Abstract
During the last decade, uterus transplantation has evolved as the first treatment for absolute uterine factor infertility, caused by absence of a functional uterus. Current challenges in the area of uterus transplantation are organ shortage and side effects of immunosuppression. These hurdles may be solved with novel tissue engineering technologies to produce a uterus from stem cells. For example, the development of patient-specific grafts using a biomaterial together with the patient’s own cells might be utilized for a partial uterus repair therapy or a whole bioengineered uterus might be developed to replace an allogeneic graft in a uterus transplantation setting. During recent years, uterus bioengineering strategies with scaffolds based on decellularized tissue have been particularly assessed. Decellularization protocols were established for both small and large animal models, including the human uterus. Promising in vivo results using such scaffolds to repair a partially injured uterus showed restoration of fertility in rodent models. Scaffold generation protocols and recellularization methodologies including various cell sources are currently being optimized and translated to more clinically relevant injury models in large animals. This review provides a summary of the progress made to date, based on use of decellularized uterine tissue for uterus repair.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
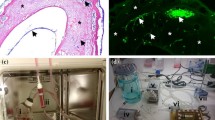
Assisted reproductive technologies made great achievements over the last decades. However, uterine factor infertility (UFI) still remains challenging to treat since general protocols still rely on a functional uterus. For these reasons, uterus transplantation (UTx) was introduced as a proposed treatment option and was proved successful by the first baby born after this procedure in 2014 [1, 2]. Despite this breakthrough in reproductive medicine and organ transplantation, risks related to live donor surgery and adverse side effects caused by immunosuppressive treatments following uterus engraftment justified the search for potential new donor sources with less negative side effects related to immunosuppression. Novel tissue engineering techniques may be an attractive option to overcome these limitations. For instance, a patient-specific uterus graft might be developed from a scaffold populated with the patient’s own cells. Such bioengineered grafting material would not require donor sources of living donors or multi-organ donors. Moreover, there would be no need for donor-recipient matching or immunosuppression following transplantation. Hence, the development of a transplantable bioengineered uterus may overcome some of the transplantation-related hurdles in UTx. Furthermore, bioengineered uterine tissue might be developed for uterus reconstructive surgery to treat various conditions of sub-infertility. For example, uterine tissue graft may be used to minimize scarring of the uterine wall after repeated surgeries to increase implantation success and reduce the risk for uterine rupture during a future pregnancy. Hence, the prospect of developing treatments for partial uterus repair using a bioengineered uterus tissue patch serves as a clinically relevant, intermediate objective to the more challenging long-term goal of developing a whole bioengineered uterus to replace a donor in a UTx setting (Fig. 1).
An ideal uterus scaffold should be immune tolerable, displays the normal anatomical structure, and has the biological characteristics that mimic the native tissue. The scaffold should also provide structural and functional support for the patient-derived cells. Scaffolds can be derived from either biological or synthetic materials and were successfully used in clinical applications for skin and bone regeneration [3]. However, more complex tissue and whole organs remain challenging to bioengineer. A popular strategy to construct scaffolds for bioengineering applications is a technique known as “decellularization.” This multi-step process usually involves chemical, physical, and/or enzymatic treatment of a donor tissue that result in the removal of immunoreactive intracellular components [4]. The remaining tissue-specific extracellular matrix (ECM) then serves as a biological three-dimensional (3D) scaffold with patent vascular conduits that facilitate future engraftment via vascular anastomosis. Cells of various origins may be added to this structure in a process called “recellularization.” These principles achieved promising results in whole-organ bioengineering studies on rodents for non-reproductive organs [3, 5,6,7,8,9], but was also assessed for novel infertility treatment applications [10]. There are several promising scaffold types evaluated for uterus bioengineering applications which is extensively summarized in a recent systematic review [11]. These include scaffolds derived from different hydrogels [12,13,14], and scaffolds derived from biodegradable polyglycolic acid (PGA) and poly-dl-lactide-co-glycolide (PLGA) polymers [15]. The present review focuses on the recent advancements in the field of uterus bioengineering, using scaffolds derived from decellularized tissue.
