Abstract
Introduction
Globally, 269 million children aged 6–59 months were anemic in 2019. Of these, 103 million anemic children were from Africa. Childhood anemia is still a serious public health concern in SSA countries, including Ethiopia. In Ethiopia, the prevalence of childhood anemia largely varies by geographic administration regions. This study is aimed to examine trends in regional inequalities in childhood anemia in Ethiopia over the period 2005–2016.
Method
This cross-sectional study was based on a pooled total sample of 17,766 children aged 6–59 months drawn from three rounds of the Ethiopian Demography and Health Surveys (2005–2016). We employed multilevel binary logistic regression analysis to identify the determinants of childhood anemia among children aged 6–59 months. We also used Theil and multivariate decomposition analyses to examine the levels and trends in relative regional inequalities in childhood anemia.
Result
A combination of individual-, household- and community-level factors were significantly (p < 001) associated with childhood anemia. From the pooled data, the highest childhood anemia was observed in Somali (78.68%) followed by Afar region (72.76%) while the lowest childhood anemia was in Amhara (41.01%), Addis Ababa (42.64%) and SNNPR (44%) between 2005 and 2016. The total relative inequality declined from 0.620 in 2005 to 0.548 in 2016. Overall, one-third of change in regional inequalities in childhood anemia was due to the differential resulted from the difference in observable characteristics of the subjects.
Conclusion
Overall progress made in Ethiopia was very slow with only a 13.14% reduction in the relative regional inequalities in childhood anemia over 11 years. The present study underscores addressing the existing disparities in socioeconomic status, maternal anemia and maternal employment status between emerging and non-emerging regions to reduce regional inequality in childhood anemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Anemia refers to lower level of red blood cell or hemoglobin (Hb) than normal [1], which is one of the key child survival indicators [2]. Anemia affects under-five children disproportionately relative to the general population [3]. Childhood anemia among children aged 6–59 months is a condition where a child has an insufficient hemoglobin level (< 110 g/l) [1], and one of the most serious public health concerns in developing countries [4]. Childhood anemia leads to poor child growth, impaired cognitive capacity and learning ability [5], and causes child mortality and morbidity [6].
Globally, 269 million children aged 6–59 months were anemic in 2019, of which, 103 million of them were from Africa [7]. Sub-Saharan Africa (SSA) had the highest burden of childhood anemia [8], where more than 64% of under-five children were anemic in 2019 [9]. Childhood anemia is still a serious public health concern in SSA countries, including Ethiopia [10]. Even though Ethiopia has shown continued commitment in implementing nutrition related programs and policies since 2008 [9,10,11], childhood anemia remains one of the major public health problems in the country.
In Ethiopia, the prevalence of childhood anemia largely varies by geographic administration regions. For example, Somali region had the highest level of childhood anemia (83%), followed by Afar region (75%); whereas the Amhara region had the lowest anemia prevalence among children (42%) in 2016 [12]. Geographic location based inequalities in childhood anemia are documented in Ethiopia [13,14,15,16]. In addition to inequalities by geographic locations, childhood anemia is worsening at national level, where unacceptably higher proportion (57%) of children aged 6–59 months were anemic in 2016 compared to the prevalence of 54% in 2005 [12]. This situation demands evidence-based investigation on trends in inequalities in childhood anemia by administrative regions in the country. The findings will serve to monitor the existing programs and consider context specific interventions at regional levels. In addition, examining trends in regional disparities in childhood anemia helps regional governments and policy makers to review regional policies vis-a-vis child health concerns.
Although most previous studies [12,13,14,15] have focused on the trends in inequalities in childhood anemia, a few studies [19,20,21,22] examined regional inequalities in childhood anemia in developing countries. Most of them did not consider the hierarchal nature of data for assessing the factors associated with childhood anemia and did not use multilevel analysis approach to explore the effects of individual, household and community characteristics. In addition, none of them quantified the contributions of observed and unobserved heterogeneity at the individual, household and community level through decomposition techniques. To the best of our knowledge, there were no studies conducted in Ethiopia that examine the trends in regional inequalities in childhood anemia using both multilevel and decomposition techniques as well as Theil Index analysis. This study has thus primarily aimed at filling this knowledge gap, and seeks to answer the question “What is the extent of trends in regional inequalities in childhood anemia in Ethiopia between 2005 and 2016?”.
