educational level [11, 14, 20, 25,26,27], and variables that showed a significant association at p ≤ 0.05 across any categories in the univariate analysis. The goodness-of-fit statistic is reported to determine if the model provides a good fit for the data (p > 0.05) [28]. The strength of association was interpreted using the adjusted odds ratio (AOR) with 95% confidence Interval (CI). A p ≤ 0.05 was considered statistically significant.
3 Results
3.1 Sample Characteristics
Among the 879 HCWs who completed the survey, the majority were Lebanese (n = 858; 97.6%), between 25 and 34 years old (n = 301; 34.2%), female (n = 619; 70.4%), Muslim (n = 423; 48.1%), had a graduate/professional degree (n = 492; 56%), and had no chronic disease (n = 708; 80.5%). Nurses (n = 385, 45.5%) accounted for the largest group among respondents. Table 1 shows the characteristics of the survey participants.
3.2 COVID-19 Vaccine Acceptance and Demographic Characteristics
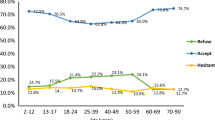
Among the 879 participants, 762 (86.8%) were willing to receive the COVID-19 vaccine, 52 (5.9%) refused, 64 (7.3%) were undecided whether to receive it or not, and 1 (0.1%) did not answer the question on whether they would take the vaccine or not (Fig. 1A). Of the 116 (13.2%) who said they would not accept a COVID-19 vaccine, 62 (53.4%) reported that the vaccine had not been studied well enough, 27 (23.3%) reported lack of trust of those developing and distributing the vaccine, 24 (20.7%) reported fear of potential side effects, and 3 (2.6%) did not answer the question related to why they would not take the vaccine (Fig. 1B). COVID-19 vaccine acceptance rates were shown to differ among the various demographic groups. Males (226/254, 88.9%), those aged 55 or older (95/100, 95%), and Lebanese (745/857, 86.9%) had the highest rates of acceptance (Table 2).
The multivariable logistic regression analysis showed that after adjusting for gender, age, religion, and education level, significant findings were seen in a couple of demographic factors (Table 3). Participants with a previous SARS-CoV-2 infection (OR: 0.47; 95% CI 0.30–0.75; p = 0.002) and those who did not know if they had a previous infection (OR: 0.24; 95% CI 0.10–0.60; p = 0.002) were less likely to accept the vaccine compared to those with no previous SARS-CoV-2 infection. No significant association was seen in the other demographic factors after adjustment.
3.3 Reliability of Media Sources and Confidence in Organizations pertaining to COVID-19 Information
Participants reported the WHO (n = 609; 69.3%), healthcare providers (n = 598; 68.0%), and health officials (n = 491; 55.9%) as the most reliable media sources of COVID-19 information. Additionally, participants reported the highest confidence in healthcare providers (n = 611 69.5%) and the WHO (n = 567; 64.5%).
3.4 Reliability of Media Sources and Confidence in Organizations and Healthcare Providers pertaining to COVID-19 Information across the COVID-19 Vaccine Acceptance Landscape
Participants who would take the COVID-19 vaccine (n = 762; 86.8%) reported the WHO (n = 609; 86.8%), healthcare providers (n = 598; 84.5%), health officials (n = 491; 69.9%) as the most reliable media sources of COVID-19 information. Participants who would not take the COVID-19 vaccine (n = 116; 13.2%) reported healthcare providers (n = 66; 62.9%), the WHO (n = 60; 58.3%), and health officials (n = 49; 47.6%) as the most reliable sources of COVID-19 information (Fig. 2).
Additionally, participants who would take the COVID-19 vaccine (n = 762; 86.8%) reported the highest confidence in healthcare providers (n = 611; 85.9%), the WHO (= 567; 80.8%), and the health ministry (n = 400; 56.6%). Participants who would not take the COVID-19 vaccine (n = 116; 13.2%) reported the highest confidence in healthcare providers (n = 64; 61.0%), the WHO (n = 52; 50.5%) and the health ministry (n = 39; 37.1%).
