Abstract
Purpose
A “one-size-fits-all” treatment recommendation is not advisable for nasopharyngeal carcinoma (NPC). This article aims to review the risk-stratified strategies and propose future directions in NPC.
Results
For low-risk NPC patients, a review of literature shows that de-escalation approaches can be generally categorized into de-escalating systemic therapy and de-escalating radiotherapy. Studies have explored the exemption of concurrent chemotherapy in stage II and T3N0M0 NPC patients, as well as sparing concurrent chemotherapy after induction chemotherapy in selected low-risk patients, changing the cisplatin-based chemotherapy schedules, and doses. De-escalation of radiotherapy involves a reduction in dose and clinical treatment volume (CTV). For high-risk patients, increasing treatment intensity is commonly used, including selecting appropriate patients to receive induction or adjuvant chemotherapy or adding targeted therapy to standard chemo-radiotherapy to improve survival. In many instances, these risk-stratified approaches are guided by the measurement of Epstein-Barr virus DNA levels and various image-based modalities. Immunotherapy has shown initial efficacy in recurrent or metastatic NPC patients. The treatment advances of ICIs monotherapy in Locoregionally advanced NPC have remained scarce, and several phase II and III anti-PD-1/PD-L1 monoclonal antibody clinical trials are currently underway.
Conclusions
Various strategies for the risk-stratified treatment of NPC have been investigated and remain highly effective in most approaches. Optimization of patient selection is still critical, and both long-term oncological outcomes and late complications remain to be determined. More prospective, multi-institutional researches are needed to elucidate how best to individualize the treatment of NPC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Nasopharyngeal carcinoma (NPC) has a unique etiology and geographic distribution which is mainly seen in Southeast Asia [1]. NPC is highly sensitive to radiotherapy and chemotherapy. The National Comprehensive Cancer Network (NCCN) guidelines recommend definitive radiotherapy alone for stage I, chemoradiotherapy for stage II, and chemoradiotherapy with induction or adjuvant chemotherapy for stages III to IVA [2]. More than 50% of patients with NPC present with locally advanced disease. Locoregionally advanced NPC (LA-NPC) is a heterogeneous patient population, with the prognosis of early-stage III NPC more closely resembling that of stage II disease [3], while T4 and N3 tumors have significantly poorer survival rates with a high risk of local–regional recurrences and/or distant metastasis [4]. Therefore, a “one-size-fits-all” treatment recommendation is not advisable. Recently, risk-stratified management strategies for NPC have attempted to individualize treatments to limit toxicity without compromising efficacy in low-risk patients and to improve survival in the high-risk patient. This article aims to review the risk-stratified strategies and propose future directions for de-escalating systemic chemotherapy or radiotherapy in low-risk NPC and increasing the intensity of treatment to improve survival in high-risk NPC.
1.1 De-escalation strategies for systemic chemotherapy
1.1.1 Omitting concurrent chemotherapy in low-risk stage II and T3N0 patients with NPC
Most recently, a multicenter, open-label, randomized, phase III, noninferiority clinical trial was conducted to assess whether concurrent chemotherapy can be safely omitted for patients with low-risk stage II and T3N0M0 NPC treated with IMRT (pretreatment plasma EBV DNA ≤ 4,000 copies/mL, maximal diameter of cervical LN ≤ 3 cm, without level IV or Vb lymph node and extranodal extension) [5]. In this study, there were no significant differences were observed in 3-year failure-free survival (FFS) between the IMRT-alone group and the CCRT group (91.9% vs. 90.5%, P value for noninferiority, < 0.001). But the IMRT-alone group experienced a significantly lower incidence of grade 3 to 4 adverse events (17% vs. 46%), including hematologic toxicities (leukopenia, neutropenia) and non-hematologic toxicities (nausea, vomiting, anorexia, weight loss, mucositis).
1.1.2 Sparing concurrent chemotherapy after induction chemotherapy in selected low-risk patients with NPC
In this era when IMRT has markedly improved locoregional control of LA-NPC [6], CCRT may provide only modest benefit while producing unnecessary toxicity. Among the chemotherapy regimens, induction chemotherapy (IC) is increasingly recommended given its advantages of better tolerance and earlier eradication of micrometastases. In this context, debates exist on whether concurrent chemotherapy should be maintained in the IC setting in the IMRT era.
Various studies have compared the outcomes of IC + CCRT versus IC + IMRT (Table 1). Regarding retrospective evidence, most studies without restricted inclusion criteria reported that IC + IMRT alone obtained similar survival outcomes with IC before CCRT for LA-NPC patients, but a relatively lower incidence of treatment-related toxicities [7,8,9,10,11,12]. Only one study by Chen et.al [13] reported improved OS in a subset of patients, mainly N3 or T4 patients, or those with larger tumor volumes after IC treatment, but no improvement was found in DMFS or LRRFS.
A phase III randomized controlled trial is underway to compare the survival outcomes and side effects of radiotherapy alone and CCRT in LA-NPC patients with satisfactory tumor response (CR or PR) after IC receiving IMRT or tomotherapy (TOMO) (NCT03015727). While awaiting more convincing evidence, optimization of patient selection to continue or cancel concurrent chemotherapy is imperative to ensure treatment efficacy and avoid excessive toxicity.