2 Data and methods
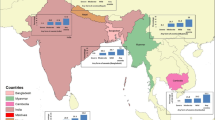
2.1 Study setting
Ethiopia is geographically and ethnically diversified country [17]. Ethiopia is landlocked and bounded by Eritrea to the north and northeast, Djibouti to the east, Somalia to the east and southeast, Kenya to the south, and Sudan and south Sudan to the west [18]. Ethiopia has implemented the Millennium Development Goals (MDGs) during the period 2000 to 2015 and registered remarkable achievements in improving child survival. Ethiopia’s government is strongly committed and implementing the 2030 Agenda for Sustainable Development and its Sustainable Development Goals (SDGs) as an integral part of its national development framework [19]. The SDG-integrated Growth Transformation Plan (GTP II) was subsequently implemented by all regional states and city administrations [19]. Although Ethiopia’s economy had shown increment from 2005 to 2016, there were significant differences in poverty reduction and non-monetary welfare outcomes across regional states [20]. Particularly, the pastoral and drought-prone regions (Somali and Afar) are lagging on all non-monetary indicators though regional inequality in consumption is low [21]. Inequality measured by the Gini coefficient, and inequality of opportunity for children largely varies across regional states [20].
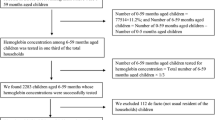
2.2 Data source
This study was based on the three rounds of the Ethiopian Demographic and Health Surveys (EDHSs) (2005–2016). These nationally representative surveys used cross-sectional study designs to monitor and explore maternal and child health indicators, including anemia. Stratified two-stage cluster sampling design was employed for selecting enumeration areas and households within each enumeration area for EDHSs [12]. The EDHSs collected information on geographic location, socioeconomic, demographic, health and nutrition related characteristics of individuals and households from women aged 15–49 years. Accordingly, a pooled sample of 17,766 children aged 6–59 months was included for analysis by merging data from the three rounds of EDHSs.
2.3 Study variables
2.3.1 Outcome variable
The outcome variable of the study was childhood anemia. It is a dummy variable, and assigned value of 1 if a child had severe, moderate or mild anemia level and 0 if a child is not anemic.
2.3.2 Explanatory variables
The explanatory variables of this study were grouped as exposure variable and covariates. The administrative region (community level) was the exposure variable identified as the key inequality driver of childhood anemia [15]. The eleven administrative regions of Ethiopia were included in this study, and further regrouped into three regional categories for analysis purpose as follows: emerging regions (Afar, Somali, Benishangul-Gumuz, and Gambella), established regions (Amhara, Oromia, Harari, Southern Nations Nationalities, and People’s Region (SNNPR) and Tigray) and fully urban (Addis Ababa and Dire Dawa City Administrations) [22]. Furthermore, we classified regional category into two categories (emerging and non-emerging (consisting of established and urban regions)) to generate a dummy variable for decomposition analysis.
Selection of the covariates was guided by the UNICEF’s conceptual framework for child malnutrition [23] and Mosley and Chen’s child survival framework [24]. We classified the covariates into community-, household- and individual-level variables. The community-level covariate, place of residence, was categorized as rural or urban. The household-level covariates included in this study were sex of household head (male/female); household size (< 6/6 +), number of under-five children in the household (< 2/2 +) and household wealth index. The household wealth index was classified into five quintiles (poorest, poorer, medium, richer and richest), and further regrouped into poor (poorest/poorer) and non-poor (medium, richer and richest).
The individual-level covariates included in this study were sex of child (male/female); child age in months (6–23/24–59 months); child size at birth as reported subjectively by mothers (small/average/large); birth order (1st/2nd–4th/5+); nutritional status of child (undernourished/nourished); duration of breastfeeding is indexed for each child (never breastfed/ 12 months/ 12 + months); maternal education (no formal education, primary, and secondary +); partner’s education (no formal education, primary, and secondary +); maternal employment status (yes/no); mother’s anemia level (anemic/not anemic); maternal age at child birth computed from mother’s and her child birth date (< 19/19 +); place of delivery (home/health facility); and survey period (2005–2011 or 2012–2016).
