Abstract
Background
Addressing population health inequities begins with quantifying how social factors affect the health and health care utilization of individuals. Such quantification relies on the availability of detailed health and demographic data. Unfortunately, administrative health care data rarely includes detailed demographic information. Data linkage, which combines administrative health data with national-level census or survey data, enables researchers to examine socio-economic inequalities in health care utilization in greater detail.
Data and methods
With access to a unique Canadian dataset linking data from the Hospital Discharge Abstract Database (DAD) from 2006 to 2007 with detailed individual-level socio-demographic data from the 2006 Canadian Census, we are able to examine the patterning of hospitalization in Canada in the early 2000s across a variety of socio-demographic variables. We examine the association of education and income, controlling for immigration status, rural residence, marital status and ethnicity, with hospitalization rates for both ambulatory care sensitive conditions (ACSCs) and non-ambulatory care sensitive conditions (non-ACSCs) for children and youth, working-age adults, and older adults, in models stratified by sex.
Results
Age standardized hospitalization rates show that there is a clear socio-economic gradient in hospitalization in Canada in the 2000s. Education and income are independently, inversely associated with hospitalization for males and females across three broad age groups. These associations are stronger for ACSCs than non-ACSCs. The association of other socio-demographic variables, such as immigrant status, and rural residence is also stronger for hospitalization for ACSCs. The association of socio-economic status with hospitalization for ACSCs is strongest for working age women and men, and is somewhat attenuated for older adults.
Conclusions
Lower socio-economic status is associated with a higher likelihood of hospitalization for men and women in Canada across three broad age groups in the 2000s. These associations are stronger for ACSCs, suggesting that in addition to increased likelihood of disease, decreased access to preventative care may be driving up hospitalization rates for marginalized groups. We conclude with the recommendation that in order to track progress in reducing health inequities, health systems should either collect detailed individual-level socio-demographic data or link their administrative health data to existing demographic data sets.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Background
Despite the existence of a universal national health care system, survey research shows that there remains an inverse relationship between socio-economic position and self-reported health status in Canada [1,2,3], similar to that seen in many other countries [4, 5]. Canadians who are identified as having lower socio-economic position (operationalized using various indicators, including education, income, and occupation) have poorer outcomes across multiple health measures [6, 7]. The inverse relationship between social class and health, which has also been documented in other countries with universal health care systems [8,9,10] indicates that as well as social disparities in health behaviours and health outcomes, there is also evidence of social disparities in health care utilization [3, 11, 12].
Structural inequalities within the Canadian health care system and others have long been masked by a lack of available data [13, 14]. The data that are collected on individuals in hospital charts and health records rarely include any socio-demographic measures beyond age and sex. Previous studies using administrative data to examine inequities in health care utilization have relied almost exclusively on aggregated area-level measures of socio-economic status (average neighbourhood income derived from Census data and matched to individuals through postal code, for example) [8, 9, 15]. These studies usually depend on ecological correlations to draw conclusions about socio-economic status and health and health care outcomes. Yet individual- and area-based measures are often not in agreement, and may represent different pathways to health inequities [3, 16, 17].
In this paper, we take advantage of a unique dataset that links hospitalization records with detailed individual-level socio-demographic data from the long-form Canadian Census [18] to examine the characteristics of those who are hospitalized and shine a light on the persistence of socio-demographic inequalities in hospitalization rates in Canada. These data enable us to examine multiple individual-level measures of socio-economic status across all age groups for the entire Canadian population [19]. We are also able to use the detailed diagnostic data to examine hospitalizations for ambulatory care sensitive conditions (ACSCs) separately from hospitalizations for non-ambulatory care sensitive conditions (non-ACSCs), which allows us to speculate about the various mechanisms through which the different socio-demographic variables may be affecting health and health care utilization.
2 Previous research
Previous research has demonstrated that lower socio-economic status (SES) is associated with higher morbidity [20,21,22], higher mortality [1, 23], and increased health care utilization [24, 25] in Canada and elsewhere. This research typically relies on one of two types of data. Some researchers use survey data such as the Canadian Community Health Survey (CCHS) in Canada [26] and the National Health Interview Survey (NHIS) in the United States (US) [27] to examine the relationship between SES and health. By necessity, this survey data contains self-reported measures of both socio-economic variables and health and disease status. For example, chronic diseases are measured in the CCHS with the question “Have you ever been diagnosed with…..?” Although the demographic data tends to be very detailed in these surveys, the health data is not detailed, and is considered less robust than the data in administrative health records [28]. The validity of self-reported health data can be affected by poor participant recall, social desirability bias, and current societal awareness of certain health conditions [28].
Other researchers rely on health care administrative data, such as primary care records, provincial health care records, or hospital discharge data to examine the relationship between SES and health. While these data usually contain detailed and precise health information, there is often not much demographic data collected (for example, in Canadian hospital discharge data the only demographic variables available are age and sex). Therefore these researchers will often match the patients’ postal code to Census Dissemination Areas and assign proxy aggregate Census measures of socio-economic status such as ‘average income in the Dissemination Area’ to individual patients [29,30,31]. These studies rely on the assumption that one can assign aggregate values to individuals, and fail to account for diversity within geographic areas, often leading to imprecise estimates of the effects of socioeconomic factors [32,33,34].
Recent advances in data management and expanded data availability have enabled researchers in several countries to access linked datasets which contain health information from health care administrative records linked to individual socio-demographic data from Censuses or surveys [35, 36]. These datasets allow researchers to examine the relationship between socio-demographic factors and health care utilization at the individual level. Recognizing the need to link demographic and health data in Canada, Statistics Canada has recently begun to provide access to some linked administrative health data and other data sources, including Censuses and surveys, to enable researchers to examine the relationships between measured, objective health outcomes and detailed individual-level social and demographic variables [3, 37, 38].
In 2015, a Statistics Canada project linked data from the 2006 long-form Census to 3 years of records from the Discharge Abstract Database (DAD) (April 1, 2006–March 31, 2009) [18]. This data, which is described in more detail in the methods section, has been used by other authors to focus on the demographic correlates of specific diseases, such as sepsis and diabetes [37, 38]. Results from these studies show that hospitalization rates for both sepsis and diabetes are influenced by several individual-level socio-demographic variables, including race/ethnicity, household income and labour force participation. Other researchers have used these data to examine variations in hospitalization rates for Indigenous people in Canada. Carriere et al. show that while hospitalization rates for ACSCs are higher for Indigenous groups than non-Indigenous groups, these rates vary by Indigenous status (First Nation, Metis or Inuit, on-reserve and off-reserve) [39].