Decellularized Uterus Tissue in Small and Large Animal Models
Uterus Decellularization Protocols in Small Animal Models
Decellularization of small tissue pieces may be conducted by simply immersing the small tissue segments directly into the decellularization agents. This concept was applied on mouse uterus pieces (10 × 2 mm) which were decellularized by agitation in an SDS solution and in a DNase solution [16]. However, the most common procedure for uterus decellularization seems to be perfusing a donor uterus through its vasculature with detergents or other chemicals. The choices of detergent, chemicals, and the perfusion time are crucial for the scaffold quality since the decellularization reagents also affect the ECM. For example, sodium dodecyl sulfate (SDS), which is an effective and widely used ionic surfactant for organ decellularization, produces an ECM-derived scaffold with different biological and physical characteristics compared with a scaffold produced by a milder non-ionic detergent under the same conditions (e.g., Triton-X100). For these reasons, much of the earlier research on uterus bioengineering predominantly focused on optimizing novel decellularization protocols. During 2014, three different labs published, in total, seven decellularization protocols for rat uterus scaffold production [17,18,19]. Miyazaki and Maruyama used an SDS protocol that was originally optimized for whole-rat liver decellularization. This protocol also proved to be efficient for whole-rat uterus decellularization and resulted in a scaffold with low-donor DNA content, with a retained ECM structure and patent conduits for the vasculature that could be anastomosed [6, 18]. Santoso et al. developed three rat uterus decellularization protocols using either SDS, Triton-X100, or high hydrostatic pressure (HHP) [19]. Their results showed that all protocols could decellularize the uterus tissue. However, their SDS protocol proved more effective for the myometrial muscle layer decellularization, but less effective in the luminal epithelial cell layer. The Triton-X100 treatment showed similar results, even when Triton-X100 was perfused for a longer time. In contrast, the developed HPP protocol removed donor cells effectively. This protocol used physical forces to decellularize the tissue rather than chemical forces and was found favorable over the detergent-based protocols due to the shorter decellularization process and a better preservation of the protein content and mechanical properties [19]. Hellström et al. also published three protocols for rat uterus decellularization [17]. Two were based on a combination of Triton-X100 and the hypertonic solution dimethyl sulfoxide (DMSO). DMSO was reported to be an enhancer for penetration of detergents and may thus reduce the ECM exposure time for detergents during decellularization [20]. The two protocols only differed in a washing step: one protocol washed the scaffolds in a phosphate buffer solution and the other protocol used deionized water (dH2O). This difference had a profound effect on the amount of lingering donor DNA. The additional hypotonic exposure from the dH2O was a significant improvement for the decellularization efficiency. The third protocol evaluated by Hellström et al. was based on sodium deoxycholate (SDC) which is a considerably milder ionic detergent compared to, e.g., SDS. This protocol resulted in a similar scaffolding structure and biological composition as the Triton-X100/DMSO/dH2O protocol [17]. Additional rat uterus bioengineering studies have since been reported that were based on decellularized tissue, including a modified SDS/Triton-X100 protocol that resulted in similar scaffold types as previously explained [21]. The same combination was also used to decellularize the slightly larger rabbit uterus [22, 23]. Importantly, Campo et al. used proteomics analysis to convincingly show that the resulting scaffold was significantly improved if the donor rabbits were hormonally stimulated two days prior to donor organ procurement.
Uterus Decellularization Protocols in Large Animal Models
Uterus decellularization has also been studied in larger animal models. One study showed that the large pig uterus also could be decellularized using the combination of SDS and Triton-X100 [24]. The authors further investigated how the scaffold was affected from a freeze–thawing (F/T) event prior to the start of the decellularization process. F/T an organ/tissue can be considered as a part of the decellularization process since the physical forces during ice crystal formation cause cells to rupture that may increase the efficiency in the subsequent perfusion steps. Campo et al. did not find any noticeable concerns in the ECM architecture after the F/T. Nevertheless, F/T cycles should be used with consideration since such events could negatively affect the ECM morphology and compromise scaffold functionality. Inclusion of a freezing medium to prevent such events may be advantageous [25].