1.1.3 Cisplatin schedules
In NPC, there is no level 1 evidence of comparable efficacy to cisplatin once every 3 weeks. The multicenter randomized phase II trial (KCSG-HN10-02) compared weekly (40 mg/m2) and triweekly cisplatin (100 mg/m2) in 109 patients and observed no significant difference in 3-year PFS (64.9% vs. 63.8%) or grade 3–4 toxicities (47.2% vs. 39.3%). But the QoL related to functional outcomes in triweekly regimen after treatment completion was better for the weekly regimen [14]. Recently, the preliminary results of a large phase III randomized controlled trial enrolling 526 patients with LA-NPC (ChiCTRC-12001979) showed no difference in survival outcomes between the two regimens, but the incidence of leukopenia (27.3% vs. 16.2%) and thrombocytopenia (4.8% vs. 1.2%) is higher in the once-weekly regimen group compared to the once-every-3-weeks regimen group [15]. The final results of this study might help to fully evaluate the different cisplatin schedules.
1.1.4 Cisplatin cumulative dose
Cisplatin toxicity is dose-dependent and complications, including ototoxicity, neuropathy, and nephrotoxicity, increase substantially with cisplatin cumulative dose (CCD), which could reach as high as 540 to 600 mg/m2 when sequential chemotherapy is contemplated [16,17,18,19]. Currently, there is no high-level evidence to guide the optimal dose intensity of concurrent cisplatin chemotherapy. Regarding studies to decide the minimum threshold for CCD in NPC, an updated combined analysis of 2 randomized studies (NPC-9901 and NPC-9902 trials) showed no difference in disease control (5-year locoregional-FFR, 88% vs. 88%) between 2 or 3 cycles of concurrent cisplatin; however, patients given 3 concurrent cycles had a significant increase in hearing impairment (40% vs. 24%, P = 0.017) [20]. Subsequently, a secondary analysis of a prospective phase III clinical trial [21] demonstrated that a CCD of 200 mg/m2 during CCRT is adequate to achieve satisfactory survival outcomes for patients with locoregionally advanced NPC. Additionally, a CCD of ≥ 240 mg/m2 was not an independent prognostic factor in patients with LA-NPC at high risk of distant metastasis. These studies showed that a cumulative CCD of 200 mg/m2 should be the threshold for achieving satisfactory survival.
Assigning treatment based on response allows another method of improved patient selection for patients with excellent prognoses. The outcomes of a retrospective study [22] revealed that in the subgroup of patients who achieved CR/PR after IC, there were no significant differences between > 200 mg/m2 and 101–200 mg/m2 for all endpoints, but was associated with fewer grade 1–4 acute toxicities. In addition, the application of different CCDs did not result in significantly different survival outcomes in the subgroup of patients who were stable disease (SD)/progressive disease (PD) after IC. However, this was a retrospective study and the data were obtained exclusively from one center; therefore, these results must be validated by other datasets.
At least three meta-analyses have confirmed that pretreatment plasma EBV DNA was a significant prognostic of survival and has been widely used as a predictor of risk stratification in recent studies [23,24,25]. By using pretreatment EBV DNA in risk stratification, Li et al. [26] performed an open-label, phase II, randomized, controlled trial to test the noninferiority of a two-cycle 100 mg/m2 concurrent DDP regimen over three-cycle in patients with low-risk LA-NPC with pretreatment EBV DNA levels < 4,000 copies/mL. In all, 332 patients were enrolled in this trial. After a median follow-up of 37.7 months, the 3-year PFS rate for the two-cycle group was 2.4% lower than the three-cycle group (88.0% vs. 90.4%) and met its primary endpoint of proving non-inferiority. Expectedly, there was a higher compliance rate in the two-cycle group than in the three-cycle group, with 165 (99.4%) of 166 patients completing two cycles of cisplatin compared with 149 (89.8%) of 166 patients completing three cycles. Patients who received only two cycles of cisplatin reported less insomnia, speech problems, xerostomia symptoms, constipation, and better cognitive functions than those who received three cycles. This study might represent a novel strategy to alter the current treatment dogma for low-risk LA-NPC.
1.2 De-escalation strategies for radiotherapy
1.2.1 Reducing doses of radiotherapy
With advances in modern radiotherapy techniques and effective systemic chemotherapy, local control for NPC has remained excellent at 90% [5]. Despite the widespread adoption of IMRT with reduced toxicity compared to conventional techniques, short- or long-term toxic effects such as mucositis, oral ulcers, and temporal lobe necrosis continue to adversely affect the QoL [17]. This finding is largely attributed to the total dose of 70 Gy near these critical normal tissues.
Considering long-term toxicities, treatment of NPC in children and adolescents has traditionally used IC to reduce radiation dose, and the 5-year event-free survival (EFS) has been achieved at 77% to 91% [27,28,29,30]. In the adult population, a single-arm, phase II trial is ongoing to assess whether an adaptive radiotherapy dose of 60 Gy after a favorable response to IC was non-inferior to the standard dose in low-risk stage III NPC patients (EBV DNA level < 4,000 copies/mL) [31]. The preliminary results of this trial revealed that the reduced-dose radiotherapy (60 Gy) is associated with favorable survival outcomes and limited treatment-related toxicities for low-risk stage III NPC patients sensitive to IC.
1.2.2 Reducing clinical target volume of radiotherapy
NPC has a high propensity for cervical node metastasis, 85% of NPC cases presented with lymphadenopathy [32]. Extensive studies on neck CTV volume reduction have mostly focused on investigating the feasibility of ipsilateral lower neck sparing irradiation for unilateral or bilateral neck node-negative NPC and have confirmed the safety, feasibility, and improved long-term QoL of this approach [33,34,35,36,37]. A recent randomized phase III noninferiority study demonstrated that elective upper-neck irradiation (UNI) of the uninvolved neck provides similar regional control and results in less radiation toxicity than standard whole-neck irradiation (WNI) in patients with N0-N1 NPC [34]. Nevertheless, the suitability of the above approach for patients with ipsilateral N2-3 disease and non-endemic populations requires further investigation. Moreover, these studies still depended heavily on the anatomical definition of the neck region without considering the specific site of lymph nodes. Therefore, effort is required to further optimize the nodal CTV delineation strategy in NPC. A multicenter non-inferiority randomized controlled phase III clinical trial (NCT05145660) from China is ongoing which aims to compare the regional control, survival outcomes, radiation-related toxicities, and QoL of Involved site irradiation (ISI) therapy, incorporated specific nodal site and spread distances of metastatic lymph nodes, with conventional elective region irradiation (ERI) in NPC patients with a limited nodal burden.