4 Discussion
During early 2021, the majority of HCWs in Lebanon reported they would accept a COVID-19 vaccine (86.8%). Our finding of 86.8% is significantly higher than what was previously reported among Lebanese HCWs (26.8%) [29]. The major difference between both acceptance rates may be because our study collected data more recently (January 2021 to May 2021), compared to the previous study that collected data only in January 2021. Therefore, the acceptance of COVID-19 vaccines among Lebanese HCWs may have been higher in our study as evidence for the efficacy of the vaccines became more widely available over time [30]. Another possible reason for the major difference in acceptance rates may be due to the difference in methodologies between both studies—our study distributed the survey via email, WhatsApp message, or Short Message Service (SMS), while the previous study only used social media platforms to recruit participants. Moreover, our high acceptance rate surpasses that of previous studies conducted in HCWs in the KSA (64.9%), the United Arab Emirates (UAE) (89.2%), France (76.9%), Belgium (76.0%), Malta (52%), U.S. (36%), and the Democratic Republic of Congo (27.7%) [14, 19, 25, 31, 32]. While this is not a direct comparison as some of these countries were surveyed prior to the vaccine becoming available, some countries, such as the UAE (89.2%), have reported a similarly high acceptance rate as found in our study.
Among those who refused COVID-19 vaccination, the main reason for their refusal was that the vaccine had not been tested well yet (54.9%). The rapid development of COVID-19 vaccines is thus manifesting as a major factor in vaccine hesitancy, as studies from the U.S. imply that the accelerated vaccine approval process played an important role in this regard [33]. Additionally, other reasons for vaccine refusal in our survey were attributed to lack of trust in those developing and distributing the vaccine as well as fear of potential side effects. Lack of trust is a global phenomenon as the amount of circulating misinformation about the SARS-CoV-2 virus has been a major factor in people losing confidence in governments and health care officials [34]. This offers an opportunity to address the important role of government officials and the Ministry of Public Health in increasing vaccine confidence by disseminating accurate information about the COVID-19 vaccine, whether through expert panels on the science and manufacturing of these vaccines, or the continued showcase of the incredibly abundant emerging safety data.
The vaccines approved and administered in Lebanon are currently the Pfizer-BioNTech, Oxford-AstraZeneca, Sputnik V, and Sinopharm vaccines [7]. Although these vaccines have been thoroughly tested, approved, and administered to hundreds of millions around the world, the high acceptance rate reported in HCWs in this study was greater than that of the general population, which was found in a previous cross-sectional study conducted in Lebanon between November and December 2020 (21.4%) [22]. This may be because both studies were conducted at different time points—the general population was surveyed before COVID-19 vaccines were introduced in Lebanon, while our study was conducted when vaccine administration began for HCWs. Additionally, HCWs may have a higher COVID-19 vaccine acceptance rate than the general population because they are likely to be more knowledgeable of the COVID-19 pandemic, given their direct exposure to COVID-19 cases.
Studies have shown that the recommendation of governments and healthcare providers of the COVID-19 vaccination is a positive predictor of acceptance in patients [35]. The disparity in acceptance between HCWs and the general population offers an opportunity for our health care professionals to mobilize the population to encourage individuals to get the COVID-19 vaccine. This should be done through campaigns, media appearances, and active encouragement in clinics and hospital settings to boost receipt as much as possible. This suggests that the Lebanese MOPH could also work with the Lebanese HCWs to develop COVID-19 messaging and educational campaigns that cater to the general Lebanese population. One intervention that has worked well to help increase COVID-19 vaccine rates is the Inter-ministerial and Municipal Platform for Assessment Coordination and Tracking (IMPACT) national vaccination platform [36]. IMPACT generates online real-time data dashboards, supports assisted vaccine registration, allows users to report adverse events following vaccination, and includes a call center that assists with rescheduling appointments [36]. Overall, IMPACT has increased the transparency of the Lebanese MOPH’s vaccination rollout and boosted public trust [36].