2.4 Statistical methods
All statistical analyses were performed using STATA version 17.0 (College Station, Texas 77845 USA). Children with missing weight, height/length and other unknown responses were excluded from statistical analysis. Descriptive statistics were used to describe the background characteristics of the study participants. Variance Inflation Factor (VIF) with cutoff value of 2.5 [25] was used to test multicollinearity effect of the explanatory variables, and result is annexed (Annex 1). Bivariate analysis was employed to explore the strength of the association between an explanatory variable and childhood anemia to make the decision for inclusion of candidate explanatory variables (p < 0.2) into multilevel logistic regression analysis.
Multilevel binary logistic regression analysis was employed for mixed effect model [26] to explore the net effect of each explanatory variable on childhood anemia. Multilevel modeling recognizes the inherent hierarchical structure of the EDHS data, where individuals are nested within household, and households are nested within community (Enumeration Areas/EA). For hierarchical data, use of a multilevel modeling is demanding as conventional regression analysis provides biased estimates [27]. We fitted a three-level model with the individual, household and community factors as level 1, level 2 and level 3, respectively. The null model was used as a baseline model to determine whether the use of multilevel modeling is appropriate for the analysis or not. Community-level predictors (administrative regions and place of residence) were included in Model I by controlling household and individual level variables. Model II was fitted after including household-level predictors into the Model I. The final model (Model III) was fitted with community, household and individual level explanatory variables to assess the association between the socioeconomic variables and childhood anemia. Intraclass Correlation Coefficient (ICC), Median Odds Ratio (MOR), Likelihood Ratio (LR) test and Criteria Information tests (AIC and BIC) were used for selecting the best model fitted for the multilevel analysis [28].
Theil Index was used to measure the inequalities in childhood anemia by administrative regions [29]. Theil index decomposes into two components (within group and between group) [30] to explore relative regional inequalities of within regions and between regions. The survey period was included to assess trends of regional relative inequalities in childhood anemia [31]. Furthermore, multivariate decomposition analysis was used to quantify the contributions to group (regional category) inequalities [32]. All analyses were made using weighted data.
3 Results
3.1 Background characteristics of the study participants
Table 1 describes the background characteristics of the study participants. More than half (54.54%) of children were living in the established regions, while about 37% of children and more than 8% of children were from emerging regions and two-chartered city administration (urban regional category), respectively. The majority (84.95%) of children were living in rural areas. Slightly higher proportion of children were living in the poor households (50.38%) compared to non-poor households (49.62%). The majority (83.25%) of children were from male headed households as compared to those living in female headed households (16.75%). More than half (57.10%) of children were living in the household with more than six household members. About 66% of the interviewed households had more than two under-five children during the survey period. There were slightly higher proportions (50.97%) of female children than male children (49.03%). More than 67% of children were 24–59 months of age during the survey period. Majority (81.53%) of children were born at home compared to those born at health facility (18.47%). Relatively lower proportions (17.92%) of children were born at the first birth order. Relatively higher proportions (52.51%) of children were undernourished. More than half (57.31%) of children were breastfed for more than a year while nonnegligible proportion (2.66%) of children never experienced breastfeeding. About 9% of children were born from young mothers (less than 19 years old). Significantly larger proportions (69.65%) of children were born from mothers who did not have any formal education, relative to the smaller proportion (30.35%) of children born from mothers who had at least primary level education. Nearly 53% children were born from mothers whose partners had no formal education. Most (70.86%) of the children were born from anemic mothers. More than half (57.69%) of children were born from unemployed mothers. About 61% of the study participants were surveyed during 2005–2011 survey period (Table 1).
3.2 Bivariate analysis results
Table 2 presents results of the bivariate association between the hypothesized explanatory variables and childhood anemia. Relatively higher proportion (60.47%) of children were significantly (p < 0.001) anemic in the later survey period (2012–2016) compared to the earlier survey period (2005–2011). It is seen that childhood anemia was significantly associated (p < 0.001) with regional category, and place of residence at community level. At household level, household wealth index, sex of household head, the household size and number of under-five children in the household were significantly (p < 0.001) associated with childhood anemia. At individual level, maternal education, anemia and employment status, partner’s education; place of birth, child’s nutritional status, age of child in months, and child size at birth as reported subjectively by mothers were significantly (p < 0.001) associated with childhood anemia. However, child sex, and maternal age at child birth were not statistically (p < 0.2) associated with childhood anemia. The overall prevalence of childhood anemia was 54.77% at national level between 2005 and 2016 (Table 2).
