Abstract
Background
Poor hand hygiene (HH) among health care workers (HCWs) in low-resource healthcare settings has continued to increase the spread of infectious diseases, including COVID-19. The present study aimed to assess the knowledge, attitude, adherence, and barriers to HH practices among HCWs during the COVID-19 pandemic in Nigeria.
Methods
The study was an online cross-sectional survey using a tailored questionnaire distributed through chain referral sampling among southern Nigerian HCWs during the first wave of the COVID-19 pandemic (February to August 2020). The primary outcomes were knowledge, attitude, adherence to HH guidelines, and the barriers limiting compliance with the guidelines. Data were analysed using percentage, frequency, mean, standard deviation, one-way ANOVA, and multiple linear regression. The study timeline was from 15 April to 31 July 2020.
Results
Four hundred and fifty-four HCWs (236 males and 218 females) participated in the study. The participants had a moderate knowledge of standard HH protocol (mean ± SD) 62.45 ± 10.82%, positive attitude 84.34 ± 11.32%, and high adherence to the standard guidelines 81.21 ± 9.49%. There was no significant difference in knowledge, attitude, and adherence across the healthcare professions. Increasing age (β = 0.186, p < 0.003) and knowledge (β = 0.229, p < 0.001), and decreasing negligence (β = − 0.178, p = 0.004), and forgetfulness (β = − 0.159, p = 0.012) were the significant predictors of effective HH practices.
Conclusion
Nigerian HCWs had moderate knowledge, a positive attitude, and adhered to the standard HH practices during the COVID-19 pandemic. However, the major barriers were institutional-based factors such as the inadequate supply of HH items, competing job demands, emergencies, increased workload, and personal characteristics such as age, poor knowledge, negligence, and forgetfulness. We recommend that hospital management provide their staff with adequate HH materials and continued infectious disease training.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Highly virulent diseases such as COVID-19 can be spread in the community through the contact of uninfected persons with infected healthcare facilities (nosocomial infection) or by infectious health care workers (HCWs) during an unrelated health procedure (iatrogenic infection) [1,2,3]. Without proper hand hygiene (HH), unsuspecting HCWs could contract the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) by touching undiagnosed patients and contaminated hospital fomites and move on spreading the virus in the community [4,5,6]. Even with the advent of vaccination, the World Health Organization (WHO) still recommends regular HH to effectively curb SARS-CoV-2 transmission among the general population, including the HCWs [7]. However, there was a wide gap in adherence to HH among HCWs, ranging from 9% in low-income countries to 70% in high-income countries [8].
A single-centre study reported poor HH adherence (31%) among the HCWs in a northern Nigerian tertiary hospital [9]. Nigerian HCWs were also hesitant to vaccine uptake [10]. Additionally, their HH can be hampered by traditional institutional barriers in low-resource settings, such as an inadequate supply of aseptic materials, infrastructure deficit, managerial inefficiency, and poor awareness and funding [11, 12]. Nonetheless, HH is a simple, effective, and economical way of preventing the spread of infectious diseases [12, 13]. When soap and water are unavailable, alcohol-based hand rubs (ABHR) may be used [7, 14].
Proper HH involves using soap and running water or ABHR [15, 16] to effectively clean the hands for about 15–30 s [14, 17]. The WHO explained five critical moments in which HCWs must practice HH: before and after touching a patient, before sterile or aseptic procedures, after touching patient surroundings, and after exposure to body fluids [18]. Kampf et al. [19] posited that proper HH, especially ABHR, can reduce the hospital-associated (nosocomial) infection rate by 40%. Therefore, advocacy of HH practices remains a crucial measure to reduce the rate of hospital-associated infections in low-resource settings, such as Nigeria. A survey on the facilitators and barriers of these practices would provide evidence for strategic infection prevention and control.