While the pig model is beneficial to study scaffold construction for large organs, the sheep is by many considered the best large animal model for uterus-related research. The sheep uterus is more like the human uterus in size and its vascular anatomy is also more similar. Furthermore, the sheep only produces 1–3 offspring per pregnancy. For these reasons, this animal model served as a crucial step toward establishing successful human UTx protocols [26, 27] and will likewise serve as an important animal model for the development of clinical uterus bioengineering protocols. This was also acknowledged by Daryabari et al., who developed three sheep uterus decellularization protocols. These were based on either a mild detergent (Triton-X100) or a strong detergent (SDS) or a combination of them [28]. Results from their extensive scaffold analysis made the authors conclude that their SDS protocol, which also included a formalin-based fixation step, seemed to be the best of the three optimized protocols. Tiemann et al. described three alternative decellularization protocols for whole-sheep uterus decellularization [29]. They reported that their most successful rat decellularization protocol (based on Triton-X100/DMSO/dH2O) did not work as efficiently on the sheep uterus. Hence, Triton-X100 was instead combined with SDC with the ambition to only use mild detergents in one of the protocols to preserve the ECM as much as possible. Two additional protocols based on either SDS or SDC were also evaluated. The study showed that all three protocols lead to a decellularized sheep uterus, but that the SDC-based protocol preserved the collagen structure and other ECM components better than the other two tested protocols [29].
Recellularization and Transplantation of Decellularized Uterus Tissue
With the growing general knowledge of how tissue and organs of various sizes may be decellularized, focus have now shifted toward how these scaffolds perform. This includes how well they harbor cells after recellularization in vitro and how these engineered grafts integrate and stimulate regeneration after transplantation in vivo.
Recellularization and Transplantation of Decellularized Tissue in Small Animal Models
Several in vivo studies in rodents showed promising results after the transplantation of small decellularized uterus segments (less than 1.5 × 0.5 cm in size) used to repair a partially injured uterus. Some of these studies grafted scaffolds without any further modifications or recellularization steps. For example, Santoso et al. evaluated their SDS- and HHP-derived rat uterus scaffolds one-month post-transplantation [19]. Rats were also mated at this time point and the results showed that both scaffold types stimulated uterus repair to such an extent that it was able to support pregnancy to full term. A different study evaluated how the topological orientation of acellular SDS-derived uterus scaffolds affected the outcomes after transplantation [30]. Interestingly, while the tissue morphology was negatively affected in the alternatively oriented scaffold grafts, the pregnancy outcome was unchanged. The same study also showed that grafts from decellularized intestinal tissue was not as beneficial, indicating the importance of tissue-specific factors for regeneration [30]. A mouse study showed that the regenerative response following decellularized uterus tissue transplantation was less dependent on the ovarian steroids, but rather dependent on signal transducer and activator of transcription 3 (STAT3) [16].
The results from these important studies are somewhat different from other studies in the sense that the uterus tissue was able to regenerate without a prior recellularization step before transplantation. Hellström et al. reported scaffold degeneration in acellular grafts, but regeneration and complete restoration of fertility when primary uterus cells and mesenchymal stem cells (MSCs) were added to the scaffolds before the reconstructive uterus surgery [31]. Difficulties in regeneration without prior recellularization of decellularized tissue have also been reported for other tissues, e.g., during rabbit urethral reconstruction [32]. These discrepancies between results of different studies might be explained by the different scaffold compositions generated from different decellularization protocols. Differences in collagen or elastin fibers, etc. may affect in vivo degeneration properties and endogenous cell regeneration mechanisms. Indeed, regenerative and functional discrepancies between scaffold types have been observed, where scaffolds derived from milder detergents (DMSO/Triton-X100/dH2O) were superior to an SDC-based protocol in both in vitro cell adherences and in vivo regeneration [31]. Additionally, the mechanical (and detergent excluding) HHP decellularization method for rat uterus scaffolds production resulted in efficient recellularization of rat endometrium stroma cells [33]. Further uterus scaffold differences were observed depending on the donor hormonal stage of the ovarian cycle [22]. In the latter study it was observed that the ECM composition was significantly different between scaffolds obtained from the non-proliferating (non-synchronous) and the proliferating endometrial tissue (synchronous with embryo implantation). This latter study is also a good example on how decellularized scaffolds may be further processed into a hydrogel that could be used as an in vitro substrate for embryos or injected into the luminal space in vivo to treat endometrial abnormalities [34, 35].