Another recent Statistics Canada project links data from the Canadian Community Health Survey (across many years) to the Discharge Abstract Database [40]. Researchers have used this data to examine the effects of survey-reported socio-economic status and health behaviours on various health outcomes such as cancer [41] and hospitalization [3]. Focusing exclusively on hospitalization for chronic conditions such as asthma, COPD, diabetes and hypertension, researchers found that both individual income and neighbourhood deprivation (measured using aggregate census data) affect hospitalizations. The authors of all of the papers using the linked datasets conclude that more work is necessary to understand the mechanisms through which socioeconomic status influences health in Canada.
3 Our approach
We approach this work through the lens of the social determinants of health [42, 43], emphasizing that social and environmental factors play a ‘fundamental’ role in health [44]. Socioeconomic stratification leads to the inequitable distribution of opportunities, resources and constraints, which then operate through an intersection of material, behavioural, and psychosocial mechanisms to affect health [45, 46]. Although they are not the focus of our current study, we recognize that sex [47, 48], race/ethnicity [12, 14, 39], immigration status [25], marital status (for adults) [49, 50], and area of residence [51] are all important social determinants of health. We control for these factors in all of our models. We focus our current analysis on two indicators of socioeconomic position that are available in the Census data, education and income [52, 53]. We posit that education and income may have independent associations with hospitalization, as they may represent access to different types of opportunities, resources, and constraints.
Group differences in hospitalization rates may reflect several types of health disparities including: different exposure to and rates of disease; differential access to information about health; differential access to resources that promote health (such as healthy food, opportunities for physical activity) or prevent disease (such as medication); and differential access to specific kinds of health care (such a primary care and specialist care) [3].
One method of disentangling these effects is to examine hospitalization for ambulatory care sensitive conditions (ACSCs) separately from hospitalizations for non-ambulatory care sensitive conditions. ACSCs were first identified by Billings et al. in a study examining socioeconomic differences in hospitalization rates in 1988 in New York City [54]. Higher hospitalization rates were noted for certain conditions (termed ACSC) in low income areas compared to high income areas, which was hypothesized to be due to lack of timely outpatient care in low income areas. These differences in hospitalization rates for ACSCs between high versus low income areas were also demonstrated in Canada, though absolute differences are small, likely owing to universal health coverage and reduced barriers to outpatient care [55]. Hospitalizations for ACSCs are sometimes referred to as ‘avoidable’ hospitalizations, as they may reflect on access to primary care [56]. For example, rural/urban patterning of ACSC hospitalization rates in Canada exists [57], and is likely at least partially attributable to underservicing and reduce access to primary care in rural areas [58]. Hospitalization rates for ACSCs are therefore sometimes considered indicators of health system equity and performance [59].
Definitions of what should be classified as ambulatory care sensitive conditions vary [58]. The Canadian Institutes of Health Information (CIHI) includes the following conditions: angina; asthma, congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD), diabetes, epilepsy and hypertension [56]. The Agency for Healthcare Research and Quality (a branch of the Department of Health and Human Services in the United States) has a slightly different list which includes diabetes, COPD, hypertension, CHF, asthma and pneumonia [59]. Researchers have argued that these lists should be expanded to include several other conditions including other vaccine preventable diseases [60, 61].
A study by Pinto et al. compared four lists of ACSCs, and found that the CIHI list had a higher disagreement and lower intraclass correlation coefficients in pairwise comparisons of these lists. For this reason, and also because the inclusion of more acute conditions (rather than only chronic conditions, such as in the CIHI list) is likely important given the inclusion of younger age groups in our sample population, we have elected to use a more comprehensive list. In the absence of a single, universally recommended list, we have used Freund et al.’s list of 26 conditions [62], which incorporates stakeholder feedback, and also encompasses conditions on the Agency of Healthcare Quality list, as well as the 19 conditions commonly used by the National Health Service in Great Britain. These 26 conditions are: angina; asthma; cellulitis; CHF; convulsion and epilepsy; COPD; dehydration and gastroenteritis; dental conditions; diabetes; ear, nose and throat infections; gangrene; hypertension; influenza and pneumonia; iron-deficient anemia; nutritional deficiency; other vaccine preventable diseases; pelvic inflammatory disease; perforated / bleeding ulcer; and pyelonephritis, alcohol-related diseases, atrial fibrillation and flutter, constipation, fractured proximal femur, dyspepsia and other stomach function disorders, hypokalemia, and migraine/acute headache.
A recent systematic review of the literature on the relationship between socio-economic status and hospitalization for ACSCs from 1990 to 2018 summarized the findings from 31 studies, nine of which were conducted in Canada [63]. Some of the Canadian studies focused on hospitalization for particular conditions, such as hypertension [64, 65] or diabetes [66, 67] while others focused on multiple ACSCs [68,69,70]. Eight of these nine studies used area level measures, all of which found an inverse relationship between SES and hospitalization for ACSCs. Only one Canadian study cited in the review utilized an individual level measure of SES, education [71]. This study was based on a survey of asthma patients in Montreal from 2003 to 2007. The authors found that lower levels of education lead to higher morbidity among the asthma patients. The systematic review found a consistent association of lower SES and higher levels of hospitalization, particularly income, in all countries including Canada. The authors conclude the article by arguing that future studies on the relationship between SES and ACSC hospitalizations need to control for other socio-demographic variables, and should use individual-level measures of SES [63].
The authors of the systematic review later published an article using the linked CCHS-DAD data examining the effects of individual and neighbourhood socioeconomic status on avoidable hospitalizations in Canada [3]. They focused on adults age 18–74, and examined household income and area-level material deprivation (both of which were dichotomized into low/high).
We take advantage of the linked Census-DAD data to expand on this work in four ways. First, the larger sample size of the long form Census allows us to estimate more precise effects. Second, we examine the joint associations between education and income and hospitalization, not just income. Third, we compare the association between socioeconomic status and ‘avoidable’ hospitalizations with the association between socioeconomic status and non-acute care sensitive hospitalizations. And fourth, we examine three age groups (0–25 years old, 26–65 years old, and 66 + years old) separately. To our knowledge, we are the first researchers to use this unique dataset to examine the following research questions at the population level:
-
1.
What are the independent and joint associations between socio-economic inequalities (operationalized using individual-level Census measures of education and income) and hospitalization rates in Canada for children and youth, working-age adults, and older adults, controlling for other social factors such as immigrant status and race / ethnicity?
-
2.
Do the associations of socio-economic inequalities with hospitalization across age groups vary if we compare ambulatory-care sensitive hospitalizations with non-ambulatory care sensitive hospitalizations?
