Abstract
Purpose
Military surgeons have the unique responsibility of maintaining a broad set of surgical skills to care for combat-related injuries during times of peace. Lower and upper limb amputations are life-altering combat injuries sustained by our military personnel. Salvage of a limb saves someone from impaired mobility, abnormal physiology, and social effects of amputation and requires the knowledge and technical proficiency to diagnose and treat vascular traumatic injuries.
Methods
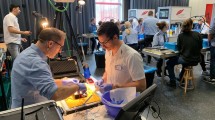
A needs assessment of deployable military surgeons was performed which demonstrated a need for additional training to diagnose and treat vascular emergencies. For simulation skills training, a novel low-cost arterial model was developed by our institution's mixed material layering 3D medical applications center. A focused simulation curriculum was developed which included both didactic and technical skills training for vascular trauma emergencies. Learners were assessed using a pre-, post-test design to evaluate efficacy.
Results
A realistic vascular model was developed using 3D printed technologies and was used for traumatic vascular emergency skills training. Implementation of the VESSELS course using both in-person and online asynchronous formats demonstrated significant increases in knowledge and confidence in diagnosing and managing limb-threatening injuries.
Conclusions
A novel, low-cost simulation model and curriculum was developed that increases the understanding of vascular surgical techniques and emergency procedures. This course is an option for deploying military surgeons and surgeons without vascular training who are responsible for managing vascular emergencies.


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Farrokhi S, Perez K, Eskridge S, Clouser M. Major deployment-related amputations of lower and upper limbs, active and reserve components, U.S. Armed Forces, 2001–2017. MSMR. 2018;25(7):10–6.
Webster JB. Lower limb amputation care across the active duty military and veteran populations. Phys Med Rehabil Clin North Am. 2019;30(1):89–109. https://doi.org/10.1016/j.pmr.2018.08.008.
Stamper DH, Jones RS, Thompson JC. Simulation in health care provider education at Brooke Army Medical Center. Mil Med. 2008;173(6):583–7. https://doi.org/10.7205/milmed.173.6.583.
Kuhls DA, Risucci DA, Bowyer MW, Luchette FA. Advanced surgical skills for exposure in trauma: a new surgical skills cadaver course for surgery residents and fellows. J Trauma Acute Care Surg. 2013;74(2):664–70. https://doi.org/10.1097/TA.0b013e31827d5e20.
Khamis NN, Satava RM, Alnassar SA, Kern DE. A stepwise model for simulation-based curriculum development for clinical skills, a modification of the six-step approach. Surg Endosc. 2016;30(1):279–87. https://doi.org/10.1007/s00464-015-4206-x.
Widmer MK, Davidson I, Widmer LW, Schmidli J, Wyss TR. Simulation in vascular access surgery. Contrib Nephrol. 2015;184:87–96. https://doi.org/10.1159/000365825.
Widmer LW, Schmidli J, Widmer MK, Wyss TR. Simulation in vascular access surgery training. J Vasc Access. 2015;16(Suppl 9):S121–5. https://doi.org/10.5301/jva.5000372.
Ballard HA, Tsao M, Robles A, et al. Use of a simulation-based mastery learning curriculum to improve ultrasound-guided vascular access skills of pediatric anesthesiologists. Paediatr Anaesth. 2020;30(11):1204–10. https://doi.org/10.1111/pan.13953.
Pantoja JL, Archie MM, Baril DT, Moore WS, Lawrence PF. Trainee experience in simulation-based education of open vascular surgery. Ann Vasc Surg. 2021;73:147–54. https://doi.org/10.1016/j.avsg.2020.11.026.
Lawaetz J, Nayahangan LJ, Strøm M, et al. Learning curves and competences of vascular trainees performing open aortic repair in a simulation-based environment. Ann Vasc Surg. 2021;72:430–9. https://doi.org/10.1016/j.avsg.2020.09.009.
Iwamoto Y, Maruhashi T, Fujii Y, et al. Intima-media thickness of brachial artery, vascular function, and cardiovascular risk factors. Arterioscler Thromb Vasc Biol. 2012;32(9):2295–303. https://doi.org/10.1161/ATVBAHA.112.249680.