The scaffold degeneration time and longevity after transplantation is also dependent on the recipient’s immune system. The relationship between the immune response and tissue healing is a balanced orchestration as there are both positive and negative elements essential for graft survival and regeneration success. Two recent studies using the rat model investigated the immunological response toward decellularized uterus tissue [36, 37]. These studies showed that the decellularization process formed allogeneic-independent damage-associated molecular patterns (DAMPs) that are immunoreactive and trigger the immune response in the recipient, even between inbred strains. Their results showed that stronger detergents form higher levels of DAMPs that risk skewing the immune response toward a pro-inflammatory and anti-regenerative state. Such response would most likely degenerate a decellularized tissue graft faster than a scaffold type containing less DAMPs. The two studies suggested that the most favorable decellularization method for rat uterus included only mild detergents, yet resulted in donor DNA levels below 1% of the original levels to remain immune tolerant after transplantation [36, 37]. This is an important finding since the results suggest a more forgiving threshold than the strict decellularization criteria discussed in a highly cited review paper where a threshold of 50-ng DNA/mg dry scaffold weight is stated [38]. Use of exceedingly strict decellularization criteria may lead to an overuse of harsh chemicals during the scaffold production, which will compromise the functionality in downstream applications. Furthermore, immunoreactive scaffold properties can be modulated by cells used in the recellularization step prior to engraftment. For example, a study in the rat showed that significantly large uterine scaffolds recellularized with bone marrow-derived MSCs skewed the host immune system toward a regenerative state and that this positive effect lasted long after the donor cells had been removed [39]. However, additional research is needed to decipher these complex immune mechanisms that can dictate failure or success after decellularized tissue transplantation, particularly, when translating these principles to a clinical setting.
In the recent study by Yao et al., using decellularized rabbit uterine tissue, the authors chose a scaffold modification strategy to delay the degradation time of the decellularized tissue after transplantation [23]. The scaffolds were treated with either of the naturally derived crosslinking agents procranidins or genipin. The study then transplanted these modified acellular scaffolds in a rat model (xenograft) and found that both compounds significantly delayed the degradation time in vivo. This suggests that crosslinking may be a beneficial addition in the scaffold production to improve its mechanical strength and adjust the degradation time in vivo. These strategies might become especially favorable when developing large constructs, where the regeneration time is expected to be prolonged and thus, will require a more durable scaffolding structure. However, further studies on the properties of these crosslinking-modified scaffolds, including tests of immunogenicity, are needed.
Even if several groups have repeatedly shown advantageous uterus repair in rodent models after decellularized uterus tissue transplantation [16, 18, 19, 21, 30, 31] not all studies detailed the implantation/placentation site or mentioned if it occurred in the graft itself. Hence, more detailed studies on these important aspects are needed to elucidate whether the graft support implantation and placentation are fully functional. Furthermore, while most studies performed different histological examinations of the graft at various time points after transplantation, no studies chose to comprehensively evaluate and characterize the infiltration of host cells. The three recent studies investigating the immunological response toward decellularized material clearly showed the importance of including immune cell phenotype characterization after transplantation [36, 37, 39] since immune cells play a significant role in tissue regeneration. Nevertheless, the collective published data conclusively provide a solid research base to further develop uterus bioengineering principles and start to evaluate clinically relevant graft sizes in large animal models.
Recellularization of Decellularized Tissue in Large Animal Models
So far, decellularized uterus tissue from large animals have only been evaluated in vitro in various recellularization studies, except for a xenograft transplantation study of decellularized sheep uterus tissue in the rat model [28]. Acellular scaffolds were assessed histologically 10 days after transplantation and some infiltrated cells were positively stained for the proliferation marker Ki67, the vascular endothelial marker CD31, and the smooth muscle cell marker SMA. Campo et al. did not conduct any in vivo study; however, they clearly showed that the large pig uterus could be decellularized and the remaining scaffold could be recellularized using a mixture of human uterus epithelial and stromal cells [24]. These were cultured in vitro for 9–12 days and organoid-like structures were observed that were stained positive for vimentin and cytokeratin, denoting that human uterus cells could accommodate xenogeneic decellularized tissue. Recellularization studies have also been performed in the sheep model. Rings of decellularized sheep uterus tissue, including ECM from all uterine tissue layers, were seeded with fetal sheep MSCs by multiple injections and then cultured in vitro for 14 days. However, cells only remained in clusters at the injection sites and at the superficial layers of the scaffolds, demonstrating a significant and common general hurdle using decellularized tissue (independent of tissue type) and a limited in vitro recellularization efficiency [29]. For these reasons, a follow-up study was conducted by the same group to evaluate if further modification to the scaffold could increase the cell density. Scaffold preconditioning was conducted with matrix metalloproteinase (MMP) 2 and 9, which have been documented to be involved in the degradation of ECM proteins during cell migration [40]. This preconditining proved to reduce the collagen fiber thickness in the scaffolds by 30–40%, but the recellularization efficiency increased by 200–300% when they were cultured in Transwell® inserts [41]. These findings show the importance of developing enhanced culturing techniques to obtain cell-rich constructs. Future strategies will most likely also involve sophisticated perfusion bioreactors for large 3D tissue constructs.