Specifically, several retrospective studies have explored the feasibility of omitting specific nodal levels. The risk of level Ib metastasis for patients with NPC is relatively low (2–8.5%). For those without risk factors for level Ib spreading, sparing Ib in prophylactic CTV has been proven to be safe by multiple studies [38,39,40]. However, for those with high-risk factors, which normally account for over one-third of all new patients [41], covering Ib is still recommended. Hence, attempts have been made to modify the CTV boundaries of level Ib. In a recent study [42], the shrinkage of the boundaries of level Ib specialized for NPC was proposed. The Ib CTVs that include the suggested modifications have significantly less volume than the CTVs suggested by the consensus. The normal tissue complication probability (NTCP) models further demonstrated that the risk of dysphagia would be significantly reduced, and the function of the submandibular gland (SMG) and the sublingual gland would be less affected by applying the CTV-proposed delineation.
1.3 Therapeutic intensification for high-risk NPC
1.3.1 high-risk NPC patients might benefit from IC
The 3 randomized phase III trials from China have proven the efficacy and effect of IC added to concurrent chemotherapy treatment mode, especially in stage III to IVA disease, on long-term patient outcomes [43,44,45]. Notably, however, the above-mentioned randomized trials did not enroll any patients staged with T3-4N0M0 or T3N1M0 at all. Some retrospective studies reported that patients with T3N0-1 do not benefit from IC [46], while male T3N1 patients with EBV DNA higher than 2000 copies/mL were the only target population for IC followed by CCRT, as suggested by another study [47].
In addition, not all patients in the above-mentioned 3 randomized phase III trials benefit from IC. Thus, in the spirit of informed decision-making, predictive models were developed to estimate the benefit of IC for individual patients would be particularly useful in clinical practice. The reasons for the results may be explained by the fact that the IC not only attenuates the tumor burden within a brief period to ameliorate tumor hypoxia but also exerts a systemic cytotoxic effect to eradicate distant micrometastases [48, 49]; therefore, patients with a high distant metastatic risk should consider treatment with IC + CCRT. However, all of the above studies are retrospective studies and multi-institutional and prospective studies are warranted to further validate these findings.
1.3.2 High-risk NPC patients might benefit from adjuvant chemotherapy
The benefit of adding adjuvant chemotherapy (AC) to chemoradiotherapy remains controversial in NPC [43, 50,51,52]. Most recently, Miao et.al [53] reported the efficacy and safety results in a randomized clinical trial of adjuvant capecitabine given at the full dose for 6 months. There were 180 patients enrolled and randomly assigned to receive in a 1:1 ratio either capecitabine (capecitabine group) or observation (control group) following CCRT (Eligibility included stage III-IVb NPC and at least 1 of the following: T3-4N2 or T1-4N3; plasma EBV DNA titer higher than 20,000 copies/mL; primary gross tumor volume larger than 30.0 cm3; [18F] FDG PET/CT maximum standard uptake value of the primary gross tumor volume larger than 10.0; or multiple nodal metastases and any larger than 4.0 cm). With a median follow-up of 58.0 months, 18 events were recorded in the capecitabine group vs. 31 events in the control group. The FFS was improved with adjuvant capecitabine (3 years, 83.3% vs.72.2%; 5 years, 78.5% vs. 65.9%; hazard ratio, 0.53; P = 0.03). The incidence of grade 3 treatment-related adverse events (TRAEs) was higher in the capecitabine group than in the control group (54 of 90 patients [60.0%] vs. 46 of 90 patients [51.1%]). TRAEs included xerostomia (17 [18.9%] vs. 9 [10.0%] patients), mucositis (21 [23.3%] vs. 15 [16.7%] patients), and anorexia (8 [8.9%] vs. 4 [4.4%] patients). The results of this randomized clinical trial support the use of capecitabine as an effective and tolerable adjuvant regimen for treating patients with LA-NPC.
1.3.3 Target therapy for high-risk patients
Epidermal growth factor receptor (EGFR) represents a promising new therapeutic target in cancer and is highly expressed in more than 85% of NPC patients. It is also an essential factor of prognosis for NPC, correlated with a more aggressive phenotype, and greater resistance to treatment. Therefore, anti-EGFR-targeted treatment is considered a potential addition to the standard CCRT regimen for NPC. In 2022, the randomized, controlled, multicenter phase III clinical trial by Sun et al. demonstrated the initial results of the clinical efficacy of long-term survival and safety of nimotuzumab combined with chemo-radiotherapy in LA-NPC patients. They found that Nimotuzumab plus chemo-radiotherapy increased the 5-year OS (76.9% vs. 64.3%, P = 0.042) in NPC patients. Besides, the combination of nimotuzumab plus chemo-radiotherapy was well tolerated. The incidence of adverse drug reactions (ADRs) in the nimotuzumab combined with the chemo-radiotherapy group was similar to the chemo-radiotherapy alone group (35.7% vs. 42.1%, P = 0.207), and the grade 3–5 ADRs as well (17.7% vs.15.7%, P = 0.609).