3.3 Results of multilevel analysis
Table 3 presents the multilevel logistic regression analysis results for the determinants of childhood anemia. The null model showed statistical significance, indicating that use of multilevel modeling was appropriate for the analysis. In Model I, children from the emerging regions had statistically (p < 0.001) higher likelihood of being anemic than their counterparts in the established regions. Children residing in urban areas were significantly (p < 0.001) less likely to be anemic compared to children living in rural areas.
In Model II, children born in emerging regions, and rural areas had significantly (p < 0.001) higher likelihood of being anemic than those children in the established regions and urban areas. Children living in the households (with at least one other under-five child) had a significantly (p < 0.001) higher likelihood of being anemic compared to those from the households (no other child). Children from non-poor households had significantly lower (p < 0.001) likelihood of anemia than their counterparts living in the poor households.
In Model III, children from the emerging regions, rural areas and poor households had significantly (p < 0.001) higher likelihood of being anemic than their counterparts in the established regions, urban areas and non-poor households, respectively. Under-two children (6–23 months of age) were more likely to be anemic than those children aged 24–59 months. Children born at fifth and above order had a significantly (p < 0.05) higher likelihood of being anemic compared to those born at first order. Undernourished (i.e., stunted, wasted or underweight) children had significantly (p < 0.001) higher likelihood of being anemic compared to nourished children. Children born from anemic mothers had significantly (p < 0.001) higher chance of being anemic. Similarly, children born from unemployed mothers had significantly (p < 0.001) higher likelihood of being anemic than those born from employed mothers. Childhood anemia was significantly (p < 0.001) higher in 2005–2011 as compared to the 2012–2016. However, household size, sex of household head, place of birth, child size at birth, and maternal and partner’s education were not significantly (p < 0.05) associated with childhood anemia in multilevel logistic analysis.
As seen from Table 3 above below, it was observed that the inclusion of individual level (level 1) covariates into the model decreased the effects of community variation from 0.301 (null model) to 0.001 (Model III). This indicates the presence of substantial variation between regions and rural–urban areas. Similarly, the household variation was also decreased from 0.563 (in Model 0) to 0.029 (Model III), which suggests that there is relative variation between communities (regions and urban rural areas) and households in childhood anemia.
Moreover, the estimated community level MOR, i.e., the unexplained regional inequality in childhood anemia also decreased from 1.687 (Model 0) to 1.001 (final model) while household level MOR also changed from 2.046 to 1.176. This suggests existence of variation between communities and households in childhood anemia. The values of AIC and BIC also decreased from 24,018.18 and 24,041.54 (Model 0) to 22,219.29 and 22,406.03 (in Model III), respectively. The lower values of AIC and BIC are evidences of better model fit of final model (Model III) compared to the rest of the models. Furthermore, likelihood ratio test (LR test) showed statistically significant associations for the fitted multilevel models and indicated good selection the models fitted for multilevel analysis.
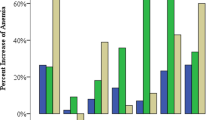
3.4 Theil decomposition trend analysis results
Table 4 shows Theil decomposition trend analysis results. In all, there were increments in prevalence of childhood anemia between 2005 and 2016 in Afar, Oromia, SNNPR, Harari, Addis Ababa and Dire Dawa. There was a substantial decrease in childhood anemia between 2005 and 2016 in Tigray, Amhara, Somali, Benishangul and Gambela. Total relative regional inequality in childhood anemia was highest (0.806) in 2011. The total relative inequality showed reduction from 0.620 in 2005 to 0.548 in 2016. The overall relative inequalities in childhood anemia could be explained by within region inequalities, and within region inequalities of childhood anemia was highest in 2011 (0.806) as compared to the year 2005 and 2016. About 98.87%, 97.39%, and 96.90% of the total relative inequalities in childhood anemia could be explained by within region inequalities, in 2005, 2011 and 2016, respectively. In view of the pooled data, the highest childhood anemia was observed in Somali (78.68%) followed by Afar region (72.76%) while the lowest childhood anemia was in Amhara (41.01%), Addis Ababa (42.64%) and SNNPR (44%) (Table 4).