Progress in Human Uterus Bioengineering with Decellularized Tissue
To our knowledge, the first human uterus tissue that was subjected to decellularization experiments was myometrial tissue segments, using a protocol based on ethanol, trypsin, and water [42]. The same protocol was also shown to be effective to decellularize myometrial tissue from the rat. These segments were then recellularized with human myometrial cells, which surprisingly were better at colonizing the rat uterus scaffolds, as compared to human myometrial scaffold. The cells formed a multilayered laminar structure on the rat scaffolds after 51 days in vitro [42]. A more recent study used the common combination of SDS and Triton-X100 to decellularize larger endometrial segments of human uteri. Recellularization of the decellularized endometrial tissue was conducted with human endometrial cells that showed functional phenotypic behavior by responding to a 28-day hormonal cycle that mimicked the human menstrual cycle [43]. This bioengineered explant culture may become an attractive in vitro model to better mimic in vivo physiological settings compared to standard 2D in vitro culturing systems to study processes in the human uterus, e.g., drug-dose response, invasive cancer mechanisms, or implantation events, in particular if combined with organ-on a-chip strategies [4, 11, 44, 45]. The organ-on-a-chip strategy utilizes a multi-channel microfluidic circuit system that connects several cell culture compartments containing cells of different phenotypes. This forms an in vitro environment that better mimics the communication between cells and organs in vivo.
Earlier this year, Daryabari et al. published the first study that utilized perfusion decellularization of a whole-human uterus [46]. Histological evaluation of the decellularized tissue demonstrated the removal of cellular components while maintaining important ECM molecules using an SDS-based protocol. Interestingly, the authors presented a protocol that used a relatively high detergent concentration and a long perfusion time compared to earlier published protocols on the sheep uterus. This indicates that protocols need to be developed and fine-tuned for every species and that decellularization protocols are not necessarily generic [17, 28, 29, 46]. Further evaluation of the decellularized human uterus was conducted using computed tomography (CT) angiography and showed that the vascular conduit network was well preserved. Scaffold biocompatibility was evaluated in a rat model for a partial uterus repair. Cell infiltration into the grafts were observed after 10 days and some cells were positive for the angiogenic and proliferative markers cluster of differentiation (CD) 31 and Ki67, respectively. Additional characterization of the infiltrated cells also showed that some cells were positive for uterus-related cytokeratin and smooth muscle cell actin markers. Based on immunohistochemistry, the MSCs-related chemoattractant C–X–C motif ligand (CXCL) 12 seemed elevated, while there was a reduction in C–X–C chemokine receptor type (CXCR) 4 and CXCR7 positivity. Previous studies have demonstrated that the relation between these proteins dictates regenerative processes by stem cell migration and proliferation [47]. Conclusively, the results showed that the human uterus can be decellularized and that the remaining ECM scaffold was able to activate important regenerative signals after transplantation in a xenograft model.