1.4 Future directions
1.4.1 Value of plasma EBV DNA for stratifying treatment
With emerging evidence for the induction-concurrent approach in advanced NPC, incorporations of EBV DNA early response as a mid-treatment prognosticator are under active investigation. Clearance of EBV DNA after systemic chemotherapy is associated with favorable drug response, and patients who attained undetectable EBV DNA after IC have significantly better survival [54,55,56]. In a large longitudinal study of 673 patients by Lv et.al [57], among the 30% early complete biochemical responders who achieved undetectable EBV DNA after a single cycle of chemotherapy, the 3-year DFS rate could reach as high as 94%. In this study, four distinct groups of patients were identified based on the kinetic of EBV DNA clearance: early responders had the best DFS, followed by intermediate responders, late responders, and the least for those who were treatment-resistant. Following this classification, a biomarker-guided risk-adopted treatment strategy was proposed (NCT04072107, currently recruiting patients): the intermediate responders (detectable EBV DNA after one cycle of IC but undetectable EBV DNA after subsequent IC) would receive adjuvant metronomic capecitabine for six months, while high-risk patients (detectable EBV DNA after three cycles of IC or early bounce of EBV DNA during induction phase) would receive concurrent anti-PD-1 therapy (sintilimab) with cisplatin and IMRT followed by adjuvant sintilimab for six months.
1.4.2 Imaging as biomarker
Applying noninvasive imaging biomarkers can predict early response to treatment and thus offers an opportunity for individualized risk-stratified treatment in NPC. MRI radiomic signatures are a superior tool in predicting responses to treatment and tumor failures in NPC [58, 59]. Dynamic contrast-enhanced MRI could be used to quantitatively assess microcirculation properties and hypoxia status of tumors because of the improved spatial resolution and signal-to-noise ratio over DWI [60].
Smaller apparent diffusion coefficient (ADC) values are related to a higher likelihood of diagnosing early NPC from nasopharyngeal lymphoid hyperplasia, as tumors with denser tumor cells and more cell membranes have lower ADCs due to greater restriction on diffusion [61]. A study in head and neck squamous cell carcinoma found that changes in ADC values after the first week of chemoradiotherapy had a high discriminatory ability in distinguishing CR from PR [62]. These studies support a potential opportunity where the total dose could be de-escalated or retained according to ADC changes throughout the treatment course. Thus, MRI radiomics is another opportunity for individualized risk-stratified treatment.
Another imaging modality that is crucial to treatment planning is PET. Chen et al. [63] investigated the value of early evaluation of response to CCRT using 18F-FDG PET-derived parameters and the EBV DNA titre in outcome prediction in patients with NPC. They found that Early evaluation of response to CCRT using 18F-FDG PET-derived parameters and the EBV DNA titre can predict outcome in patients with primary NPC. A combination of interim PET parameters and the EBV DNA titre enables better stratification of patients into subgroups with different survival rates. A study of patients with advanced NPC found that a combination of EBV DNA clearance and a reduction in maximum standardized uptake value of less than 50% at 4 weeks after initiation of chemotherapy was prognostic and predicted improvements in PFS and OS compared with either modality alone, which provided an opportunity for modification of treatment decisions at an early stage [64]. The functional aspect of PET allows tissue metabolic changes to be detected that may not be apparent on cross-sectional imaging and has also been found to be more accurate than MRI in the assessment of early treatment response [65]. These studies support a potential opportunity to identify low-risk groups who could potentially be spared from concurrent chemotherapy throughout the treatment course.
1.4.3 Immunotherapy
NPC is characterized by high PD-L1 expression (up to 90% of tumor cells) and abundant infiltration of non-malignant [66,67,68,69,70,71], which makes NPC patients potentially suitable for immune checkpoint blockade therapies. Several important single-arm trials evaluating anti-programmed death 1 (PD 1) antibodies, such as nivolumab, pembrolizumab, and camrelizumab, have demonstrated encouraging activity in recurrent or metastatic NPC (RM-NPC).
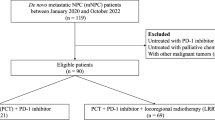
The treatment advances of ICIs monotherapy in LA-NPC have remained scarce, and currently, the optimal sequence to incorporate ICIs with definitive radiotherapy in NPC is uncertain. Although ICIs are not yet recommended in the guidelines for patients with LA-NPC, several phase II to III anti-PD-1/PD-L1 monoclonal antibody clinical trials are currently underway (Table 2). NCT04453826 and NCT03925090 aim to explore EBV-directed immunotherapies as alternatives to adjuvant chemotherapy for high-risk patients (ie, detectable EBV DNA after primary radiotherapy). NCT03925090 (induction and adjuvant toripalimab), NCT03427827 (adjuvant camrelizumab), and NCT03700476 (induction, concurrent and adjuvant sintilimab) will test the value of adding anti-PD-1 therapy to standard treatment in the curative setting. Three trials would be of interest to compare the efficacy of ICI as an adjuvant treatment (NCT04870905) or even as a radiosensitizer in replacement of cisplatin (NCT04907370 and NCT03984357). To this end, studies on predictive biomarkers (eg, PDL 1 expression, tumor mutational load, immune cell infiltration, and immune gene expression) to enrich treatment responses are crucial to guide patient selection (NCT03427827).