4 Methods
4.1 Data and design
We accessed the Census-DAD linked data files available in the Prairie Regional Research Data Centre in 2021. We utilized the data for 1 year, covering hospitalizations that occurred between April 1, 2006 and March 31, 2007 [18, 72]. The DAD, which is maintained by the Canadian Institute for Health Information (CIHI), provides discharge data from all inpatient care facilities across Canada, excluding Quebec. It contains approximately 3 million hospitalizations a year, representing approximately 2.5 million unique individuals [18]. The DAD contains detailed information on diagnoses (including the ‘most responsible diagnosis’), length of stay, interventions, and discharge locations. The DAD includes data from both live discharges and deaths.
The long-form Census is a 20% sample of the full population, with coverage estimated at 95–97% in the Provinces and 93–94% in the Territories. The long-form Census contains detailed demographic information at both the individual and the household level including age, sex, marital status, race/ethnicity, Indigenous status, immigration history, as well as detailed information on education, income, labour market activities, housing and migration.
The record linkage was conducted by Statistics Canada. The initial matching was done between the DAD and the short form census, using three pieces of unique identifying information common to both datasets: date of birth, sex, and postal code. Tax files were consulted for missing postal codes. The final dataset, which represents our cohort of interest, contains 4.65 million long-form respondents. We use weights provided by Statistics Canada to produce the national-level estimates. Approximately 5.3% of the long-form respondents were linked to at least one hospitalization over the three-year period [18].
Since hospitalization is a relatively rare event, it is difficult to assess the linkage accuracy. While the DAD is generally considered to capture most hospitalizations, we know that individuals may have been missing from either or both the long and short form Censuses, or their linkage may have been missed. However, coverage analysis assessing the extent to which the linked data represent the ‘expected’ health outcomes of the population of interest concludes that approximately 80% of hospital discharges are captured by the weighted data. A validation study conducted in 2015 concluded that the linked file is suitable for research, and that the file is broadly representative of the population of Canada [18].
4.2 Variables
Our dependent variable is any hospitalization in 2006–2007 for any reason other than pregnancy. We excluded pregnancy-related hospitalizations because of the differential impact of our independent variables of interest (income and education) on fertility rates. We divide hospitalizations into two types, ACSCs and non-ACSCs, using the Freund classification, as described above [62], to capture population-level hospitalization usage for both types of conditions. For individuals who were hospitalized more than once, we count only the first hospitalization. Our linked data include approximately 250,000 discharges for the year.
Our independent variables, taken from the long-form Census, include sex, age, marital status, immigrant status, rural/urban residence, race/ethnicity, income and education. Sex and age are reported for each individual in a Census household. Marital status is included for those age 25 and above, categorized as married, separated or divorced, widowed, or never married. Immigration status is based on the question “Were you born in Canada.” Those who answered no were classified as immigrants. Individuals were assigned as living in either an urban or a rural area based on their geographic location. In 2006, Statistics Canada defined ‘urban residence’ as living in a Census Metropolitan Area (CMA), a Census agglomeration (CA), or an urban area (classified as having at least 1,000 residents and a population density of at least 400 people per square kilometer) [73]. We use the Census data to control for the effects of race / ethnicity by categorizing respondents into three categories: White, Visible Minority, and Indigenous.
Our measure of income is based on total after tax household income (which includes government transfers), as reported on the Census long form. We adjusted the income measure for the household size (divided after tax total household income by the square root of the number of household members), and then divided it into quartiles. The quartiles represent the following income levels: Quartile 1—mean $12,513, 95% confidence interval $12,491–$12,536; Quartile 2—mean $28,311, 95% ci: $28,302-$28,320; Quartile 3—mean $44,838, 95% ci: $44,827–$44,849); and Quartile 4—mean $93,338, 95% ci: $93,078–$93,598.
For adults (over 18 years old), our measure of education is based on the highest level of education completed by the individual. For individuals aged 18 and younger, we used the level of education of the household head. Education level was divided into roughly four equal groups: less than high school; high school graduate; some post-secondary (including college or trade); and a Bachelor’s degree or higher.
We stratify our models by sex to account for the fact that men and women may be hospitalized at different rates for different reasons, and to examine the different associations of socioeconomic status with hospitalization by sex [47, 48]. Understanding the importance of a life course perspective on health [74], we also divide the respondents into three age groups and run the models separately for: children and young adults (ages 0–25); working age adults (26–65) and older adults (66 +). This allows us to see if the associations between socioeconomic status and hospitalization vary across the three age groups.
4.3 Statistical analyses
We first calculate age standardized hospitalization rates for both ACSCs and non-ACSCs by sex using the Spiegelman direct standardization method, stratified by gender, for each of the socio-demographic variables independently [75]. We used the age distribution of the Canadian population in 2006, based on 10-year age groups, with the last grouping containing all those aged 90 and above. We used the Fay and Feuer [76] method to calculate confidence intervals around the age standardized rates. For each demographic group, we then calculate the percentage of total hospitalizations that can be attributed to ACSCs.
We next perform logistic regression analyses, predicting both ACSC and non-ACSC hospitalization including all of the socio-demographic variables, for all three age groups, to try to isolate the associations with each of the variables. We applied the Census weights to create nationally representative results. All unweighted counts were rounded to the nearest 5, and all results were weighted, as per disclosure rules. All of our results were vetted by a committee of Statistics Canada Analysts.
5 Results
Weighted results show that the 4.65 million long-form Census respondents represent over 26 million Canadians (remembering that Quebec residents are excluded). Table 1 includes the distribution of the independent variables, for the sample overall and separately for men and women. The 2006 Canadian population self-identifies as 77% White, 19% visible minority and 4% Indigenous. Twenty-three percent are immigrants, and 80% live in urban areas. Women are slightly less likely than men to have the highest levels of education (some post-secondary of Bachelor’s degree and above) and slightly less likely than men to be in the top two income quartiles.
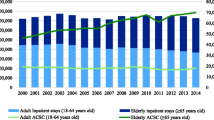
5.1 Hospitalization rates
The age-standardized hospitalization rates (ASHRs) for both ACSCs and non-ACSCs are presented in Table 2 for men and Table 3 for women. Across both sexes, we can see that both ACSC hospitalizations and non-ACSC hospitalizations are associated with all of the socio-demographic variables.