This study is grounded in the health belief theory, which postulated that a low perception of health risk may lead to a lag in positive behavioural changes [20]. The findings were discussed using the psycho-behavioural (health belief) framework, which linked persons’ belief in the personal threat of disease and the effectiveness of the standard precautions to their likelihood of adherence to the desired behavioural changes. We conceptualised HCWs’ disposition to HH using the six constructs of the health belief model: perceived susceptibility (HCWs are very susceptible to the virulent SARS-CoV-2 due to the nature of their work), perceived severity (COVID-19 is a life-threatening disease), perceived benefits (adherence to the guidelines will limit HCWs’ risk of infection), perceived barriers (inadequate HH materials in low-resource settings), cue to action (research, conducive work environment, and enforcement), and self-efficacy (knowledge and attitude). Therefore, this study aimed to assess the knowledge, attitude, adherence, and barriers to HH practices among HCWs during the COVID-19 pandemic in Nigeria.
These research questions guided the study: (1) What are the participants’ levels of knowledge, attitude, and adherence to HH guidelines? (2) What are the participants’ sources of HH guidelines? (3) What are the barriers to HH guideline adherence? (4) Is there any significant difference in the levels of knowledge, attitude, and adherence to HH guidelines across health care professions? (5) Which sociodemographic and professional factors can predict HH adherence among the participants?
2 Methods
2.1 Study design
This study was an online cross-sectional survey of 454 HCWs in southern Nigeria between April 15 and July 31, 2020. The study was conducted in adherence to the ethical principles of the Declaration of Helsinki [21] and reported in line with Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [22].
2.2 Participants, setting, and eligibility criteria
The participants were doctors, nurses, physiotherapists, radiographers, medical laboratory scientists, and public health workers involved in patient care during the COVID-19 pandemic in Nigeria. Nigeria, with a population estimate of over 200 million, is the most populated country in Africa and the most populous black nation in the world [23]. Studies have shown that most Nigerian frontline HCWs were seropositive with SARS-CoV-2 during the pandemic [24], and about 38% were asymptomatic [25].
The inclusion criteria were being a frontline HCW in a tertiary or secondary health care setting, including federal, state, and private hospitals, domiciliary and faith-based outreaches during the first wave of the pandemic and being able and willing to sign the informed consent and complete the online survey. Participants were excluded if they were not involved in patient care during the pandemic or under 18 years old.
2.3 Sample size estimation
We targeted a sample size of 305 participants based on a priori calculation using the G*Power 3.1.9.4 software. The parameters were 17-predictor multiple linear regression, a moderate effect size of 0.1, an error probability of 0.05, and 95% power. G*Power software ensures an accurate sample size estimation that will obtain appropriate statistical power [26].
2.4 Sampling and bias
The authors shared the survey link with the health care professional bodies in Nigeria with an appeal to snowball the link through their email list and social media platforms. All HCWs registered with the professional bodies had equal opportunity to participate in the study. Snowballing sampling, or chain referral sampling, is a non-probability sampling method where participants are recruited through referrals from existing participants within a professional network [27]. The online snowballing technique was successful in surveying HCWs’ practices during the COVID-19 pandemic [3].
2.5 Research instrument
The instrument was developed from the WHO’s HH knowledge and perception questionnaire for HCWs [28], and the items on attitude, practices, and barriers to adherence to the guidelines were formulated through an in-depth literature review [9, 13, 17, 19, 29, 30]. Six psychometrics and public health experts completed the questionnaire’s face and content validity through email exchanges [31]. The validated instrument was hosted online and pilot-tested among 30 HCWs to ensure the clarity of questions and assess for possible programming errors that may become evident during the main survey. The internal consistency (Cronbach’s alpha) for each questionnaire domain ranged from 0.67 to 0.84, and the cut-off for acceptability was 0.5.