3.5 Multivariate decomposition analysis results
Table 5 illustrates the overall and detailed multivariable decomposition analysis of regional inequalities in childhood anemia between 2005 and 2016. The multivariate decomposition analysis result revealed that 47.12% of observed regional inequalities in childhood anemia can be attributed to difference in characteristic effects (explained) while 52.88% could be due to difference in coefficient effect (unexplained component). Addressing the household socioeconomic status, maternal anemia and maternal employment status gaps would be expected to reduce the emerging and non-emerging regional inequalities in childhood anemia by about 12.91%, 13.83% and 14.15%, respectively. However, the disparity in household socioeconomic status, and maternal employment status could significantly (p < 0.01) contribute to widening the regional inequalities in childhood anemia by about 25.34%, and 23.64%, respectively (Table 5).
4 Discussion
The present study employed multilevel, Theil index and multivariate decomposition analyses to examine trends in regional inequalities in childhood anemia in Ethiopia using three round nationally representative data (2005–2016). The weighted prevalence of childhood anemia computed from three rounds pooled data analysis was 54.77%, higher than the prevalence of childhood anemia in Sudan (50.8%) [33], and in Uganda (50%) [34] and lower than in Nigeria (68.1%) [35], which needs attention to address contributing factors in the country.
Our multilevel analysis shows that the community, household and individual level factors had significant contribution to the observed childhood anemia prevalence in the country. This finding is consistent with previous studies conducted in Ethiopia [15] and Sub-Saharan Africa countries [36]. Children living in the emerging regions and rural areas had significantly higher likelihood of childhood anemic compared to children from established regions and urban settings at community level, which is consistent with a previous study conducted in Ethiopia [37]. This could be due to differences in socioeconomic status, access to resources, level of education, cultural and feeding practices [15]. In addition, individuals living in urban areas might have access to better education, awareness on child health and risk of anemia, better income and resource as compared to rural areas that are directly or indirectly related to poverty [15].
At household level, household asset-based wealth index was significantly associated with childhood anemia. Children from the poor households were more likely to be anemic than those living in the non-poor households. This could be directly linked with nutritional intake as anemia is a nutrient-deficiency health problem, and the richer households have the economic means to meet their children’s nutritional and health needs [36]. In line with this finding, undernourished (stunted, wasted or underweight) children were more likely to be anemic compared to nourished children. This could be due to the fact that anemia is one of nutritional diseases which is associated with poor dietary habits [36]. Children born from employed mothers were less likely to be anemic as compared to those born from unemployed mothers. This might be due to the reason that employed mothers can have relatively better chance to buy additional dietary foods for their children as compared to unemployed mothers. In our finding, children born from anemic mothers were more likely to be anemic as compared to those born from non-anemic mothers. This might be due to the reason that maternal iron deficiency could have potential effects on childhood anemia [38].
Our finding from the Theil index analysis result revealed that about 13.14% reduction of the relative regional inequality in childhood anemia from 0.620 in 2005 to 0.548 in 2016. This could be due to continued implementation of national and international commitments, including Millennium Development Goals (MDGs), Health Extension Program (HEP), Child survival strategies and Nutrition Programs as well as Secota declaration and Growth Transformation Plans in all regions. In this study, the overall relative inequalities in childhood anemia were largely explained by within region inequalities. The Theil index analysis using pooled data showed that the highest childhood anemia in Somali (78.68%) followed by Afar region (72.76%), while the lowest childhood anemia was in Amhara (41.01%) from the pooled. This indicates that the existence of the highest burden of childhood anemia in emerging regions as compared to non-emerging regions (i.e., established regions and urban regions). The potential reason could be the fact that Somali and Afar regions are mostly drought and malaria-prone regions [21] and the drought and malaria could directly or indirectly escalate prevalence of childhood anemia in these regions.
Our multivariate decomposition analysis also revealed that more than a half (52.88%) of the regional inequalities in childhood anemia was due to difference in unobserved characteristics (coefficient effect), and the remaining (47.12%) was due to difference in observed characteristic effects. Household socioeconomic status (wealth index), maternal anemia and maternal employment have significantly explained the variations in the regional inequalities in childhood anemia between emerging and non-emerging regions over the study period. Therefore, equalizing the socioeconomic status, maternal employment status and maternal anemia could contribute to reduce the emerging and non-emerging regional inequalities in childhood anemia by about 12.91%, 13.83% and 14.15%, respectively. This suggests due attention for addressing the existing disparities in socioeconomic status, maternal anemia and maternal employment status between emerging and non-emerging regions to reduce regional inequality in childhood anemia.