Examining the association of hospitalization with immigration status, immigrants are significantly less likely than non-immigrants to be hospitalized both for ACSCs and non-ACSCs. Area of residence also has an association with hospitalization rates. Men who live in rural areas are 29% more likely to be hospitalized for non-ACSCs (4576 versus 3555 per 100,000) and 169% more likely to be hospitalized for ACSCs (1037 versus 614 per 100,000) than men who live in urban areas. Women who live in rural areas are 36% more likely to be hospitalized for non-ACSCs (5296 versus 3882 per 100,000) and 179% more likely to be hospitalized for ACSCs (1135 versus 634 per 100,000) than women who live in urban areas.
The ASHRs for both men and women show that household income is inversely associated with hospitalizations for both non-ACSCs and ACSCs. Women and men living in households in the lowest income quartile are 40% and 30% more likely to be hospitalized for non-ACSCs than those in the highest income quartile, respectively. Women and men living in households in the lowest income quartile are over twice as likely to be hospitalized for ACSCs than those in the highest income quartile.
The association of education with hospitalization is also inverse, but only statistically significant at the extremes, when we compare the lowest and the highest educational groups. Women with less than a high school education are 77% more likely to be hospitalized for non-ACSCs than those with a Bachelor’s degree or above and over twice as likely to be hospitalized for ACSCs. Men with less than a high school education are 63% more likely to be hospitalized for non-ACSCs than those with a Bachelor’s degree or above and 246% more likely to be hospitalized for ACSCs. However, there is no difference in hospitalization rates between those with a high school diploma and those with some post-secondary education for either men or women.
Tables 2 and 3 thus highlight that the bivariate associations with the socio-demographic variables are consistently stronger for hospitalization for ACSCs than for non-ACSCs. Additionally, the association with the socio-demographic variables is somewhat stronger for women than for men with the exception of the association between income and education and ACSCs, which is stronger for men.
Tables 2 and 3 also contain data on the percent of all hospitalizations that are attributable to ACSCs (the final column of each table). Overall, 15.01% of all hospitalizations for women and 15.88% of all hospitalizations for men are attributable to ACSCs. However, this percentage varies greatly by social group. For example, 17.65% of hospitalizations for rural women and 18.47% of hospitalizations for rural men are attributable to ACSCs.
This figures again show an inverse relationship between income and hospitalization. A higher percentage of hospitalizations for those in the lowest income quartile and are due to ACSCs than for those in the highest income quartile for both women (there is a 5.39% difference between lowest and highest quartile) and men (there is a 7.06% difference between lowest and highest quartile). There is also a relationship between education and hospitalization for ACSCs, which is most evident when we compare those in the lowest versus the highest educational categories.
5.2 Multivariate regression models
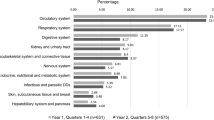
Tables 4 and 5 include the results from the multivariate models. Table 4 summarizes the results predicting hospitalization for non-ACSCs and Table 5 summarizes the results for ACSCs, separately for men and women across the three age groups. These models are adjusted for race/ethnicity, and are presented separately for the three age groups: children and youth (0–25 years old); working age adults (26–65 years old); and older adults (66 + years old).
Starting with Table 4, we note that in the multivariate models the associations with all of the socio-demographic variables remain significant for both men and women. These results indicate that multiple socio-demographic factors are associated with hospitalization for non-ACSCs (the majority of hospitalizations) in Canada, net of each other, for both men and women. The inverse association with income is clear for all groups except for males under the age of 26 and working age women aged 26–65 (where the inverse association is only significant when we compare the lowest and the highest quartiles). As we saw in the age standardized hospitalization rates, for most groups, the likelihood of being hospitalized decreases as income quartile rises, even when controlling for other variables.
The association with education is inverse for men, with each education level below Bachelor’s degree being less likely to be hospitalized for non-ACSCs, controlling for other variables, across all the age groups. However, the association of education with hospitalization for women shifts a bit once we control for the other socio-demographic variables. While there is still an association across all levels of education for females under 26, for older women (age 26 and above) the association is strongest at the extremes.
Table 5 shows that multiple social factors are also associated with hospitalization for ACSCs for both men and women across the three age groups. The inverse association with income is clear for both sexes across all age groups, with the likelihood of being hospitalized for ACSCs decreasing as income quartile rises. These associations are particularly striking for adults between 26 and 65, with men and women in the lowest income quartile over twice as likely to be hospitalized for ACSCs than men and women in the highest income quartile, even controlling for all the other sociodemographic variables. The association with income is stronger for the ACSC hospitalizations than for the non-ACSC hospitalizations, and strongest for the population aged 26–65.
The association of education with ACSC hospitalizations for children and youth is only significant at the extremes; those coming from households with less than high school education are 27% more likely to be hospitalized for ACSCs than those coming from households with a Bachelor’s or above. The association of education with hospitalization is strongest for working age men and women, and is stronger for ACSC hospitalizations than for non-ACSCs for all adults. Working age men and women with less than a high school education are over twice as likely to be hospitalized for ACSCs than those with a Bachelor’s or above, controlling for other sociodemographic variables.
Briefly examining the association of hospitalization with the other variables in the models, we note that the association with immigration status is consistent across all groups, with non-immigrants being more likely to be hospitalized for both ACSCs and non-ACSCs than immigrants, but these associations are reduced as we move into the older age groups. Similarly, the association of living in a rural residence with hospitalization is consistent for men and for women, with those living in rural areas more likely to be hospitalized than their urban counterparts. This association is also reduced across the age groups except for women over 65 and hospitalization for ACSCs. Older women living in rural areas are 30% more likely to be hospitalized for ACSCs than their urban counterparts, controlling for all other variables.
The association of marital status with hospitalization, which was only examined for those above age 25, is not consistent either across age group or across type of hospitalization. Focusing on working age adults, both men and women who are married are less likely to be hospitalized for ACSCs than those who are not married. However, never married women are half as likely as married women to be hospitalized for non ACSCs.
6 Discussion
With access to a unique linked dataset, combining Census data with health care administration data, we are able to take a detailed look at the socio-economic and demographic factors which are associated with hospitalization rates in Canada in the mid-2000s. We are further able to examine the differential independent and joint associations of these factors with hospitalization for ACSCs and non-ACSCs across three broad age groups, allowing us to speculate about the potential pathways through which these associations may operate.
We divide our discussion into three sections. The first two sections follow from our research questions. First we provide an overview of the independent and joint associations of socio-economic inequality with hospitalization rates in Canada across the age groups, controlling for other social factors such as immigrant status, marital status, residence, and race/ethnicity. Next, we analyze whether the association of socio-economic inequality with hospitalization varies when we compare ambulatory-care sensitive hospitalizations with non-ambulatory care sensitive hospitalizations. In the third section of our discussion, we summarize our findings regarding the association of hospitalization with other socio-demographic variables such as immigrant status, marital status, and rural residence for men and women.