The final version of the questionnaire comprised 40 items arranged under five sections: sociodemographic characteristics (6 items), knowledge (14 items), attitude (6 items), adherence (13 items), and barriers to HH practices (1 item). The knowledge domain comprised multiple-choice questions (MCQs) with scores range 0 to 26. The attitude domain comprised 5-point Likert-scale questions with scores range 6 to 30. The adherence was measured with 5-point Likert-scale questions with scores range 13 to 65. One MCQ with 10 options was used to collect information on the barriers to HH adherence. Knowledge, attitude, and adherence domains were converted to percentages [32].
2.6 Procedure for data collection
We hosted the questionnaire as a Google form between 15 April and 31 July 2020 (107 days). The cover page contained informed consent information. Participants were instructed to read and endorse the consent form to proceed with the survey; otherwise, they may decline consent and exit the questionnaire [33].
We contacted the health professional associations in Nigeria to email all their members the introductory message and survey link, including an appeal to send them reminders at specific intervals. The web link was equally snowballed through the health professional body’s social media platforms such as WhatsApp, Facebook, Telegram, and Twitter [3]. The email recipients were sent reminders on three successive weekends. At the end of the study, the dataset was downloaded in a spreadsheet file format and stored in a password-encrypted device until ready for analysis.
2.7 Variables
Continuous variables were knowledge, attitude, and adherence to HH, measured in percentages. For knowledge and adherence, scores were classified as low (0 to 50%), moderate (51 to 74%), and high (75 to 100%). Attitude scores below 50% were considered negative, while 50% and above were considered positive [3]. Barriers to HH were obtained as nominal variables.
2.8 Data analysis
The survey data was analysed using Statistical Package for the Social Sciences (SPSS) software version 26 (SPSS, Chicago, IL, USA). We replaced the 2.3% missing data in the attitude domain using series mean substitution [34]. Descriptive statistics such as frequency, percentage, mean, and standard deviation were used to summarise the participants’ demographic characteristics and levels of knowledge, attitude, and adherence. The data were diagnosed and fixed for univariate (standardised Z-score test > ± 3.29) and multivariate outliers (Mahalanobis distance test), normality (Kolmogorov–Smirnov test), homoscedasticity (Levene’s test), linearity (Q-Q plot) and multicollinearity (tolerance factor), respectively. Inferential statistics—one-way-ANOVA was used to determine any significant mean differences in the knowledge, attitude, and adherence scores across the health professions. A forward stepwise, multiple linear regression was used to determine the demographic and practice characteristics that influenced adherence to HH guidelines. The tested predictors are shown in the footnote of Table 3. The alpha level was set at 0.05.
2.9 Ethics approval
The study protocol was approved by the Human Research Ethics Committees of the Faculty of Health Sciences and Technology, Nnamdi Azikiwe University, Anambra, Nigeria (MRH/NAU/FHST/2023/3).
3 Results
3.1 Participants’ demographic characteristics
The study involved 454 HCWs aged (mean ± SD) 35.92 ± 9.63, comprising 52.0% males and 48.0% females working in southern Nigeria during the first wave of the COVID-19 pandemic. Most of the participants were physiotherapists (54.6%) and doctors (21.1%) who had practised for 1 to 10 years (67.4%). The participants’ demographic characteristics were shown in Table 1.
3.2 Levels of knowledge, attitude, and adherence to standard HH
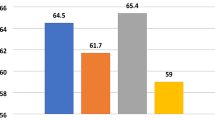
Generally, the participants’ knowledge of standard HH protocol (62.45 ± 10.82%) was moderate. The public health workers and physiotherapists appeared to have higher knowledge scores, 63.53 ± 8.89% and 63.40 ± 10.93%, respectively. Public health workers are paramedics, including vaccinators, nutritionists, and sanitarians who practise in communities to implement public health interventions. However, the one-way ANOVA result (Table 2) showed no significant difference in knowledge across the designations, F (5, 448) = 1.059, p = 0.384.