Conclusion and Future Perspectives
This review briefly summarizes the progress made using decellularized tissue for uterus bioengineering applications (Table 1). Whole-uterus decellularization protocols have been established for several species, including the human. The most common detergents used in these decellularization protocols are SDS, Triton-X100 and, to a lesser extent, SDC. However, several reports suggest that these decellularization protocols need to be optimized for each species and particular care needs to be considered so that DAMPs are kept to a minimum to reduce the immunogenicity of the created scaffold after transplantation. Collectively, regeneration of small uterine tissue defects has been successful in rodent models and the engineered grafts showed to be bioactive by the stimulation of angiogenesis and homing of endogenous stem cells. Despite these promising results, several obstacles remain to be solved. The recellularization techniques need to be further improved so that decellularized tissue may become appropriately repopulated prior to transplantation. Further improvement to the scaffolds might be needed to improve the recellularization efficiency, its biomechanical properties, and degradation properties in vivo. Most published work to date used relatively small graft sizes, indicating that there is a need for studies using more clinically relevant sized material and further assessment of functionality in vivo using large animal models. Another pertinent question is what cell source should be used for the reconstruction phase? It is plausible that a combination of various cell types will be needed, e.g., endothelial cells, endometrial stem/stroma cells, adipose-derived MSCs, and/or induced pluripotent stem cells. Importantly, a vast number of patient-derived cells would be required to recellularize a relevant sized graft for clinical use, and it is essential to consider how such methods can be established and scaled up to meet good manufacturing practice and appropriate quality control regulations.
References
M. Brännström, Uterus transplantation. Fertil. Steril. 99(2), 348–349 (2013). https://doi.org/10.1016/j.fertnstert.2012.10.020
M. Brännström et al., Livebirth after uterus transplantation. Lancet 385(9968), 607–616 (2015). https://doi.org/10.1016/s0140-6736(14)61728-1
P.M. Baptista et al., Whole organ decellularization—a tool for bioscaffold fabrication and organ bioengineering. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2009, 6526–6529 (2009). https://doi.org/10.1109/iembs.2009.5333145
M. Hellström, S. Bandstein, M. Brännström, Uterine tissue engineering and the future of uterus transplantation. Ann. Biomed. Eng. 45(7), 1718–1730 (2017). https://doi.org/10.1007/s10439-016-1776-2
H.C. Ott et al., Perfusion-decellularized matrix: using nature’s platform to engineer a bioartificial heart. Nat. Med. 14(2), 213–221 (2008). https://doi.org/10.1038/nm1684
B.E. Uygun et al., Organ reengineering through development of a transplantable recellularized liver graft using decellularized liver matrix. Nat. Med. 16(7), 814–820 (2010). https://doi.org/10.1038/nm.2170
H.C. Ott et al., Regeneration and orthotropic transplantation of a bioartificial lung. Nat. Med. 16(8), 927–933 (2010). https://doi.org/10.1038/nm.2193
T.H. Petersen et al., Tissue-engineered lungs for in vivo implantation. Science 329(5991), 538–541 (2010). https://doi.org/10.1126/science.1189345
J.J. Song et al., Regeneration and experimental orthotopic transplantation of a bioengineered kidney. Nat. Med. 19(5), 646–651 (2013). https://doi.org/10.1038/nm.3154
A.M. Padma, M. Brännström, M. Hellström, Uterus bioengineering as a future alternative to uterus transplantation. CEOG 49(3), 72 (2022). https://doi.org/10.31083/j.ceog4903072
E. Francés-Herrero et al., Bioengineering trends in female reproduction: a systematic review. Hum. Reprod. Update (2022). https://doi.org/10.1093/humupd/dmac025
L. Ding et al., Transplantation of bone marrow mesenchymal stem cells on collagen scaffolds for the functional regeneration of injured rat uterus. Biomaterials 35(18), 4888–4900 (2014). https://doi.org/10.1016/j.biomaterials.2014.02.046