6.1 Socio-economic inequality
Socio-economic inequality is strongly associated with hospitalization in Canada across all age groups. People from lower-income households and people with less education are more likely to be hospitalized, even when we control for other demographic factors known to be associated with hospitalization such as race/ethnicity, immigrant status, marital status, and rural residence. The association of income with hospitalizations for ACSCs is strikingly similar for women and men in all three age groups, with those from households in the lowest income quartile being more likely to be hospitalized for ACSCs than those from households in the highest income quartile. The association of income with hospitalization is less consistent for hospitalizations for non-ACSCs, and in fact there is no association between income and the likelihood of being hospitalized for non-ACSCs for males under age 26.
The association with education is also clearest for hospitalizations for ACSCs, and for adults. The association of education with hospitalization for non ACSCs for women is apparent at the extremes, but differences in hospitalization rates between the middle two education categories (high school graduate and some postsecondary) and those with at least a Bachelor’s are inconsistent.
The association of education and income with hospitalization that we saw in the bivariate age-standardized hospitalization rates is still present in the multivariate models. Recent work using linked survey and Canada Revenue data which examined the joint effects of education and income on self-rated health and physical and mental illness concluded that a proportion of the association between education and self-reported health outcomes was attributed to income [77]. Our results suggest education and income have independent associations with hospitalization. However, we do note that overall the more consistent and the stronger associations between income and hospitalization compared to education and hospitalization may suggest that the effects of social class on health care utilization in Canada may be more related to access to material resources, rather than knowledge or health literacy [78, 79].
6.2 ACSC versus non-ACSC hospitalizations
The association with socio-economic status is stronger for ACSC hospitalizations than for non-ACSC hospitalizations, both in the bivariate models (age-standardized rates) and in the multivariate models. To interpret this result, we consider what each type of hospitalization might represent. Hospitalization for non-ACSCs may reflect health and overall wellness or propensity to disease, while hospitalization for ACSCs may reflect access to primary and preventative health care [56, 60]. ACSC hospitalizations are considered ‘avoidable’ because the conditions leading to these hospitalizations can be treated and/or managed in the community. The stronger effects of socio-economic inequality on ACSC hospitalizations therefore suggests that socio-economic inequality may have a stronger effect on access to community-based health care than it does on propensity to disease.
This finding leads us to consult the research on barriers to access to primary care [80]. There are barriers that occur before accessing care (such as the local availability of primary care, time, transportation, costs) and then during accessing care (such as the care not being coordinated, not being well explained, language barriers) and then after accessing care (such as obtaining medication, adhering to medication, attending follow-up appointments) [81]. Almost all of this research concludes that vulnerable groups, including those with low income and low levels of education, face more barriers to care [82].
Inequalities in accessing primary care are well documented in Canada, too, despite the existence of universal health care [83,84,85]. A recent study in British Columbia found that access to primary care in British Columbia varied by neighbourhood SES (measured using income quintile) and that inequalities in access had actually increased from 1999 to 2018 [86]. Improving access to primary care requires interventions that address barriers at both the provider and the patient level [83].
6.3 Other socio-demographic variables
Overall, the associations between the socio-demographic variables and hospitalization are remarkably similar for men and women. Non-immigrants are approximately 16% more likely than immigrants to be hospitalized for non-ACSCs and approximately 30% more likely than immigrants to be hospitalized for ACSCs, net of all other variables. Men living in rural areas are 9% more likely than men living in urban areas to be hospitalized for non-ACSCs and 17% more likely to be hospitalized for ACSCs. Women living in rural areas are 25% more likely to be hospitalized for ACSCs than women living in urban areas. On the whole, marriage appears to be protective against hospitalization. However, there are some exceptions to this pattern. Never married women between the ages of 26 and 65 are less likely than married women to be hospitalized, net of other socioeconomic variables.
These findings mirror many of the findings in previous literature on social disparities in health in Canada [87], including research on sex differences in rural/urban discrepancies [51, 85], on the ‘healthy immigrant effect [2, 56]”, and on the generally positive association between marriage and health, but mixed findings on the relationship between marriage and health for women [49, 50].
As noted in the background section of the paper, much of this previous research on socio-economic disparities in health care utilization in Canada has utilized area-level measures. While there have been attempts to examine multiple social determinants of health at the area-level by using aggregated Census data to construct ‘Deprivation Indices’ which include both material and social variable (for example the Pampalon index [88], which includes the percent low income households and the percent of adults with less than a high school education in a given area), most of this research does not isolate the effects of either the socio-economic or the demographic variables. Marginalized groups are often marginalized in more than one aspect of their lives. By accounting for a variety of sociodemographic disparities, we are able to isolate the effects of each. Isolating these effects may help us better understand the mechanisms through which marginalization is linked to health care utilization in Canada.
6.4 Limitations
We acknowledge that the data used in the study are 15 years old. However, other research has shown that health inequities in Canada have not changed over time using area-based measures. Therefore we suspect that our results, although based on historic data, are likely to reflect current health inequities. Statistics Canada has plans to link more recent Census data with more recent hospital discharge data [89]. We hope to be able to repeat these analyses with more recent data as soon as it becomes available, and examine whether socio-economic inequalities in hospitalization have changed over time.
We note that the DAD data does not include data from Quebec, and also note that there are some inter-provincial variations in coverage. For example, DAD does not contain day surgery data from the provinces of Nova Scotia, Prince Edward Island, Ontario, and Alberta. Therefore,our data include hospitalizations for day surgery in all provinces except Nova Scotia, Prince Edward Island, Ontario and Alberta [90].
We also acknowledge that by only examining hospital discharge data, we are not capturing the prevalence of disease, or health care utilization more generally. We recognize that the list of ACSCs contains many conditions, and that we do not have any measures of pre-existing diagnoses, health care utilization before hospitalization, or health behaviours of individuals.
It is also important to note who might be missing from our linked data. The DAD does not contain information on day surgeries, psychiatric services, or emergency room visits that did not result in hospitalization. We must also remain aware of those who may have been mis-matched or missing through poor linkage. Linkage rates were not as good for younger people and for those living in the Territories. Overall, though, the linking process was robust, capturing over 80% of expected hospitalizations [18].