As stated earlier, a major pillar in vaccine hesitancy is related to reduced confidence in vaccine manufacturers, distributors, governments and international organizations. Our study found that a majority of Lebanese HCWs highly regard the Lebanese MOPH and the WHO as reliable sources of information in relation to COVID-19. Additionally, Lebanese HCWs reported confidence in health care providers (doctors, nurses, and pharmacists), which underscores the importance of spreading the correct scientific information by these authoritative bodies and successfully competing with widespread misinformation falsely spread on social media. Reported confidence and trust of HCWs in their peers also highlights the need for healthcare providers to have peer-based interventions (e.g., engaging in expert panels and conferences to learn about the evolving vaccine safety and effectiveness data), which may increase COVID-19 vaccine acceptance [37].
After adjusting our data for multiple demographic characteristics, no significant differences in vaccine acceptance were found according to age or gender of participants. This is in contrast to multiple other studies that found women HCWs to be less likely to accept the COVID-19 vaccine [14, 26]. The fact that the largest number of health care professionals surveyed were nurses and considering that the Lebanese nurse force is mainly female predominant, this might offer a possible explanation [38]. Nurses, since the beginning of the COVID-19 pandemic, have been spearheading the COVID-19 response and are thus responsible for taking care of the sickest and critical patients. This could explain the high rates of vaccine approval among this demographic, who may fear the morbidity and mortality associated with the COVID-19 infection.
Similarly, after adjustment of multiple demographic factors, no significant findings concerning the impact of religion on willingness to take the vaccine were reported in our study. When comparing with other studies, no clear association between religion and vaccine hesitancy was seen, as some studies showed religion influencing vaccine acceptance, while other studies showed no significant effects [39,40,41,42]. Our finding that there was no significant association between chronic conditions and vaccine acceptance was similar to a study conducted in Singapore [43], yet different from a separate study conducted in Ethiopia [44]. The lack of significant association between chronic conditions and vaccine acceptance found in our study may be due to HCWs’ low risk perception for chronic conditions as being a catalyst for increasing the risk of hospitalization and death. As for religion, given Lebanon’s religious diversity among its population, it would be interesting to further investigate participants’ religious views and their level of religiosity to understand this lack of association.
HCWs with a previous SARS-CoV-2 infection were found to be less likely to take the COVID-19 vaccine as compared with those who had not been infected. A possible explanation of this finding is a false perception of acquired natural immunity in these individuals prompting them to decline future vaccines. According to the Center for Disease Control and Prevention (CDC) in the U.S., current recommendations are for individuals to be vaccinated regardless of previous infection status, as we do not yet know the extent and duration of naturally produced immunity from COVID-19 [45]. This subgroup of Lebanese HCWs must thus be targeted by pro-vaccine campaigns, and health care officials must take the lead in correcting any misinformation in this regard, especially before it begins to spread across the general Lebanese population. The uncertainty of one’s SARS-Cov-2 infection history may influence an individual’s willingness to take the vaccine. Those who may have caught the virus and have acquired immunity against it may decide that they do not need the vaccine. Others may claim that they may have contracted the virus, yet still decide to take the vaccine for extra precaution and prevention of an additional future infection.
Moreover, because several SARS-CoV-2 variants emerged since we collected our data in the beginning of 2021, HCWs' perceptions may have changed during this time. For example, Omicron variants that started in January 2022 had a significant impact on HCWs, where only two-thirds of HCWs felt that vaccination was the best option to prevent the spread of the Omicron variant from early 2022—indicating the need for further messaging campaigns for COVID-19 vaccination [46].