Across the designations, participants had a positive attitude (84.34 ± 11.32%) towards adherence to the standard HH protocol. The medical doctors (86.10 ± 8.60%) had a more positive attitude than other HCWs. However, the one-way ANOVA result (Table 2) showed no significant difference in attitude across the designations, F (5, 448) = 1.724, p = 0.130.
The overall participants’ mean adherence to the standard HH protocol (81.21 ± 9.49) was high. The medical laboratory scientists and public health workers had higher mean adherence to the standard HH protocol, 83.67 ± 10.79 and 83.06 ± 12.15, respectively. However, similar to knowledge and attitude, there was no significant difference in adherence across the designations, F (5, 448) = 1.658, p = 0.146.
3.3 Source of HH information
Figure 1 shows the frequency distribution of sources of information about proper HH. The topmost sources were social media 364 (80.2%), television 318 (70.0%), online news platforms 266 (58.6%), and hospital training/seminars 262 (57.7%). None of the participants reported the WHO guidelines as their direct source of information on HH.
3.4 Barriers to adherence to standard HH during the pandemic
Figure 2 shows the common barriers to HH among the participants. The top three barriers to proper HH adherence were an inadequate provision of aseptic materials 252 (55.5%), working under emergency conditions 122 (26.9%), and a heavy workload 104 (22.9%). A heavy workload involves managing too many patients concurrently, while working under emergency conditions refers to providing immediate care to patients in critical condition, often without prior appointments.
3.5 Predictors of adherence to standard HH during the pandemic
A forward stepwise entry, linear multiple regression (Table 3), was used to determine the most significant sociodemographic factors and barriers associated with HH practices. The result shows that increasing knowledge (β = 0.229, p < 0.001) and participants’ age (β = 0.186, p < 0.003) and decreasing negligence (β = − 0.178, p = 0.004) and forgetfulness (β = − 0.159, p = 0.012) were the significant predictors of maintaining good HH practices. Items excluded from the model were shown in the footnote of Table 3. The overall model was significant, F (4, 447) = 12.418, p < 0.001, and accounted for 16.9% of the total variance in HH compliance (Adjusted R2).
4 Discussion
The study aimed to determine the levels of knowledge, attitude, adherence, and barriers to proper HH among HCWs in Nigeria. We also explored the sources of HH information and sociodemographic and professional factors associated with HH adherence. The findings showed that, on average, participants had moderate knowledge and positive attitudes towards HH, alongside a high level of compliance, with no significant difference across HCW designations. The primary sources of information on HH were media and hospital seminars rather than direct personal access to the WHO guidelines. The main barriers to HH adherence were inadequate supply of aseptic materials, work overload, and emergency conditions. HCWs who were younger, less knowledgeable about the guidelines, or prone to negligence or forgetfulness were found to be at a higher risk of poor HH compliance.
Our findings aligned with a previous study, which showed that Malaysian nurses had moderate HH knowledge [35]. Studies have shown that a high knowledge of proper HH and an understanding of the risks associated with poor adherence to the guidelines increased during the COVID-19 pandemic [1, 16, 36, 37]. It could be deduced from the health belief model that the increase in risk perception among HCWs during the pandemic caused positive behavioural responses [6, 11]. The pandemic was overwhelming for healthcare systems in low-resource settings [23, 38]. Emergency responses were prioritised over staff training. Only about half of our participants received their HH information through in-hospital seminars. Anecdotally, hospital seminars incorporate valid and reliable local and international guidelines, such as the WHO HH guidelines. Some HCWs depended on the proliferation of information in media spaces to fill the training gaps [39, 40]. Similar to our findings, it was reported that social media provided a valuable means of bridging the knowledge-to-practice gap as information disseminated through them has a wider and faster reach, especially among young practitioners [39, 40]. However, social media misinformation and disinformation have raised concerns warranting health care agencies to counteract the deleterious effect proactively and for individuals to crosscheck information received on social media with other sources [41].