2 Conclusion
Various risk-stratified treatment strategies for NPC have been explored. The optimization of patient selection remains critical, and long-term outcomes remain to be determined. Attention needs to be paid to the generalizability of the results because subtypes of NPC can present in different manners. Continued investigation in prospective, multi-institutional studies is needed to elucidate how best to individualize the risk-stratified treatment of NPC.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- AC:
-
Adjuvant chemotherapy
- ADC:
-
Apparent diffusion coefficient
- ADRs:
-
Adverse drug reactions
- CCRT:
-
Concurrent chemoradiotherapy
- CR:
-
Complete response
- cCR:
-
Complete clinical response
- DWI:
-
Diffusion-weighted imaging
- EBV:
-
Epstein-Barr virus
- EGFR:
-
Epidermal growth factor receptor
- HPV:
-
Human papillomavirus
- MAD:
-
Maximum axial diameter
- NPC:
-
Nasopharyngeal carcinoma
- NCCN:
-
National Comprehensive Cancer Network
- IC:
-
Induction chemotherapy
- IMRT:
-
Intensity-modulated radiotherapy
- QoL:
-
Quality-of-life
- PR:
-
Partial response
- RCT:
-
Randomized-controlled trials
- TRAEs:
-
Treatment-related adverse events
References
Chen Y-P, Chan ATC, Le Q-T, Blanchard P, Sun Y, Ma J. Nasopharyngeal carcinoma. Lancet. 2019;394:64–80.
Pfister DG, Sharon S, David A, Douglas A, Yoshimi A, Brizel DM, et al. Head and Neck Cancers, Version 2.2020, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2020;18:873–98.
Au KH, Ngan RKC, Ng AWY, Poon DMC, Ng WT, Yuen KT, et al. Treatment outcomes of nasopharyngeal carcinoma in modern era after intensity modulated radiotherapy (IMRT) in Hong Kong: A report of 3328 patients (HKNPCSG 1301 study). Oral Oncol. 2018;77:16–21.
Ng WT, Corry J, Langendijk JA, Lee AWM, Mäkitie A, Mendenhall WM, et al. Current management of stage IV nasopharyngeal carcinoma without distant metastasis. Cancer Treat Rev. 2020;85: 101995.
Tang LL, Guo R, Zhang N, Deng B, Chen L, Cheng ZB, et al. Effect of radiotherapy alone vs radiotherapy with concurrent chemoradiotherapy on survival without disease relapse in patients with low-risk nasopharyngeal carcinoma: a randomized clinical trial. JAMA. 2022;328:728–36.
Sun XS, Liu SL, Luo MJ, Li XY, Chen QY, Guo SS, et al. The association between the development of radiation therapy, image technology, and chemotherapy, and the survival of patients with nasopharyngeal carcinoma: a cohort study from 1990 to 2012. Int J Radiat Oncol Biol Phys. 2019;105:581–90.
Wang F, Jiang C, Wang L, Yan F, Sun Q, Ye Z, et al. Influence of concurrent chemotherapy on locoregionally advanced nasopharyngeal carcinoma treated with neoadjuvant chemotherapy plus intensity-modulated radiotherapy: A retrospective matched analysis. Sci Rep. 2020;10:2489.
Liu L, Fei Z, Chen M, Zhao L, Su H, Gu D, et al. Induction chemotherapy plus concurrent chemoradiotherapy versus induction chemotherapy plus volumetric modulated arc therapy alone in the treatment of stage II-IVB nasopharyngeal carcinoma patients: a retrospective controlled study. Radiat Oncol. 2018;13:148.
Zhang L, Shan GP, Li P, Cheng PJ. The role of concurrent chemotherapy to intensity-modulated radiotherapy (IMRT) after neoadjuvant docetaxel and cisplatin treatment in locoregionally advanced nasopharyngeal carcinoma. Med Oncol. 2015;32:41.
Wei Z, Zhang Z, Luo J, Li N, Peng X. Induction chemotherapy plus IMRT alone versus induction chemotherapy plus IMRT-based concurrent chemoradiotherapy in locoregionally advanced nasopharyngeal carcinoma: a retrospective cohort study. J Cancer Res Clin Oncol. 2019;145:1857–64.
Li WF, Li YQ, Chen L, Zhang Y, Guo R, Zhang F, et al. Propensity-matched analysis of three different chemotherapy sequences in patients with locoregionally advanced nasopharyngeal carcinoma treated using intensity-modulated radiotherapy. BMC Cancer. 2015;15:810.
Lin S, Lu JJ, Han L, Chen Q, Pan J. Sequential chemotherapy and intensity-modulated radiation therapy in the management of locoregionally advanced nasopharyngeal carcinoma: experience of 370 consecutive cases. BMC Cancer. 2010;10:39.
Chen FP, Wen DW, Li F, Lin L, Kou J, Zheng WH, et al. The role of post-neoadjuvant chemotherapy tumor volume for prognostication and treatment guidance in loco-regionally advanced nasopharyngeal carcinoma. Cancers (Basel). 2019;11:1632.
Lee JY, Sun JM, Oh DR, Lim SH, Goo J, Lee SH, et al. Comparison of weekly versus triweekly cisplatin delivered concurrently with radiation therapy in patients with locally advanced nasopharyngeal cancer: A multicenter randomized phase II trial (KCSG-HN10-02). Radiother Oncol. 2016;118:244–50.
Kiyota N, Tahara M, Fujii H, Yamazaki T, Mitani H, Iwae S, et al. Phase II/III trial of post-operative chemoradiotherapy comparing 3-weekly cisplatin with weekly cisplatin in high-risk patients with squamous cell carcinoma of head and neck (JCOG1008). J Clin Oncol. 2020;38:6502.
Zheng Y, Han F, Xiao W, Xiang Y, Lu L, Deng X, et al. Analysis of late toxicity in nasopharyngeal carcinoma patients treated with intensity modulated radiation therapy. Radiat Oncol. 2015;10:17.