4.1 Strengths and Limitations
While our study included a large enough sample size of 879 HCWs, and we knew our target population included approximately 20,000 HCWs, we were unable to track the number of emails and messages (WhatsApp and SMS) that were received, returned, and/or went to spam. Therefore, we were unable to calculate the response rate. Also, given that we used a purposive sampling method and not a stratified random sample; our findings may not be generalizable to the whole Lebanese HCW population. Furthermore, our study examined the intent to vaccinate, which may not always translate into vaccine uptake [47]. Moreover, because our survey did not define “chronic conditions” and whether these conditions were related to COVID-19, participants may have interpreted this differently, which may have affected our results.
Given that the French language is one of the most commonly spoken languages in Lebanon and the survey was only provided in English or Arabic, participants who did not read and understand English or Arabic may have not participated in our study. Lastly, our findings may be influenced by a social desirability bias, as HCWs may respond to the survey questions in a manner that is viewed favorably by others.
However, the main strength of this study is that participants were from multiple hospitals throughout different areas of Lebanon, so it is representative in this regard. Also, to our knowledge, this is the first study in Lebanon that helps understand COVID-19 vaccine perception and acceptance among HCWs, as opposed to studies done on the general population.
5 Conclusion
Our study showed that 86.8% of the Lebanese HCWs would accept a COVID-19 vaccine. Refusal of vaccination was mainly due to the perception that COVID-19 vaccines have not been tested well. The surveyed HCWs showed great confidence in the MOPH and WHO, which must be key communication platforms in the COVID-19 vaccination campaign. Lebanese health care authorities can utilize these findings to establish COVID-19 programs to improve vaccine acceptance and uptake among HCWs and the general public.
Data Availability
Data are available upon request due to privacy and ethical restrictions.
Abbreviations
- HCWs:
-
Health care workers
- COVID-19:
-
Coronavirus Disease-2019
- LMICs:
-
Low- and middle-income countries
- COVAX:
-
COVID-19 Vaccines Global Access
- WHO:
-
World Health Organization
- MOPH:
-
Ministry of Public Health
- mRNA:
-
Messenger Ribonucleic acid
- U.S.:
-
United States
- KSA:
-
Kingdom of Saudi Arabia
- UN:
-
United Nations
- SARS-CoV-2:
-
Severe Acute Respiratory Syndrome-Coronavirus-2
- IRB:
-
Institutional Review Board
- SMS:
-
Short Message Service
- SPSS:
-
Statistical Package for Social Sciences
- OR:
-
Odds Ratio
- CI:
-
Confidence Interval
- UAE:
-
United Arab Emirates
- CDC:
-
Center for Disease Control and Prevention
References
World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. 2021; Available from: Available at: https://covid19.who.int/. Accessed 27 Aug 2021
Okereke M, et al. Impact of COVID-19 on access to healthcare in low- and middle-income countries: current evidence and future recommendations. Int J Health Plann Manage. 2021;36(1):13–7.
Khoury P, et al. COVID-19 Response in Lebanon: current experience and challenges in a low-resource setting. JAMA. 2020;324(6):548–9.
El Cheikh J, et al. Implemented Interventions at the Naef K. Basile Cancer Institute to protect patients and medical personnel From COVID infections: effectiveness and patient satisfaction. Front Oncol. 2021. https://doi.org/10.3389/fonc.2021.68510.
World Health Organization. COVAX, Working for global equitable access to COVID-19 vaccines. 2022; Available from: https://www.who.int/initiatives/act-accelerator/covax. Accessed 24 Feb 2022
Lebanese Ministry of Public Health. Lebanon National Deployment and Vaccination Plan for COVID-19 Vaccines. 2021; Available from: https://www.moph.gov.lb/userfiles/files/Prevention/COVID-19%20Vaccine/Lebanon%20NDVP-%20Feb%2016%202021.pdf. Accessed 9 Aug 2021
Mumtaz GR, et al. Modeling the impact of COVID-19 vaccination in Lebanon: a call to speed-up vaccine roll out. Vaccines. 2021;9(7):697.