The result further showed that Nigerian HCWs had a positive attitude towards HH, leading to high compliance with the protocol. This finding is consistent with other studies, which showed that HCWs had positive attitudes towards HH and adhered to its protocol regularly [11, 17, 29, 35]. The nonsignificant difference in knowledge, attitude, and adherence to standard HH protocol across the professional categories proves that all HCWs were equally conscious of protecting themselves from COVID-19 and curtailing the chances of spreading the virus. It is unclear whether this positive attitude will be carried over to routine clinical practices post-pandemic. Health belief theorists suggest that a short-term acquired behavioural change can be reversed if the perceived risk is reduced [42]. Then, it is unclear how long the gains in HH would outlive the pandemic. Data collected after the pandemic's peak showed diminishing levels of HH compliance [5, 43]. Beyond the personal factors, the dearth of organisational cues continues to hamper safe HH in the low-resource setting [5, 11, 12, 36].
Despite having a positive attitude towards HH, the major barriers to its practice were institution-based: inadequate provision of HH materials, insufficient time or emergencies, and a heavy workload. Similarly, Ahmadipour et al. [36] reported that organisational factors such as improperly designed wards, lack of equipment and a heavy workload were among the major barriers to HCWs’ compliance with HH. Many hospitals faced a scarce supply of HH items, among other personal protective equipment, during the pandemic [5, 12]. The scarcity of these items during the pandemic, inadequate healthcare funding, and poor maintenance attitude, as reported in previous African studies [5, 9, 30] may have resulted in the inadequate provision, constituting a barrier to compliance with HH. Also, the workload during the COVID-19 pandemic increased as more patients were admitted to the hospital [23, 38], creating an emergency situation that affected proper hygiene before transitioning from one patient to another [38]. Similar to our findings, other studies have reported that a heavy workload, insufficient time, urgency, forgetfulness, and outright negligence were associated with poor HH practices [43, 44].
Among all the demographic characteristics, age positively predicted the HCWs’ HH practice, suggesting that being old is associated with better HH practices. Older HCWs may have more experience with hospital-related infections [45], making them comply better with standard HH during the COVID-19 pandemic. Older HCWs have more administrative roles and less clinical workloads. Moreover, the report that older people were more likely to get sick from COVID-19 may have ensured better HH practices among older cohorts. Effective HH with soap and water reduces the risk of cross-transmission of microorganisms in the hospital, particularly during the COVID-19 pandemic [13, 37]. Poor HH compliance of HCWs may lead to hospital-acquired infections for non-carrier patients, cross-transmission among HCWs, unsafe hospitals, and economic loss due to higher morbidity and mortality rates [37, 46].
4.1 Limitation
Self-reported information on HH practices among HCWs during the pandemic may be susceptible to social desirability bias. HCWs may report better practice than habitual practice in line with their job roles and expectations. Secondly, the use of a non-probability sampling method may limit the generalizability of the findings. Calculation of response rate is difficult with the snowballing recruitment technique. The sample was dominated by physiotherapists who are allied health workers. Demand for primary care was very high during the first wave of the pandemic; doctors, nurses, and diagnostic professionals were overwhelmed with clinical services and had less time to snowball the survey among their networks. Therefore, there could be nonresponse bias from the underrepresented sub-populations.
5 Conclusion
Nigerian HCWs had moderate knowledge of the standard COVID-19 HH practices. The HCWs displayed a positive attitude towards these practices and adhered to the standard guidelines. However, inadequate supply of HH items, insufficient time or emergencies, and increased workload were the major barriers to the practice of standard HH. Since these barriers are institution-based, we recommend that hospitals’ management employ more HCWs and ensure continued infectious disease training and an adequate supply of HH materials.
Availability of data and materials
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request. Data are located in controlled access data storage at the Department of Medical Rehabilitation, Nnamdi Azikiwe University, Nigeria.