X. Li et al., Regeneration of uterine horns in rats by collagen scaffolds loaded with collagen-binding human basic fibroblast growth factor. Biomaterials 32(32), 8172–8181 (2011). https://doi.org/10.1016/j.biomaterials.2011.07.050
L. Xu et al., Umbilical cord-derived mesenchymal stem cells on scaffolds facilitate collagen degradation via upregulation of MMP-9 in rat uterine scars. Stem Cell Res. Ther. 8(1), 84 (2017). https://doi.org/10.1186/s13287-017-0535-0
R.S. Magalhaes et al., A tissue-engineered uterus supports live births in rabbits. Nat. Biotechnol. 38(11), 1280–1287 (2020). https://doi.org/10.1038/s41587-020-0547-7
T. Hiraoka et al., STAT3 accelerates uterine epithelial regeneration in a mouse model of decellularized uterine matrix transplantation. JCI Insight (2016). https://doi.org/10.1172/jci.insight.87591
M. Hellstrom et al., Towards the development of a bioengineered uterus: comparison of different protocols for rat uterus decellularization. Acta Biomater. 10(12), 5034–5042 (2014). https://doi.org/10.1016/j.actbio.2014.08.018
K. Miyazaki, T. Maruyama, Partial regeneration and reconstruction of the rat uterus through recellularization of a decellularized uterine matrix. Biomaterials 35(31), 8791–8800 (2014). https://doi.org/10.1016/j.biomaterials.2014.06.052
E.G. Santoso et al., Application of detergents or high hydrostatic pressure as decellularization processes in uterine tissues and their subsequent effects on in vivo uterine regeneration in murine models. PLoS ONE 9(7), e103201 (2014). https://doi.org/10.1371/journal.pone.0103201
S. Guler et al., Improvement of decellularization efficiency of porcine aorta using dimethyl sulfoxide as a penetration enhancer. Artif. Organs 42(2), 219–230 (2018). https://doi.org/10.1111/aor.12978
X. Li et al., Reconstruction of functional uterine tissues through recellularizing the decellularized rat uterine scaffolds by MSCs in vivo and in vitro. Biomed. Mater. 16(3), 035023 (2021). https://doi.org/10.1088/1748-605X/abd116
H. Campo et al., Tissue-specific decellularized endometrial substratum mimicking different physiological conditions influences in vitro embryo development in a rabbit model. Acta Biomater. 89, 126–138 (2019). https://doi.org/10.1016/j.actbio.2019.03.004
Q. Yao et al., Exploiting crosslinked decellularized matrix to achieve uterus regeneration and construction. Artif. Cells Nanomed. Biotechnol. 48(1), 218–229 (2020). https://doi.org/10.1080/21691401.2019.1699828
H. Campo et al., De- and recellularization of the pig uterus: a bioengineering pilot study. Biol. Reprod. 96(1), 34–45 (2017). https://doi.org/10.1095/biolreprod.116.143396
S.E. Pors et al., Initial steps in reconstruction of the human ovary: survival of pre-antral stage follicles in a decellularized human ovarian scaffold. Hum. Reprod. 34(8), 1523–1535 (2019). https://doi.org/10.1093/humrep/dez077
W. Andraus et al., Sheep model for uterine transplantation: the best option before starting a human program. Clinics (Sao Paulo) 72(3), 178–182 (2017). https://doi.org/10.6061/clinics/2017(03)08
P. Dahm-Kähler et al., Transplantation of the uterus in sheep: methodology and early reperfusion events. J. Obstet. Gynaecol. Res. 34(5), 784–793 (2008). https://doi.org/10.1111/j.1447-0756.2008.00854.x
S.S. Daryabari et al., Development of an efficient perfusion-based protocol for whole-organ decellularization of the ovine uterus as a human-sized model and in vivo application of the bioscaffolds. J. Assist. Reprod. Genet. 36(6), 1211–1223 (2019). https://doi.org/10.1007/s10815-019-01463-4
T.T. Tiemann et al., Towards uterus tissue engineering: a comparative study of sheep uterus decellularisation. Mol. Hum. Reprod. 26(3), 167–178 (2020). https://doi.org/10.1093/molehr/gaaa009
F. Miki et al., The orientation of a decellularized uterine scaffold determines the tissue topology and architecture of the regenerated uterus in rats. Biol. Reprod. 100(5), 1215–1227 (2019). https://doi.org/10.1093/biolre/ioz004
M. Hellström et al., Bioengineered uterine tissue supports pregnancy in a rat model. Fertil. Steril. 106(2), 487-496.e1 (2016). https://doi.org/10.1016/j.fertnstert.2016.03.048