7 Conclusion
We examined the association between various socio-demographic factors and hospitalization in Canada across three broad age groups. We conclude that socio-economic disparities in ASHRs existed in the 2000s, and that education and income both have strong independent associations with the likelihood of hospitalization. Income appears to have a stronger association than education with hospitalizations—a relationship that persists when other socio-demographic factors are considered. These associations are stronger for working age adults than for older adults, suggesting that the Canadian public pension system for seniors may have an impact on reducing health inequalities for those over 65 [91]. These associations are also stronger for hospitalization for ACSCs than for non-ACSCs, suggesting that both education and income may both be related to access to primary care. The mechanisms through which education and income may affect access to primary care are many and varied. Thus, efforts to improve access to primary care should operate at several levels.
Improving access may require instituting changes directly in the health care system such as building more primacy care facilities in certain areas, extending opening hours, and allowing health care providers to spend more time with individual patients. It may also involve thinking more broadly about the barriers faced by those with lower income and lower education who attempt to access care such as transportation, language, time (being able to take time off work to access care for example), and health literacy (knowing how to take medications, for example).
We also wish to re-emphasize the importance of collecting individual-level data on socio-demographic characteristics alongside administrative health data. We encourage all of the agencies collecting health data to also include data on socio-demographic variables, especially income, education, immigration status, and race/ethnicity. Such data will be invaluable in understanding the social positioning of those who are currently accessing care, and in tracking change over time.
We would also like to encourage our data stewards (Statistics Canada and CIHI) to consider making more recent Census-DAD linked datasets available to researchers. The call for the provision of more socio-demographic data linked to data on health care utilization cannot be ignored. We cannot measure what we do not count, and we cannot address inequities in health care without first measuring what needs to be changed.
Availability of data and materials
The datasets analyzed during the current study are available through Statistics Canada, and were accessed at the Prairie Regional Data Centre at the University of Calgary. Information on accessing these datasets is available here: Census 2006—Discharge Abstract Database (DAD) Linked Data | Canadian Research Data Centre Network (https://www.crdcn.org) Researchers can apply to use the Census-DAD linked dataset in any Statistics Canada Research Data Centre (https://www.statcan.gc.ca/en/microdata/data-centres/data).
References
Frohlich KL, Ross N, Richmond C. Health disparities in Canada today: some evidence and a theoretical framework. Health Policy. 2006;79(2):132–43.
Boozary A, Laupacis A. The mirage of universality: Canada’s failure to act on social policy and health care. CMAJ. 2020;192(5):E105-106. https://doi.org/10.1503/cmaj.200085.
Wallar LE, Rosella LC. Individual and neighbourhood socioeconomic status increase risk of avoidable hospitalizations among Canadian adults: a retrospective cohort study of linked population health data. Int J Popul Data Sci. 2020;5(1):33.
Dalstra JA, Kunst AE, Borrell C, et al. Socioeconomic differences in the prevalence of common chronic diseases: an overview of eight European countries. Int J Epidemiol. 2005;34:316–26. https://doi.org/10.1093/ije/dyh386.
Mackenbach JP, Stirbu I, Roskam AJ, et al. Socioeconomic inequalities in health in 22 European countries. N Engl J Med. 2008;358:2468–81.
Kosteniuk JG, Dickinson HD. Tracing the social gradient in the health of Canadians: primary and secondary determinants. Soc Sci Med. 2003;57(2):263–76. https://doi.org/10.1016/S0277-9536(02)00345-3.
Raphael D, Labonte R, Colman R, Hayward K, Torgerson R, Macdonald J. Income and health in Canada: research gaps and future opportunities. Can J Public Health. 2006;97(Suppl 3):S16-23. https://doi.org/10.1007/BF03405393.
Lofqvist T, Burstrom B, Walander A, Ljung R. Inequalities in avoidable hospitalization by area income and the role of individual characteristics: a population-based register study in Stockholm County, Sweden. BMJ Qual Saf. 2014;23(3):206–14. https://doi.org/10.1136/bmjqs-2013-002591.
Gupta RP, Mukherjee M, Sheikh A, Strachan DP. Persistent variations in national asthma mortality, hospital admissions and prevalence by socioeconomic status and region in England. Thorax. 2018;73(8):706–12. https://doi.org/10.1136/thoraxjnl-2017-210714.
Kivimaki M, Vahtera J, Tabak AG, et al. Neighbourhood socioeconomic disadvantage, risk factors, and diabetes from childhood to middle age in the Young Finns study: a cohort study. Lancet Public Health. 2018;3:e365–73. https://doi.org/10.1016/S2468-2667(18)30111-7.
Laporte A, Nauenberg E, Shen C. Aging, social capital and health care utilization in Canada. Health Econ Policy Law. 2008;3(4):393–411. https://doi.org/10.1017/S1744133108004568.
Reading C, Wien F. Health inequalities and the social determinants of Aboriginal people’s health. Prince George: National Collaborating Centre for Aboriginal Health; 2013.
Martin D, Milley AP, Quesnal-Vallee A, Caron NR, Vissandjee B, Marchildon GP. Canada’s universal health-care system: achieving its potential. Lancet. 2018;391:1718–35. https://doi.org/10.1016/S0140-6736(18)30181-8.
Gone JP, Hartmann WE, Pomerville A, Wendt DC, Klem SH, Burrage RL. The impact of historical trauma on health outcomes for indigenous populations in the USA and Canada: a systematic review. Am Psychol. 2019;74(1):20–35. https://doi.org/10.1037/amp0000338.
Peters PS, Oliver LN, Carriere GM. Geozones: an area-based method for analysis of health outcomes. Health Rep. 2012;23(1):55–64.
Pichora E, Polsky JY, Catley C, Perumal N, Jin J, Allin S. Comparing individual and area-based income measures: impact on analysis of inequalities in smoking obesity and diabetes rates in Canadian 2003–2013. Can J Public Health. 2018;109(3):410–8. https://doi.org/10.17269/s41997-018-0062-5.
Buajitti E, Chiodo S, Rosella LC. Agreement between area- and individual-level income measures in a population-based cohort: implications for population health research. SSM-Popul Health. 2020;10: 100553. https://doi.org/10.1016/j.ssmph.2020.100553.
Rotermann M, Sanmartin C, Trudeau R, St-Jean H. Linking 2006 census and hospital data in Canada. Health Rep. 2015;26(10):10–20.
Geyer S, Hemstrom O, Peter R, Vagero D. Education, income and occupational class cannot be used interchangeably in social epidemiology. Empirical evidence against a common practice. J Epidemiol Commun Health. 2006;60(9):804–10. https://doi.org/10.1136/jech.2005.041319.
Chu LM, Pahwa P. Prevalence and associated factors for self-reported asthma in a Canadian population: the Canadian community Health survey, 2014. J Asthma. 2018;55(1):26–34. https://doi.org/10.1080/02770903.2017.1310228.