Finally, it is worth mentioning the strengths and limitation of the present study. Concerning the strength of the study, our findings were based on a nationally representative sample of respondents from all old regions that could be generalized to the broader population in Ethiopia. Thus, the findings could be helpful in addressing regional differences in the prevalence of anemia among children. However, we also recognized that this study has some limitations. First, this study is based on repeated cross-section surveys, which was not possible to draw cause-effect relationship. Second, all the DHS data are self-reported, and hence, might be influenced by recall bias. In addition, most mothers are illiterate that could lead to non-response, omission and commission errors. Third, the present study focused on well documented determinants of childhood anemia, there might be potential factors not included in the analysis, including food insecurity, appropriate child feeding, and others. Lastly, macro level factors affecting anemia (such as policy, finance, government commitment, and others) are not part of this analysis.
5 Conclusion
With only a 13.14% reduction in the relative regional inequalities in childhood anemia over 11 years, progress made in Ethiopia was very slow. Overall, one-third of change in regional inequalities in childhood anemia was due to the differential resulted from the difference in observable characteristics of the subjects. Household asset-based wealth index, maternal anemia and maternal employment status are significantly contributed to reduce and increase in regional inequalities in childhood anemia over the study period. Therefore, the present study underscores addressing the existing disparities in socioeconomic status, maternal anemia and maternal employment status between emerging and non-emerging regions to reduce regional inequality in childhood anemia.
Data availability
The dataset can be accessed at https://dhsprogram.com/data/available-datasets.cfm.
Abbreviations
- AIC:
-
Akaike’s Information Criteria
- BIC:
-
Bayesian Information Criteria
- CSA:
-
Central Statistical Agency
- DHS:
-
Demographic and Health Survey
- EDHS:
-
Ethiopia Demographic and Health Survey
- ICC:
-
Intraclass Correlation Coefficient
- LR:
-
Likelihood ratio
- SDG:
-
Sustainable Development Goal
- UNICEF:
-
United Nations Children’s Fund
- VIF:
-
Variance Inflation Factor
- WHO:
-
World Health Organization
References
WHO. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Geneva, Switz. World Heal. Organ, pp. 1–6, 2011, 2011.
Nkosi-Gondwe T, Calis J, van Hensbroek MB, Bates I, Blomberg B, Phiri KS. A cohort analysis of survival and outcomes in severely anaemic children with moderate to severe acute malnutrition in Malawi. PLoS ONE. 2021;16(2):1–11. https://doi.org/10.1371/journal.pone.0246267.
Sunguya BF, et al. Regional disparities in the decline of anemia and remaining challenges among children in Tanzania: analyses of the Tanzania demographic and health survey 2004–2015. Int J Environ Res Public Health. 2020;17(10):1–15. https://doi.org/10.3390/ijerph17103492.
Tesfaye TS, Tessema F, Jarso H. Prevalence of anemia and associated factors among ‘apparently healthy’ urban and rural residents in Ethiopia: a comparative cross-sectional study. J Blood Med. 2020;11:89–96. https://doi.org/10.2147/JBM.S239988.
Zegeye B, Ahinkorah BO, Ameyaw EK, Seidu AA, Keetile M, Yaya S. Determining prevalence of anemia and its associated factors in Cameroon: a multilevel analysis. Biomed Res Int. 2021. https://doi.org/10.1155/2021/9912549.
WHO. The global prevalence of anaemia in 2011. Who, pp. 1–48, 2011, [Online]. Available: https://apps.who.int/iris/handle/10665/177094.
Stevens GA, et al. National, regional, and global estimates of anaemia by severity in women and children for 2000–19: a pooled analysis of population-representative data. Lancet Glob Heal. 2022;10(5):e627–39. https://doi.org/10.1016/s2214-109x(22)00084-5.
Safiri S, et al. Burden of anemia and its underlying causes in 204 countries and territories, 1990–2019: results from the Global Burden of Disease Study 2019. J Hematol Oncol. 2021;14(1):1–16. https://doi.org/10.1186/s13045-021-01202-2.
Federal Democratic Republic of Ethiopia. Republic of Ethiopia National Nutrition Program 2008–2015. 2008.