R.P. Dorin et al., Tubularized urethral replacement with unseeded matrices: what is the maximum distance for normal tissue regeneration? World J. Urol. 26(4), 323–326 (2008). https://doi.org/10.1007/s00345-008-0316-6
N. Charoensombut et al., Internal radial perfusion bioreactor promotes decellularization and recellularization of rat uterine tissue. J. Biosci. Bioeng. 133(1), 83–88 (2022). https://doi.org/10.1016/j.jbiosc.2021.09.007
S. López-Martínez et al., A natural xenogeneic endometrial extracellular matrix hydrogel toward improving current human in vitro models and future in vivo applications. Front. Bioeng. Biotechnol. 9, 639688 (2021). https://doi.org/10.3389/fbioe.2021.639688
S. Lopez-Martinez et al., Bioengineered endometrial hydrogels with growth factors promote tissue regeneration and restore fertility in murine models. Acta Biomater. 135, 113–125 (2021). https://doi.org/10.1016/j.actbio.2021.08.025
A.M. Padma et al., Immune response after allogeneic transplantation of decellularized uterine scaffolds in the rat. Biomed. Mater. (2021). https://doi.org/10.1088/1748-605X/abfdfe
A.M. Padma et al., Decellularization protocol-dependent damage-associated molecular patterns in rat uterus scaffolds differentially affect the immune response after transplantation. J. Tissue Eng. Regen. Med. 15(7), 674–685 (2021). https://doi.org/10.1002/term.3217
P.M. Crapo, T.W. Gilbert, S.F. Badylak, An overview of tissue and whole organ decellularization processes. Biomaterials 32(12), 3233–3243 (2011). https://doi.org/10.1016/j.biomaterials.2011.01.057
E. Sehic et al., Mesenchymal stem cells establish a pro-regenerative immune milieu after decellularized rat uterus tissue transplantation. J. Tissue Eng. 13, 20417314221118856 (2022). https://doi.org/10.1177/20417314221118858
G.A. Cabral-Pacheco et al., The roles of matrix metalloproteinases and their inhibitors in human diseases. Int. J. Mol. Sci. (2020). https://doi.org/10.3390/ijms21249739
A.M. Padma et al., Towards a bioengineered uterus: bioactive sheep uterus scaffolds are effectively recellularized by enzymatic preconditioning. NPJ Regen. Med. 6(1), 26 (2021). https://doi.org/10.1038/s41536-021-00136-0
R.C. Young, G. Goloman, Allo- and xeno-reassembly of human and rat myometrium from cells and scaffolds. Tissue Eng Part A 19(19–20), 2112–2119 (2013). https://doi.org/10.1089/ten.TEA.2012.0549
S.A. Olalekan et al., Development of a novel human recellularized endometrium that responds to a 28-day hormone treatment. Biol. Reprod. 96(5), 971–981 (2017). https://doi.org/10.1093/biolre/iox039
S.R. Park et al., Development of a novel dual reproductive organ on a chip: recapitulating bidirectional endocrine crosstalk between the uterine endometrium and the ovary. Biofabrication (2020). https://doi.org/10.1088/1758-5090/abbd29
J. Ahn et al., Three-dimensional microengineered vascularised endometrium-on-a-chip. Hum. Reprod. 36(10), 2720–2731 (2021)
S.S. Daryabari et al., Whole-organ decellularization of the human uterus and in vivo application of the bio-scaffolds in animal models. J. Assist. Reprod. Genet. 39(6), 1237–1247 (2022). https://doi.org/10.1007/s10815-022-02492-2
X. Wang et al., Chemoattraction of bone marrow-derived stem cells towards human endometrial stromal cells is mediated by estradiol regulated CXCL12 and CXCR4 expression. Stem Cell Res. 15(1), 14–22 (2015). https://doi.org/10.1016/j.scr.2015.04.004
Acknowledgements
We thank the reviewers for their time and valuable comments.
Funding
Open access funding provided by University of Gothenburg. The authors receive financial support to conduct uterus bioengineering research by the Knut and Alice Wallenberg foundation, the Swedish research council (VR: 116008), the ALF-agreement (between the Swedish government and the county council), the Adlerbertska, Hjalmar Svensson, and Wilhelm & Martina Lundgrens research foundations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sehic, E., Brännström, M. & Hellström, M. Progress in Preclinical Research on Uterus Bioengineering That Utilizes Scaffolds Derived from Decellularized Uterine Tissue. Biomedical Materials & Devices 1, 66–73 (2023). https://doi.org/10.1007/s44174-022-00036-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44174-022-00036-x