Mohan V, Ravikumar R, Shanthi Rani S, Deepa R. Intimal medial thickness of the carotid artery in South Indian diabetic and non-diabetic subjects: the Chennai Urban Population Study (CUPS). Diabetologia. 2000;43(4):494–9. https://doi.org/10.1007/s001250051334.
Soneye MA, Adekanmi AJ, Obajimi MO, Aje A. Intima-media thickness of femoral arteries and carotids among an adult hypertensive Nigerian population: a case-control study to assess their use as surrogate markers of atherosclerosis. Ann Afr Med. 2019;18(3):158–66. https://doi.org/10.4103/aam.aam_57_18.
Tomiyama Y, Yoshinaga K, Fujii S, et al. Accurate quantitative measurements of brachial artery cross-sectional vascular area and vascular volume elastic modulus using automated oscillometric measurements: comparison with brachial artery ultrasound. Hypertens Res. 2015;38(7):478–84. https://doi.org/10.1038/hr.2015.6.
Mayer R, Moreno R. A cognitive theory of multimedia learning: implications for design principles. 91. 2005.
Mcgaghie WC, Harris IB. Learning theory foundations of simulation-based mastery learning. Simul Healthc. 2018;13(3 Suppl 1):S15–20. https://doi.org/10.1097/SIH.0000000000000279.
Poore JA, Cullen DL, Schaar GL. Simulation-based interprofessional education guided by Kolb’s experiential learning theory. Clin Simul Nurs. 2014;10(5):241–7. https://doi.org/10.1016/j.ecns.2014.01.004.
Morrow DS, Broder J. Cost-effective, reusable, leak-resistant ultrasound-guided vascular access trainer. J Emerg Med. 2015;49(3):313–7. https://doi.org/10.1016/j.jemermed.2015.04.005.
Tan TX, Wu YY, Riley I, Duanmu Y, Rylowicz S, Shimada K. Development of a three-dimensionally printed ultrasound-guided peripheral intravenous catheter phantom. Cureus. 2021;13(8): e17139. https://doi.org/10.7759/cureus.17139.
Sarmento PLFA, Fernandes AL, do Vale BL, et al. Latex balloons: an alternative, low-cost model for vascular anastomosis training in medical education. J Vasc Bras. 2018;17(3):267–72. https://doi.org/10.1590/1677-5449.170111.
Melkonian V, Huy T, Varma CR, Nazzal M, Randall HB, Nguyen MJ. The creation of a novel low-cost bench-top kidney transplant surgery simulator and a survey on its fidelity and educational utility. Cureus. 2020;12(11): e11427. https://doi.org/10.7759/cureus.11427.
McGuire LS, Fuentes A, Alaraj A. Three-dimensional modeling in training, simulation, and surgical planning in open vascular and endovascular neurosurgery: a systematic review of the literature. World Neurosurg. 2021;154:53–63. https://doi.org/10.1016/j.wneu.2021.07.057.
Mashiko T, Otani K, Kawano R, et al. Development of three-dimensional hollow elastic model for cerebral aneurysm clipping simulation enabling rapid and low cost prototyping. World Neurosurg. 2015;83(3):351–61. https://doi.org/10.1016/j.wneu.2013.10.032.
American College of Surgeons. Trauma education: Advanced surgical skills for exposure in trauma. https://www.facs.org/quality-programs/trauma/education/asset/. Accessed 16 May 2022.
Simpson JS. An economical approach to teaching cadaver anatomy: a 10-year retrospective. Am Bio Teach. 2014;76(1):42–6. https://doi.org/10.1525/abt.2014.76.1.9.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclaimer: The contents of this publication are the sole responsibility of the authors and do not necessarily reflect the views, opinions, or policies of The Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc., the Uniformed Services University of the Health Sciences (USUHS), the Department of Defense (DoD), or the Departments of the Army, Navy, or Air Force. Mention of trade names, commercial products, or organizations does not imply endorsement by the U.S. Government.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hickey, C., Davic, M., Sweeney, W.B. et al. Vascular Emergency Surgery: Simulated Exercises for Limb Salvage (VESSELS)—development of a simulation model and curriculum for the military general surgeon. Global Surg Educ 2, 35 (2023). https://doi.org/10.1007/s44186-023-00110-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44186-023-00110-y