Lin YH, Huang TL, Chien CY, Chen HC, Hsu HC, Huang EY, et al. Pretreatment prognostic factors of survival and late toxicities for patients with nasopharyngeal carcinoma treated by simultaneous integrated boost intensity-modulated radiotherapy. Radiat Oncol. 2018;13:45.
Miao J, Wang L, Zhu M, Xiao W, Wu H, Di M, et al. Long-term survival and late toxicities of elderly nasopharyngeal carcinoma (NPC) patients treated by high-total- and fractionated-dose simultaneous modulated accelerated radiotherapy with or without chemotherapy. Oral Oncol. 2019;89:40–7.
McDowell LJ, Rock K, Xu W, Chan B, Waldron J, Lu L, et al. Long-term late toxicity, quality of life, and emotional distress in patients with nasopharyngeal carcinoma treated with intensity modulated radiation therapy. Int J Radiat Oncol Biol Phys. 2018;102:340–52.
Lee AW, Tung SY, Ngan RK, Chappell R, Chua DT, Lu TX, et al. Factors contributing to the efficacy of concurrent-adjuvant chemotherapy for locoregionally advanced nasopharyngeal carcinoma: combined analyses of NPC-9901 and NPC-9902 Trials. Eur J Cancer. 2011;47:656–66.
Peng H, Chen L, Zhang Y, Li WF, Mao YP, Zhang F, et al. Prognostic value of the cumulative cisplatin dose during concurrent chemoradiotherapy in locoregionally advanced nasopharyngeal Carcinoma: a secondary analysis of a prospective phase III clinical trial. Oncologist. 2016;21:1369–76.
Liu SL, Sun XS, Yan JJ, Chen QY, Lin HX, Wen YF, et al. Optimal cumulative cisplatin dose in nasopharyngeal carcinoma patients based on induction chemotherapy response. Radiother Oncol. 2019;137:83–94.
Zhang W, Chen Y, Chen L, Guo R, Zhou G, Tang L, et al. The clinical utility of plasma Epstein-Barr virus DNA assays in nasopharyngeal carcinoma: the dawn of a new era?: a systematic review and meta-analysis of 7836 cases. Medicine (Baltimore). 2015;94: e845.
Zhang J, Shu C, Song Y, Li Q, Huang J, Ma X. Epstein-Barr virus DNA level as a novel prognostic factor in nasopharyngeal carcinoma: A meta-analysis. Medicine (Baltimore). 2016;95: e5130.
Liu TB, Zheng ZH, Pan J, Pan LL, Chen LH. Prognostic role of plasma Epstein-Barr virus DNA load for nasopharyngeal carcinoma: a meta-analysis. Clin Invest Med. 2017;40:E1-e12.
Lee AWM, Lee VHF, Ng WT, Strojan P, Saba NF, Rinaldo A, et al. A systematic review and recommendations on the use of plasma EBV DNA for nasopharyngeal carcinoma. Eur J Cancer. 2021;153:109–22.
Buehrlen M, Zwaan CM, Granzen B, Lassay L, Deutz P, Vorwerk P, et al. Multimodal treatment, including interferon beta, of nasopharyngeal carcinoma in children and young adults: preliminary results from the prospective, multicenter study NPC-2003-GPOH/DCOG. Cancer. 2012;118:4892–900.
Casanova M, Bisogno G, Gandola L, Cecchetto G, Di Cataldo A, Basso E, et al. A prospective protocol for nasopharyngeal carcinoma in children and adolescents: the Italian Rare Tumors in Pediatric Age (TREP) project. Cancer. 2012;118:2718–25.
Mertens R, Granzen B, Lassay L, Bucsky P, Hundgen M, Stetter G, et al. Treatment of nasopharyngeal carcinoma in children and adolescents: definitive results of a multicenter study (NPC-91-GPOH). Cancer. 2005;104:1083–9.
Rodriguez-Galindo C, Wofford M, Castleberry RP, Swanson GP, London WB, Fontanesi J, et al. Preradiation chemotherapy with methotrexate, cisplatin, 5-fluorouracil, and leucovorin for pediatric nasopharyngeal carcinoma. Cancer. 2005;103:850–7.
Mai H-Q, Yang J-H, Guo S-S, Sun X-S, Liu L-Z, Yang Z-C, et al. Reduced-dose radiotherapy for pretreatment EBV DNA selected low-risk stage III nasopharyngeal carcinoma: A single-arm, phase II trial. J Clin Oncol. 2022;40:6002.
Ho FC, Tham IW, Earnest A, Lee KM, Lu JJ. Patterns of regional lymph node metastasis of nasopharyngeal carcinoma: a meta-analysis of clinical evidence. BMC Cancer. 2012;12:98.
Chen JZ, Le QT, Han F, Lu LX, Huang SM, Lin CG, et al. Results of a phase 2 study examining the effects of omitting elective neck irradiation to nodal levels IV and Vb in patients with N(0–1) nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 2013;85:929–34.
Tang L-L, Huang C-L, Zhang N, Jiang W, Wu Y-S, Huang SH, et al. Elective upper-neck versus whole-neck irradiation of the uninvolved neck in patients with nasopharyngeal carcinoma: an open-label, non-inferiority, multicentre, randomised phase 3 trial. Lancet Oncol. 2022;23(4):479–90.
Huang CL, Xu C, Zhang Y, Zhou GQ, Mao YP, Liu Q, et al. Feasibility of ipsilateral lower neck sparing irradiation for unilateral or bilateral neck node-negative nasopharyngeal carcinoma: systemic review and meta-analysis of 2, 521 patients. Radiat Oncol. 2018;13:141.
Cho WK, Oh D, Lee E, Kim TG, Lee H, Nam H, et al. Feasibility of Selective Neck Irradiation with Lower Elective Radiation Dose in Treating Nasopharynx Cancer Patients. Cancer Res Treat. 2019;51:603–10.