Federal Democratic Republic of Ethiopia. Food and Nutrition policy Ethiopia. 2018.
Federal Ministry of Health. National-Nutrition-Strategy 2008.pdf. 2008.
Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016. 2016.
Anteneh ZA, Van Geertruyden JP. Spatial variations and determinants of anemia among under-five children in Ethiopia, EDHS 2005–2016. PLoS ONE. 2021;16(4):1–24. https://doi.org/10.1371/journal.pone.0249412.
Endris BS, Dinant GJ, Gebreyesus SH, Spigt M. Geospatial inequality of anaemia among children in Ethiopia. Geospat Health. 2021. https://doi.org/10.4081/gh.2021.1036.
Gebreegziabher T, Regassa N, Wakefield M, Pritchett K, Hawk S. Disparities in the prevalence and risk factors of anaemia among children aged 6 24 months and 25 59 months in Ethiopia. J Nutr Sci. 2020. https://doi.org/10.1017/jns.2020.29.
Jember TA, Teshome DF, Gezie LD, Agegnehu CD. Spatial variation and determinants of childhood anemia among children aged 6 to 59 months in Ethiopia: further analysis of Ethiopian demographic and health survey 2016. BMC Pediatr. 2021;21(1):1–14. https://doi.org/10.1186/s12887-021-02901-y.
Tariku S, Gara L. Place of diversity in the current Ethiopian education and training policy: analysis of Cardinal dimensions. Educ Res Rev. 2016;11(8):582–8. https://doi.org/10.5897/err2015.2614.
FAO. AQUASTAT Country Profile—Ethiopia. Food and Agriculture Organization of the United Nations (FAO). Rome, Italy. FAO, AQUSAT reports, pp. 11–12, 2016.
National Plan Commission. Voluntary National Reviews on SDGs of Ethiopia: Government Commitments, National Ownership and Performance Trends. pp. 1–52, 2017.
World Bank. Ethiopia Regional Poverty Report. Ethiop Reg Poverty Rep. 2020. https://doi.org/10.1596/34805.
World Bank. Poverity and Equity Brief: Ethiopia. 2022, [Online]. Available: https://databankfiles.worldbank.org/data/download/poverty/987B9C90-CB9F-4D93-AE8C-750588BF00QA/current/Global_POVEQ_ETH.pdf.
Bareke L, Agezew BH, Dedho NH, Hailu A. Education inequalities in Ethiopia: a macro-level analysis and its policy implications. 2022. https://doi.org/10.20944/preprints202206.0341.v1.
UNICEF, Improving Child Nutrition—The achievable imperative for global progress. United Nations Children’s fund. 2013.
Mosley WH, Chen LC. An analytical framework for the study of child survival in developing countries. Bull World Health Organ. 1984;81(2):140–5. https://doi.org/10.1590/S0042-96862003000200012.
Johnston R, Jones K, Manley D. Confounding and collinearity in regression analysis: a cautionary tale and an alternative procedure, illustrated by studies of British voting behaviour. Qual Quant. 2018;52(4):1957–76. https://doi.org/10.1007/s11135-017-0584-6.
StataCorp., Multilevel Mixed Effects REFERENCE MANUAL RELEASE 17. A Stata Press Publication StataCorp LLC College Station, Texas, 2021.
Snijders and Bosker. Multilevel analysis: an introduction to basic and advanced multilevel modeling, second edition. Sage Publishers, 2012. Available: https://www.stats.ox.ac.uk/~snijders/MLB_new_S.pdf.
Luke D. Multilevel modeling: the null model. Second edition. SAGE Publications Inc.; 2020.
Hosseinpoor AR, Bergen N, Barros AJD, Wong KLM, Boerma T, Victora CG. Monitoring subnational regional inequalities in health: measurement approaches and challenges. Int J Equity Health. 2016. https://doi.org/10.1186/s12939-016-0307-y.
Wijaya O, Susanto DA, Heruwarsi T, Giyanti S, Ibrahim NRN. Decomposition of the Theil index in inequality analyses in Yogyakarta Indonesia. E3S Web Conf. 2021;316:02046. https://doi.org/10.1051/e3sconf/202131602046.
Li J. Rate decomposition for aggregate data using Das Gupta’s method. Stata J. 2017;17(2):490–502. https://doi.org/10.1177/1536867x1701700213.