World Health Organization. Coronavirus disease (COVID-19): Vaccines. 2020; Available from: https://www.who.int/news-room/q-a-detail/coronavirus-disease-(covid-19)-vaccines?topicsurvey=v8kj13)&gclid=Cj0KCQjwwY-LBhD6ARIsACvT72Nr6Ha1E5LDJXj10_T8_llunO1NS9kIplbGz_J8jqQ57KovRogdaIcaAr9bEALw_wcB. Accessed 1 Nov 2021
Larson HJ, et al. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine. 2014;32(19):2150–9.
Karafillakis E, et al. Vaccine hesitancy among healthcare workers in Europe: a qualitative study. Vaccine. 2016;34(41):5013–20.
Lazarus JV, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–8.
Dzieciolowska S, et al. Covid-19 vaccine acceptance, hesitancy, and refusal among Canadian healthcare workers: a multicenter survey. Am J Infect Control. 2021;49(9):1152–7.
Fisher KA, et al. Attitudes toward a potential SARS-CoV-2 vaccine : a survey of U.S. adults. Ann Intern Med. 2020;173(12):964–73.
Elharake JA, et al. COVID-19 Vaccine acceptance among health care workers in the Kingdom of Saudi Arabia. Int J Infect Dis. 2021;109:286–93.
Saddik B, et al. Determinants of healthcare workers perceptions, acceptance and choice of COVID-19 vaccines: a cross-sectional study from the United Arab Emirates. Hum Vaccin Immunother. 2022;18(1):1–9.
Al-Metwali BZ, et al. Exploring the acceptance of COVID-19 vaccine among healthcare workers and general population using health belief model. J Eval Clin Pract. 2021;27(5):1112–22.
Yigit M, Ozkaya-Parlakay A, Senel E. Evaluation of COVID-19 vaccine acceptance of healthcare providers in a tertiary Pediatric hospital. Hum Vaccin Immunother. 2021;17(9):2946–50.
Adeniyi OV, et al. Acceptance of COVID-19 vaccine among the healthcare workers in the Eastern Cape, South Africa: a cross sectional study. Vaccines (Basel). 2021;9(6):666.
Verger P, et al. Attitudes of healthcare workers towards COVID-19 vaccination: a survey in France and French-speaking parts of Belgium and Canada, 2020. Euro Surveill. 2021;26(3):666.
Malik AA, et al. Determinants of COVID-19 vaccine acceptance in the US. EClin Med. 2020;26: 100495.
Tankwanchi AS, et al. Taking stock of vaccine hesitancy among migrants: a scoping review protocol. BMJ Open. 2020;10(5): e035225.
Al Halabi K, et al. Attitudes of Lebanese adults regarding COVID-19 vaccination. BMC Public Health. 2021;21(1):998.
World Bank Group. World Health Organization's Global Health Workforce Statistics, OECD, supplemented by country data. 2021 01/11/2021]; Available from: https://data.worldbank.org/indicator/SH.MED.PHYS.ZS?locations=LB. Accessed 1 Nov 2021
World Medical Association (2013) WMA declaration of Helsinki – ethical principles for medical research involving human subjects, pp 1–4
Shekhar V, et al. COVID-19 vaccine acceptance among health care Workers in the United States. Vaccines (Basel). 2021;9(2):119.
Detoc M, et al. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine. 2020;38(45):7002–6.
Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines. 2021;9(2):160.
SPSS Statistics. Tests of Model Fit. 2021; Available from: https://www.ibm.com/docs/en/spss-statistics/28.0.0?topic=diagnostics-tests-model-fit
Qunaibi, et al. Hesitancy of Arab healthcare workers towards COVID-19 vaccination: a large-scale multinational study. Vaccines. 2021;9(5):446.
Temsah M-H, et al. Changes in healthcare workers’ knowledge, attitudes, practices, and stress during the COVID-19 pandemic. Medicine. 2021;100(18):e25825.