Li JG, Yuan X, Zhang LL, Tang YQ, Liu L, Chen XD, et al. A randomized clinical trial comparing prophylactic upper versus whole-neck irradiation in the treatment of patients with node-negative nasopharyngeal carcinoma. Cancer. 2013;119:3170–6.
Chen J, Ou D, He X, Hu C. Sparing level Ib lymph nodes by intensity-modulated radiotherapy in the treatment of nasopharyngeal carcinoma. Int J Clin Oncol. 2014;19:998–1004.
Li M, Huang XG, Yang ZN, Lu JY, Zhan YZ, Xie WJ, et al. Effects of omitting elective neck irradiation to nodal Level IB in nasopharyngeal carcinoma patients with negative Level IB lymph nodes treated by intensity-modulated radiotherapy: a Phase 2 study. Br J Radiol. 2016;89:20150621.
Ou X, Miao Y, Wang X, Ding J, He X, Hu C. The feasibility analysis of omission of elective irradiation to level IB lymph nodes in low-risk nasopharyngeal carcinoma based on the 2013 updated consensus guideline for neck nodal levels. Radiat Oncol. 2017;12:137.
Zhang F, Cheng YK, Li WF, Guo R, Chen L, Sun Y, et al. Investigation of the feasibility of elective irradiation to neck level Ib using intensity-modulated radiotherapy for patients with nasopharyngeal carcinoma: a retrospective analysis. BMC Cancer. 2015;15:709.
Zhao Y, Liao X, Wang Y, Lan W, Ren J, Yang N, et al. Level Ib CTV delineation in nasopharyngeal carcinoma based on lymph node distribution and topographic anatomy. Radiother Oncol. 2022;172:10–7.
Sun Y, Li WF, Chen NY, Zhang N, Hu GQ, Xie FY, et al. Induction chemotherapy plus concurrent chemoradiotherapy versus concurrent chemoradiotherapy alone in locoregionally advanced nasopharyngeal carcinoma: a phase 3, multicentre, randomised controlled trial. Lancet Oncol. 2016;17:1509–20.
Zhang Y, Chen L, Hu GQ, Zhang N, Zhu XD, Yang KY, et al. Gemcitabine and cisplatin induction chemotherapy in nasopharyngeal carcinoma. N Engl J Med. 2019;381:1124–35.
Zhang Y, Chen L, Hu GQ, Zhang N, Zhu XD, Yang KY, et al. Final overall survival analysis of gemcitabine and cisplatin induction chemotherapy in nasopharyngeal carcinoma: a multicenter, randomized phase III trial. J Clin Oncol. 2022;40:2420–5.
Lan XW, Xiao Y, Zou XB, Zhang XM, OuYang PY, Xie FY. Outcomes of adding induction chemotherapy to concurrent chemoradiotherapy for stage T3N0-1 nasopharyngeal carcinoma: a propensity-matched study. Onco Targets Ther. 2017;10:3853–60.
Xu C, Zhang S, Li WF, Chen L, Mao YP, Guo Y, et al. Selection and validation of induction chemotherapy beneficiaries among patients with T3N0, T3N1, T4N0 nasopharyngeal carcinoma using Epstein-Barr virus DNA: a joint analysis of real-world and clinical trial data. Front Oncol. 2019;9:1343.
Argiris A, Karamouzis MV. Empowering induction therapy for locally advanced head and neck cancer. Ann Oncol. 2011;22:773–81.
Langendijk JA, Leemans CR, Buter J, Berkhof J, Slotman BJ. The additional value of chemotherapy to radiotherapy in locally advanced nasopharyngeal carcinoma: a meta-analysis of the published literature. J Clin Oncol. 2004;22:4604–12.
Hui EP, Ma BB, Leung SF, King AD, Mo F, Kam MK, et al. Randomized phase II trial of concurrent cisplatin-radiotherapy with or without neoadjuvant docetaxel and cisplatin in advanced nasopharyngeal carcinoma. J Clin Oncol. 2009;27:242–9.
Chen YP, Tang LL, Yang Q, Poh SS, Hui EP, Chan ATC, et al. Induction chemotherapy plus concurrent chemoradiotherapy in endemic nasopharyngeal carcinoma: individual patient data pooled analysis of four randomized trials. Clin Cancer Res. 2018;24:1824–33.
Li WF, Chen NY, Zhang N, Hu GQ, Xie FY, Sun Y, et al. Concurrent chemoradiotherapy with/without induction chemotherapy in locoregionally advanced nasopharyngeal carcinoma: Long-term results of phase 3 randomized controlled trial. Int J Cancer. 2019;145:295–305.
Miao J, Wang L, Tan SH, Li JG, Yi J, Ong EHW, et al. Adjuvant capecitabine following concurrent chemoradiotherapy in locoregionally advanced nasopharyngeal carcinoma: a randomized clinical trial. JAMA Oncol. 2022;8(12):1776–85.
Hsu CL, Chang KP, Lin CY, Chang HK, Wang CH, Lin TL, et al. Plasma Epstein-Barr virus DNA concentration and clearance rate as novel prognostic factors for metastatic nasopharyngeal carcinoma. Head Neck. 2012;34:1064–70.
Wang WY, Twu CW, Chen HH, Jan JS, Jiang RS, Chao JY, et al. Plasma EBV DNA clearance rate as a novel prognostic marker for metastatic/recurrent nasopharyngeal carcinoma. Clin Cancer Res. 2010;16:1016–24.