Wilk P, Stranges S, Bellocco R, Bohn T, Samouda H, Nicholson K, Makovski T, Maltby A. Multimorbidity in large Canadian urban centres: a multilevel analysis of pooled 2015–2018 cross-sectional cycles of the Canadian community health survey. J Multimorb Comorb. 2021;11:1–11. https://doi.org/10.1177/2F26335565211058037.
Srugo SA, Jiang Y, de Groh M. At-a-glance–living arrangements and health status of seniors in the 2018 Canadian community health survey. Health Promot Chronic Dis Prev Can. 2020;40(1):18–22. https://doi.org/10.24095/2Fhpcdp.40.1.03.
James PD, Wilkins R, Detsky AS, et al. Avoidable mortality by neighbourhood income in Canada: 25 years after the establishment of universal health insurance. J Epidemiol Commun Health. 2007;61:287–96. https://doi.org/10.1136/jech.2006.047092.
Nethery E, Schummers L, Maginley S, Dunn S, Norman WV. Household income and contraceptive methods among female youth: a cross-sectional study using the Canadian community health survey (2009–2010 and 2013–2014). CMAJ Open. 2019. https://doi.org/10.9778/cmajo.20190087.
Ravichandiran N, Mathews M, Ryan RL. Utilization of healthcare by immigrants in Canada: a cross-sectional analysis of the Canadian community health survey. BMC Prim Care. 2022. https://doi.org/10.1186/s12875-022-01682-2.
Godley J, McLaren L. Socio-economic status and body mass index in Canada: exploring measures and mechanisms. Can Rev Sociol. 2010;47(4):381–403. https://doi.org/10.1111/j.1755-618X.2010.01244.x.
Assari S, Bazargan M. Minorities’ diminished returns of educational attainment on hospitalization risk: National Health Interview Survey (NHIS). Hosp Pract Res. 2019;4(3):86–91. https://doi.org/10.15171/HPR.2019.17.
Tremblay M. The need for directly measured health data in Canada. Can J Public Health. 2004;95(3):165–8.
Hatef E, Kharrazi H, Nelson K, et al. The association between neighborhood socioeconomic and housing characteristics with hospitalization: results of a national study of veterans. J Am Board Fam Med. 2019;32(6):890–903. https://doi.org/10.3122/jabfm.2019.06.190138.
Nagasako EM, Reidhead M, Waterman B, Dunagan WC. Adding socioeconomic data to hospital readmissions calculations may produce more useful results. Health Aff (Millwood). 2014;33:786–91. https://doi.org/10.1377/hlthaff.2013.1148.
Nelson K, Schwartz G, Hernandez S, Simonetti J, Curits I, Fihn SD. The association between neighborhood environment and mortality: results from a national study of veterans. J Gen Intern Med. 2017;32:416–22. https://doi.org/10.1007/s11606-016-3905-x.
Mahmoudi E, Kamdar N, Kim N, Gonzales G, Singh K, Waljee AK. Use of electronic medical records in development and validation of risk prediction models of hospital readmission: systematic review. BMJ. 2020;369: m958. https://doi.org/10.1136/bmj.m958.
Gottlieb LM, Tirozzi KJ, Manchanda R, Burns AR, Sandel MT. Moving electronic medical records upstream: incorporating social determinants of health. Am J Prev Med. 2015;48:215–8. https://doi.org/10.1016/j.amepre.2014.07.009.
Bhavsar NA, Gao A, Phelan M, Pagidipati NJ, Goldstein BA. Value of neighborhood socioeconomic status in predicting risk of outcomes in studies that use electronic health record data. JAMA Netw Open. 2018;1: e182716. https://doi.org/10.1001/jamanetworkopen.2018.2716.
Johnson L, Cornish R, Boyd A, Macleod J. Socio-demographic patterns in hospital admissions and accident and emergency attendances among young people using linkage to NHS hospital episode statistics: results from the Avon Longitudinal study of parents and children. BMC Health Serv Res. 2019;1:134. https://doi.org/10.1186/s12913-019-3922-7.
Kivimaki M, Batty GD, Pentti J, Shipley MJ, Sipilia PN, Nyberg ST, Suominen SB, et al. Association between socioeconomic status and the development of mental and physical health conditions in adulthood: a multi-cohort study. Lancet Public Health. 2020;5:e140-149.
Hennessy DA, Soo A, Niven DH, Jolley RJ, Posadas-Calleja J, Stelfox HT, Doig CJ. Socio-demographic characteristics associated with hospitalization for sepsis among adults in Canada: a census-linked cohort study. Can J Anesth. 2020;67:408–20. https://doi.org/10.1007/s12630-019-01536-z.
Gupta N, Crouse DL. Social disparities in the risk of potentially avoidable hospitalization for diabetes mellitus: an analysis with linked census and hospital data. Can Stud Popul. 2019;46:145–59. https://doi.org/10.1007/s42650-019-00012-9.
Carriere G, Bougie E, Kohen D, Rotermann M, Sanmartin C. Ambulatory care hospitalization by Aboriginal identity, Canada, 2006 through 2008. Health Rep. 2016;27(8):3–11.
Rotterman M. Evaluation of the coverage of linked Canadian community health survey and hospital inpatient records. Health Rep. 2009;20(1):45–51.
Nejatinamini S, Godley J, Minaker LM, Sajobi TT, McCormack GR, Cooke MJ, Nykiforuk CIJ, de Koning L, Olstad DL. Quantifying the contribution of modifiable risk factors to socio-economic inequities in cancer morbidity and mortality: a nationally representative population-based cohort study. Int J Epidemiol. 2021;50:1498–511. https://doi.org/10.1093/ije/dyab067.
Taylor LA, Tan AX, Coyle CE, et al. Leveraging the social determinants of health: what works? PLoS ONE. 2016;11: e0160217. https://doi.org/10.1371/journal.pone.0160217.
Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health. 2011;32:381–98. https://doi.org/10.1146/annurev-publhealth-031210-101218.
Phelan JC, Link BG, Diez-Roux A, Kawachi I, Levin B. “Fundamental causes” of social inequalities in mortality: a test of the theory. J Health Soc Behav. 2004;45(3):265–85. https://doi.org/10.1177/2F002214650404500303.
Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Aff. 2002;21(2):60–76. https://doi.org/10.1377/hlthaff.21.2.60.
Pampel FC, Krueger PM, Denney JT. Socioeconomic disparities in health behaviors. Ann Rev Sociol. 2010;36:349–70. https://doi.org/10.1146/annurev.soc.012809.102529.