AlKetbi MB, et al. COVID-19 vaccine acceptance among healthcare workers in the United Arab Emirates. IJID Regions. 2021;1:20–6.
Gagneux-Brunon A, et al. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross-sectional survey. J Hosp Infect. 2021;108:168–73.
Latkin CA, et al. Trust in a COVID-19 vaccine in the U.S.: a social-ecological perspective. Soc Sci Med. 2021;270:113684.
Khurshid A. Applying Blockchain technology to address the crisis of trust during the COVID-19 pandemic. JMIR Med Inform. 2020;8(9): e20477.
Joshi A, et al. Predictors of COVID-19 vaccine acceptance, intention, and hesitancy: a scoping review. Front Public Health. 2021;9:698111.
Varkey S (2022) Lebanon’s COVID-19 vaccination digital platform promotes transparency & public trust. 2022 [cited 2022 September]; Available from: https://blogs.worldbank.org/arabvoices/lebanons-covid-19-vaccination-digital-platform-promotes-transparency-public-trust
Blake H, et al. COVID-19 vaccine education (CoVE) for health and care workers to facilitate global promotion of the COVID-19 vaccines. Int J Environ Res Public Health. 2022;19(2):653.
Order of Nurses in Lebanon. Statistics issued by the Order. 2020; Available from: http://orderofnurses.org.lb/PDF/STATS2020EN.pdf
Freeman D, et al. COVID-19 vaccine hesitancy in the UK: the Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol Med. 2020;52(14):3127–41.
Guidry JPD, et al. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am J Infect Control. 2021;49(2):137–42.
Kilic M, Ustundag Ocal N, Uslukilic G. The relationship of Covid-19 vaccine attitude with life satisfaction, religious attitude and Covid-19 avoidance in Turkey. Hum Vaccin Immunother. 2021;17(10):3384–93.
Sherman SM, et al. COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Hum Vaccin Immunother. 2021;17(6):1612–21.
Koh SWC, et al. COVID-19 vaccine acceptance and hesitancy among primary healthcare workers in Singapore. BMC Primary Care. 2022;23(1):81.
Angelo AT, Alemayehu DS, Dachew AM. Health care workers intention to accept COVID-19 vaccine and associated factors in southwestern Ethiopia, 2021. PLoS ONE. 2021;16(9): e0257109.
Center for Disease Control and Prevention. Benefits of Getting a COVID-19 Vaccine. 2021 6 September 2021 ]; Available from: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/vaccine-benefits.html. Accessed 6 Sept 2021
Temsah MH, et al. SARS-CoV-2 omicron variant: exploring healthcare workers’ awareness and perception of vaccine effectiveness: a national survey during the first week of WHO variant alert. Front Public Health. 2022;10: 878159.
McEachan RRC, et al. Prospective prediction of health-related behaviours with the theory of planned behaviour: a meta-analysis. Health Psychol Rev. 2011;5(2):97–144.
Acknowledgements
We acknowledge the participating hospitals, and the Lebanese Orders of Physicians, Nurses, and Pharmacists.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
JAE, BG, KK, SBO, and ZAM conceptualized the study. SMM and AAM designed the initial survey questionnaire. CFB adapted the survey for a Lebanese context, cleaned the data and performed the analyses. NJF, NKT, MMM, and CFB wrote the initial draft of the manuscript. All authors read, edited, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical Approval
Ethical approval for this research was obtained from the Institutional Review Boards (IRB) at the American University of Beirut Medical Center (IRB protocol number: SBS-2020-0563). After we informed the subjects about the purpose of the study, E-consent was required prior to data collection.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Youssef, N.J., Tfaily, N.K., Moumneh, M.B.M. et al. COVID-19 Vaccine Acceptance and Hesitancy Among Health Care Workers in Lebanon. J Epidemiol Glob Health 13, 55–66 (2023). https://doi.org/10.1007/s44197-023-00086-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44197-023-00086-4