An X, Wang FH, Ding PR, Deng L, Jiang WQ, Zhang L, et al. Plasma Epstein-Barr virus DNA level strongly predicts survival in metastatic/recurrent nasopharyngeal carcinoma treated with palliative chemotherapy. Cancer. 2011;117:3750–7.
Lv J, Chen Y, Zhou G, Qi Z, Tan KRL, Wang H, et al. Liquid biopsy tracking during sequential chemo-radiotherapy identifies distinct prognostic phenotypes in nasopharyngeal carcinoma. Nat Commun. 2019;10:3941.
Zhang B, Ouyang F, Gu D, Dong Y, Zhang L, Mo X, et al. Advanced nasopharyngeal carcinoma: pre-treatment prediction of progression based on multi-parametric MRI radiomics. Oncotarget. 2017;8:72457–65.
Zhang B, Tian J, Dong D, Gu D, Dong Y, Zhang L, et al. Radiomics Features of Multiparametric MRI as Novel Prognostic Factors in Advanced Nasopharyngeal Carcinoma. Clin Cancer Res. 2017;23:4259–69.
Zheng D, Chen Y, Chen Y, Xu L, Chen W, Yao Y, et al. Dynamic contrast-enhanced MRI of nasopharyngeal carcinoma: a preliminary study of the correlations between quantitative parameters and clinical stage. J Magn Reson Imaging. 2014;39:940–8.
Yu JY, Zhang D, Huang XL, Ma J, Yang C, Li XJ, et al. Quantitative analysis of DCE-MRI and RESOLVE-DWI for differentiating nasopharyngeal carcinoma from nasopharyngeal lymphoid hyperplasia. J Med Syst. 2020;44:75.
Kim S, Loevner L, Quon H, Sherman E, Weinstein G, Kilger A, et al. Diffusion-weighted magnetic resonance imaging for predicting and detecting early response to chemoradiation therapy of squamous cell carcinomas of the head and neck. Clin Cancer Res. 2009;15:986–94.
Chen YH, Chang KP, Chu SC, Yen TC, Wang LY, Chang JT, et al. Value of early evaluation of treatment response using (18)F-FDG PET/CT parameters and the Epstein-Barr virus DNA load for prediction of outcome in patients with primary nasopharyngeal carcinoma. Eur J Nucl Med Mol Imaging. 2019;46:650–60.
Ma B, Hui EP, King A, Leung SF, Kam MK, Mo F, et al. Prospective evaluation of plasma Epstein-Barr virus DNA clearance and fluorodeoxyglucose positron emission scan in assessing early response to chemotherapy in patients with advanced or recurrent nasopharyngeal carcinoma. Br J Cancer. 2018;118:1051–5.
Tsai MH, Shiau YC, Kao CH, Shen YY, Lin CC, Lee CC. Detection of recurrent nasopharyngeal carcinomas with positron emission tomography using 18-fluoro-2-deoxyglucose in patients with indeterminate magnetic resonance imaging findings after radiotherapy. J Cancer Res Clin Oncol. 2002;128:279–82.
Fang W, Zhang J, Hong S, Zhan J, Chen N, Qin T, et al. EBV-driven LMP1 and IFN-γ up-regulate PD-L1 in nasopharyngeal carcinoma: Implications for oncotargeted therapy. Oncotarget. 2014;5:12189–202.
Lee VH, Lo AW, Leung CY, Shek WH, Kwong DL, Lam KO, et al. Correlation of PD-L1 expression of tumor cells with survival outcomes after radical intensity-modulated radiation therapy for non-metastatic nasopharyngeal carcinoma. PLoS ONE. 2016;11: e0157969.
Zhu Q, Cai MY, Chen CL, Hu H, Lin HX, Li M, et al. Tumor cells PD-L1 expression as a favorable prognosis factor in nasopharyngeal carcinoma patients with pre-existing intratumor-infiltrating lymphocytes. Oncoimmunology. 2017;6: e1312240.
Larbcharoensub N, Mahaprom K, Jiarpinitnun C, Trachu N, Tubthong N, Pattaranutaporn P, et al. Characterization of PD-L1 and PD-1 expression and CD8+ tumor-infiltrating lymphocyte in Epstein-Barr virus-associated nasopharyngeal carcinoma. Am J Clin Oncol. 2018;41:1204–10.
Ono T, Azuma K, Kawahara A, Sasada T, Matsuo N, Kakuma T, et al. Prognostic stratification of patients with nasopharyngeal carcinoma based on tumor immune microenvironment. Head Neck. 2018;40:2007–19.
Wang YQ, Chen YP, Zhang Y, Jiang W, Liu N, Yun JP, et al. Prognostic significance of tumor-infiltrating lymphocytes in nondisseminated nasopharyngeal carcinoma: A large-scale cohort study. Int J Cancer. 2018;142:2558–66.
Acknowledgements
We thank all our families and the authors of literature in this review.
Publication statement
This study has not been submitted for consideration of publication elsewhere.
Disclaimers
None.
Funding
This work was supported by the Beijing hope run fund (grant number LC2021L06).
Author information
Authors and Affiliations
Contributions
Conception and design: Junlin Yi, Ziou Du, Shiyu Song, Yang Liu; Administrative support: Junlin Yi; Provision of study materials or patients: Junlin Yi, Ziou Du, Yang Liu; Manuscript writing: Yang Liu; Final approval of manuscript: All authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was considered exempt from the institutional review board of our hospital because it was a review of published literature.
Consent for publication
The authors consent to the publication of this paper.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, Y., Du, Z., Song, S. et al. Progress in the comprehensive treatment of nasopharyngeal carcinoma: a review for risk-stratified management strategies. Holist Integ Oncol 2, 19 (2023). https://doi.org/10.1007/s44178-023-00046-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44178-023-00046-9