Abbreviations
- ABHR:
-
Alcohol-based hand rubs
- ANOVA:
-
Analysis of Variance
- COVID-19:
-
Coronavirus Disease 2019
- HCW:
-
Health care workers
- HH:
-
Hand hygiene
- SARS-CoV-2:
-
Severe Acute Respiratory Syndrome Coronavirus 2
- SD:
-
Standard deviation
- WHO:
-
World Health Organization
References
Abbas M, RobaloNunes T, Martischang R, Zingg W, Iten A, Pittet D, et al. Nosocomial transmission and outbreaks of coronavirus disease 2019: the need to protect both patients and healthcare workers. Antimicrob Resist Infect Control. 2021;10(1):7.
Collins AS. Advances in patient safety preventing health care-associated infections. In: Hughes RG, editor. Patient safety and quality: an evidence-based handbook for nurses. Rockville: Agency for Healthcare Research and Quality (US); 2008.
Ezema CI, Onyeso OK, Okafor UA, Mabry LM, Adje ME, Shiraku J, et al. Knowledge, attitude and adherence to standard precautions among frontline clinical physiotherapists during the COVID-19 pandemic: a cross-sectional survey. Eur J Physiother. 2023;25(3):138–46.
Khan HA, Ahmad A, Mehboob R. Nosocomial infections and their control strategies. Asian Pac J Trop Biomed. 2015;5(7):509–14.
Lakoh S, Maruta A, Kallon C, Deen GF, Russell JBW, Fofanah BD, et al. How well are hand hygiene practices and promotion implemented in Sierra Leone? A cross-sectional study in 13 public hospitals. Int J Environ Res Public Health. 2022;19(7):3787.
Du Q, Zhang D, Hu W, Li X, Xia Q, Wen T, et al. Nosocomial infection of COVID-19: a new challenge for healthcare professionals (review). Int J Mol Med. 2021;47(4):31.
World Health Organization. Advice for the public: Coronavirus disease (COVID-19); 2023 https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public.
de Kraker MEA, Tartari E, Tomczyk S, Twyman A, Francioli LC, Cassini A, et al. Implementation of hand hygiene in health-care facilities: results from the WHO hand hygiene self-assessment framework global survey 2019. Lancet Infect Dis. 2022;22(6):835–44.
Onyedibe KI, Shehu NY, Pires D, Isa SE, Okolo MO, Gomerep SS, et al. Assessment of hand hygiene facilities and staff compliance in a large tertiary health care facility in northern Nigeria: a cross sectional study. Antimicrob Resist Infect Control. 2020;9(1):30.
Adejumo OA, Ogundele OA, Madubuko CR, Oluwafemi RO, Okoye OC, Okonkwo KC, et al. Perceptions of the COVID-19 vaccine and willingness to receive vaccination among health workers in Nigeria. Osong Public Health Res Perspect. 2021;12(4):236–43.
Ezema CI, Erondu OF, Onyeso OK, Alumona CJ, Ijever AW, Amarachukwu CN, et al. Radiographers’ knowledge, attitude and adherence to standard COVID-19 precautions and the policy implications: a national cross-sectional study in Nigeria. Ann Med. 2023;55(1):2210844.
Ilesanmi OS, Afolabi AA, Akande A, Raji T, Mohammed A. Infection prevention and control during COVID-19 pandemic: realities from health care workers in a north central state in Nigeria. Epidemiol Infect. 2021;149: e15.
Engdaw GT, Gebrehiwot M, Andualem Z. Hand hygiene compliance and associated factors among health care providers in Central Gondar zone public primary hospitals. Northwest Ethiopia Antimicrob Resist Infect Control. 2019;8:190.
Pires D, Soule H, Bellissimo-Rodrigues F, Gayet-Ageron A, Pittet D. Hand hygiene with alcohol-based hand rub: how long is long enough? Infect Control Hosp Epidemiol. 2017;38(5):547–52.
Pittet D. Improving adherence to hand hygiene practice: a multidisciplinary approach. Emerg Infect Dis. 2001;7(2):234–40.