Powers DA, Yoshioka H, Yun MS. Mvdcmp: multivariate decomposition for nonlinear response models. Stata J. 2011;11(4):556–76. https://doi.org/10.1177/1536867X1201100404.
Elmardi KA, Adam I, Malik EM, Ibrahim AA, Elhassan AH, Kafy HT, Nawai LM, Abdin MS, Kremers S. Anaemia prevalence and determinants in under 5 years children findings of a cross-sectional population-based study in Sudan. BMC Pediatr. 2020;2020(538):20. https://doi.org/10.1186/s12887-020-02434-w.
Nankinga O, Aguta D, Kabahuma C. Trends and determinants of anemia in Uganda: further analysis of the demographic and health surveys. DHS Working Paper No. 149. Rockville, Maryland, USA: ICF. 2019, https://doi.org/10.2147/phmt.s258114.
Obasohan PE, Walters SJ, Jacques R, Khatab K. Individual, household and area predictors of anaemia among children aged 6–59 months in Nigeria. Public Heal Pract. 2022;3(2021):100229. https://doi.org/10.1016/j.puhip.2022.100229.
Amegbor PM, Borges SS, Pysklywec A, Sabel CE. Effect of individual, household and regional socioeconomic factors and PM2.5 on anaemia: a cross-sectional study of sub-Saharan African countries. Spat Spatiotemporal Epidemiol. 2022;40(2021):100472. https://doi.org/10.1016/j.sste.2021.100472.
Heinrichs H, Endris BS, Dejene T, Dinant GJ, Spigt M. Anaemia and its determinants among young children aged 6–23 months in Ethiopia (2005–2016). Matern Child Nutr. 2021;17(2):1–13. https://doi.org/10.1111/mcn.13082.
Shukla AK, Srivastava S, Verma G. Effect of maternal anemia on the status of iron stores in infants: a cohort study. J Fam Community Med. 2019;26(2):118–22. https://doi.org/10.4103/jfcm.JFCM_115_18.
Acknowledgements
We are grateful to the MEASURE DHS program for providing free access to the original data.
Authors’ information
Center of Population Studies, College of Development Studies, Addis Ababa University, Addis Ababa, Ethiopia (NST, NRG).
Funding
The study did not receive any funding.
Author information
Authors and Affiliations
Contributions
Conception and design of the study: NST and NRG; analysis and/or interpretation of data; drafting the manuscript: NST; revising the manuscript critically for important intellectual content: NRG. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
For the original conduct of the five rounds of Ethiopia Demographic and Health Surveys (DHSs), ethical approval was obtained from the ethical committee of the ICF. The enumerators obtained informed consent and authorization to anonymously use the data from all survey participants. In our study, we obtained permission to use the data from the DHS program. No further ethical approval was required, as our study solely involved secondary data analysis of publicly available data that does not contain any identifiable information that links to the actual survey participants. The authors also confirm that all methods were carried out by relevant guidelines and regulations.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Annex 1: variance inflation factor
Annex 1: variance inflation factor
Explanatory variables | VIF | 1/VIF |
|---|---|---|
Birth order | 1.776 | 0.563 |
Place of residence | 1.687 | 0.593 |
Place of birth | 1.604 | 0.623 |
Household size | 1.524 | 0.656 |
Child age in months | 1.504 | 0.665 |
Duration of breastfeeding | 1.493 | 0.67 |
Maternal education | 1.408 | 0.71 |
Household wealth index | 1.291 | 0.774 |
Partner’s education | 1.289 | 0.776 |
Region | 1.247 | 0.802 |
Maternal age at child birth | 1.224 | 0.817 |
Number of under-five in the HH | 1.144 | 0.874 |
Survey period | 1.109 | 0.902 |
Nutritional status of child | 1.070 | 0.935 |
Maternal anemia | 1.063 | 0.94 |
Maternal employment | 1.062 | 0.942 |
Sex of household head | 1.041 | 0.96 |
Child size at birth | 1.040 | 0.961 |
Child sex | 1.011 | 0.989 |
Mean VIF | 1.294 |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Negussie, ., Nigatu, . Trends in regional inequalities in childhood anemia in Ethiopia: evidence from the 2005–2016 Ethiopian Demographic and Health Surveys. Discov Soc Sci Health 3, 7 (2023). https://doi.org/10.1007/s44155-023-00038-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44155-023-00038-0