Lotfinejad N, Peters A, Pittet D. Hand hygiene and the novel coronavirus pandemic: the role of healthcare workers. J Hosp Infect. 2020;105(4):776–7.
Tschudin-Sutter S, Sepulcri D, Dangel M, Schuhmacher H, Widmer AF. Compliance with the World Health Organization hand hygiene technique: a prospective observational study. Infect Control Hosp Epidemiol. 2015;36(4):482–3.
Sax H, Allegranzi B, Uçkay I, Larson E, Boyce J, Pittet D. ‘My five moments for hand hygiene’: a user-centred design approach to understand, train, monitor and report hand hygiene. J Hosp Infect. 2007;67(1):9–21.
Kampf G, Löffler H, Gastmeier P. Hand hygiene for the prevention of nosocomial infections. Dtsch Arztebl Int. 2009;106(40):649–55.
Hayden J. Introduction to health behavior theory. Jones & Bartlett Learning; 2022.
World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–4.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–9.
Amoo EO, Adekeye O, Olawole-Isaac A, Fasina F, Adekola PO, Samuel GW, et al. Nigeria and Italy divergences in coronavirus experience: impact of population density. Sci World J. 2020;2020:8923036.
Ojji DB, Sancilio A, Shedul GL, Orji IA, Chopra A, Abu J, et al. Nigeria healthcare worker sars-cov-2 serology study: results from a prospective, longitudinal cohort. PLoS Glob Public Health. 2023;3(1): e0000549.
Eze-Emiri C, Patrick F, Igwe E, Owhonda G. Retrospective study of COVID-19 outcomes among healthcare workers in Rivers State, Nigeria. BMJ Open. 2022;12(11): e061826.
Kang H. Sample size determination and power analysis using the g*power software. J Educ Eval Health Prof. 2021;18:17.
Heckathorn DD. Snowball versus respondent-driven sampling. Sociol Methodol. 2011;41(1):355–66.
World Health Organization. Hand hygiene knowledge questionnaire; 2009. https://cdn.who.int/media/docs/default-source/integrated-health-services-(ihs)/hand-hygiene/monitoring/surveyform/hand-hygiene-knowledge-questionnaire.doc?sfvrsn=dbb4da65_2
Ra’awji BAA, Almogbel ES, Alharbi LA, Alotaibi AK, Al-Qazlan FA, Saquib J. Knowledge, attitudes, and practices of health-care workers regarding hand hygiene guidelines in Al-Qassim, Saudi Arabia: a multicenter study. Int J Health Sci (Qassim). 2018;12(2):3–8.
Refeai SA, Kamal NN, Ghazawy ERA, Fekry CM. Perception and barriers regarding infection control measures among healthcare workers in Minia City. Egypt Int J Prev Med. 2020;11:11.
Onyeso OKK, Umunnah JO, Ibikunle PO, Odole AC, Anyachukwu CC, Ezema CI, et al. Physiotherapist’s musculoskeletal imaging profiling questionnaire: Development, validation and pilot testing. S Afr J Physiother. 2019;75(1):1338.
Sullivan GM, Artino AR Jr. Analyzing and interpreting data from likert-type scales. J Grad Med Educ. 2013;5(4):541–2.
Onyeso OK, Umunnah JO, Eze JC, Onigbinde AT, Anyachukwu CC, Ezema CI, et al. Musculoskeletal imaging authority, levels of training, attitude, competence, and utilisation among clinical physiotherapists in Nigeria: a cross-sectional survey. BMC Med Educ. 2022;22(1):701.
Tabachnick BG, Fidell LS. Using multivariate statistics. 6th ed. Boston: Pearson; 2013.
Abd Rahim MH, Ibrahim MI. Hand hygiene knowledge, perception, and self-reported performance among nurses in Kelantan, Malaysia: a cross-sectional study. BMC Nurs. 2022;21(1):38.
Ahmadipour M, Dehghan M, Ahmadinejad M, Jabarpour M, MangolianShahrbabaki P, Ebrahimi RZ. Barriers to hand hygiene compliance in intensive care units during the COVID-19 pandemic: a qualitative study. Front Public Health. 2022;10: 968231.
Roshan R, Feroz AS, Rafique Z, Virani N. Rigorous hand hygiene practices among health care workers reduce hospital-associated infections during the COVID-19 pandemic. J Prim Care Community Health. 2020;11:2150132720943331.
Cheong HS, Kwon KT, Hwang S, Kim SW, Chang HH, Park SY, et al. Workload of healthcare workers during the COVID-19 outbreak in Korea: a nationwide survey. J Korean Med Sci. 2022;37(6): e49.
Saud M, Mashud MI, Ida R. Usage of social media during the pandemic: Seeking support and awareness about COVID-19 through social media platforms. J Public Affairs. 2020;20(4): e2417.
Glasdam S, Sandberg H, Stjernswärd S, Jacobsen FF, Grønning AH, Hybholt L. Nurses’ use of social media during the COVID-19 pandemic—a scoping review. PLoS ONE. 2022;17(2): e0263502.
Neely S, Eldredge C, Sanders R. Health information seeking behaviors on social media during the COVID-19 pandemic among American social networking site users: survey study. J Med Internet Res. 2021;23(6): e29802.
Savadori L, Lauriola M. Risk perceptions and COVID-19 protective behaviors: a two-wave longitudinal study of epidemic and post-epidemic periods. Soc Sci Med. 2022;301: 114949.
Harun MGD, Anwar MMU, Sumon SA, Mohona TM, Hassan MZ, Rahman A, et al. Hand hygiene compliance and associated factors among healthcare workers in selected tertiary-care hospitals in Bangladesh. J Hosp Infect. 2023;139:220–7.
Nwaokenye J, Lakoh S, Morgan J. Perceptions of Nigerian healthcare workers towards hand hygiene: a qualitative study. Pan Afr Med J. 2020;36:204.
Desta M, Ayenew T, Sitotaw N, Tegegne N, Dires M, Getie M. Knowledge, practice and associated factors of infection prevention among healthcare workers in Debre Markos Referral Hospital, Northwest Ethiopia. BMC Health Serv Res. 2018;18(1):465.
DehghanManshadi SA, Sedaghat M, Mohammad Hashem F, Salehi M, Mohammadnejad E, Seifi A, et al. Knowledge and perception of hand hygiene: a survey using who standardized tools in Tehran. Iran Caspian J Intern Med. 2022;13(1):122–6.
Acknowledgements
We thank the study participants for their cooperation and the research assistants for their various roles that contributed to the success of this study.
Funding
There was no external funding for this study.
Author information
Authors and Affiliations
Contributions
ECE, IBN, CN, ENDE, and ACO contributed to the conception of this study. All authors made substantial contributions to the design. All authors participated in data acquisition. OKO, CJA, OEA, and KMO performed the statistical analysis. ECE, CN, IBN, CJA, OEA, and KMO were responsible for drafting the article. OKO, ENDE, IAA, EYI, and ACO contributed to its critical revision. All authors approved the final manuscript for publication and agreed to be accountable for all aspects of the work, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Health Research and Ethics Committee of the Faculty of Health Sciences and Technology, Nnamdi Azikiwe University, Awka, Anambra, Nigeria (MRH/NAU/FHST/2023/3). The study's objectives, procedures, and benefits were clearly explained to the participants. Each participant signed a written informed consent before participating in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ekediegwu, E.C., Onyeso, O.K., Nwanne, C. et al. COVID-19 hand hygiene practices and its barriers among health care workers in a low-resource setting: a cross-sectional study in Nigeria. Discov Soc Sci Health 4, 43 (2024). https://doi.org/10.1007/s44155-024-00106-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44155-024-00106-z