Pederson A, Raphael D. Gender, race and health inequalities. In: Raphael D, Bryant T, Rioux M, editors. Staying alive: critical perspectives on health, illness, and health care. Toronto: Canadian Scholars Press; 2006. p. 159–91.
Denton M, Prus S, Walters V. Gender differences in health: a Canadian study of the psychosocial, structural and behavioural determinants of health. Soc Sci Med. 2004;58:2585–600. https://doi.org/10.1016/j.socscimed.2003.09.008.
Chapman B, Guven C. Revisiting the relationship between marriage and wellbeing: does marital quality matter? J Happiness Stud. 2016;17:533–51. https://doi.org/10.1007/s10902-014-9607-3.
Ramezankhani A, Azizi F, Hadaegh F. Associations of marital status with diabetes, hypertension, cardiovascular disease and all-cause mortality: a long term follow-up study. PLoS ONE. 2019;14(4): e0215593. https://doi.org/10.1371/journal.pone.0215593.
Wanless D, Mitchell BA, Wister A. Social determinants of health for older women in Canada: does rural-urban residency matter? Can J Aging. 2010;29(2):233–47. https://doi.org/10.1017/S0714980810000140.
Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts methodologies, and guidelines. Annu Rev Public Health. 1997;18:341–78.
Godley J, Fundytus K, Stones C, Peller P, McLaren L. Survey research on health inequalities: exploring the availability of indicators of multiple forms of capital in Canadian datasets. Int J Public Health. 2021;66:584916. https://doi.org/10.3389/ijph.2021.584916.
Billings J, Zeitel L, Lukomnik J, Carey TS, Blank AE, Newman L. Impact of socioeconomic status on hospital use in New York City. Health Aff. 1993;12(1):162–73. https://doi.org/10.1377/hlthaff.12.1.162.
Billings J, Anderson GM, Newman LS. Recent findings on preventable hospitalizations. Health Aff (Millwood). 1999;15(3):239–49. https://doi.org/10.1377/hlthaff.15.3.239.
Canadian institute for health information. Ambulatory care sensitive conditions. Ottawa. ON. 2018. https://www.cihi.ca/en/indicators/ambulatory-care-sensitive-conditions. Accessed 20 Sept 2022.
Sanchez M, Vellanky S, Herring J, Liang J, Jia H. Variations in Canadian rates of hospitalization for ambulatory care sensitive conditions. Healthc Q. 2008;11(4):20–2. https://doi.org/10.12927/hcq.2008.20087.
Anderson GM, et al. Common conditions considered sensitive to ambulatory care. In: Goel V, et al., editors. Patterns of health care in ontario. 2nd ed. Ottawa: CMA; 1996. p. 104–10.
Agency for healthcare research and quality. Quality indicators. 2021. https://qualityindicators.ahrq.gov/Downloads/Resources/Publications/2021/Empirical_Methods_2021.pdf. Accessed 20 Sept 2022.
Purdy S, Griffin T, Salisbury C, Sharp D. Ambulatory care sensitive conditions: terminology and disease coding need to be more specific to aid policy makers and clinicians. Public Health. 2009;123(2):169–73. https://doi.org/10.1016/j.puhe.2008.11.001.
Pinto A, Santos JV, Souza J, Viana J, Costa Santos C, Lobo M, Freitas A. Comparison and impact of four different methodologies for identification of ambulatory care sensitive conditions. Int J Environ Res Public Health. 2020;17(21):8121. https://doi.org/10.3390/ijerph17218121.
Freund T, Campbell SM, Geissler S, Kunz CU, Mahler C, Peters-Klimm F, Szecsenyi J. Strategies for reducing potentially avoidable hospitalizations for ambulatory care-sensitive conditions. Ann Fam Med. 2013;11(4):363–70. https://doi.org/10.1370/afm.1498.
Wallar LE, De Prophetis E, Rosella LC. Socioeconomic inequalities in hospitalizations for chronic ambulatory care sensitive conditions: a systematic review of peer-reviewed literature, 1990–2018. Int J Equity Health. 2020. https://doi.org/10.1186/s12939-020-01160-0.
Aube-Maurice J, Rochette L, Blais C. Divergent associations between incident hypertension and deprivation based on different sources of case identification. Chronic Dis Inj Can. 2013;32(3):121–30.
Walker RL, Chen G, McAlister FA, Campbell NRC, Hemmelgarn BR, Dixon E, et al. Hospitalization for uncomplicated hypertension: an ambulatory care sensitive condition. Can J Cardiol. 2013;29(11):1462–9. https://doi.org/10.1016/j.cjca.2013.05.002.
Shulman R, Luo J, Shah BR. Mental health visits and low socio-economic status in adolescence are associated with complications of type 1 diabetes in early adulthood: a population-based cohort study. Diabet Med. 2018;35(7):920–8. https://doi.org/10.1111/dme.13633.
Booth GL, Hux JE. Relationship between avoidable hospitalizations for diabetes mellitus and income level. Arch Intern Med. 2003;163(1):101–6. https://doi.org/10.1001/archinte.163.1.101.
Disano J, Goulet J, Muhajarine N, Neudorf C, Harvey J. Social-economic status and rates of hospital admission for chronic disease in urban Canada. Can Nurse. 2010;106(1):24–9.
Lemstra M, Neudorf C, Opondo J. Health disparity by neighbourhood income. Can J Public Health. 2006;97(6):435–9. https://doi.org/10.1007/BF03405223.
Roos LL, Walld R, Uhanova J, Bond R. Physician visits, hospitalizations, and socioeconomic status: ambulatory care sensitive conditions in a Canadian setting. Health Serv Res. 2005;40(4):1167–85. https://doi.org/10.1111/j.1475-6773.2005.00407.x.
Bacon SL, Bouchard A, Loucks EB, et al. Individual-level socioeconomic status is associated with worse asthma morbidity in patients with asthma. Respir Res. 2009;10:125. https://doi.org/10.1186/1465-9921-10-125.
Canadian Institutes of Health Information (CIHI). Discharge Abstract Database Metadata. Accessed 12 Sept 2022.
Statistics Canada. Dissemination Geography Unique Identifier: Definition and Structure. 2019. https://www150.statcan.gc.ca/n1/pub/92f0138m/92f0138m2019001-eng.htm. Accessed 30 Oct 2022.
Kuh D, Shlomo YB. A life course approach to chronic disease epidemiology. Oxford: Oxford University Press; 2004.
Spiegelman M. Introduction to Demography: revised edition. Cambridge: Harvard University Press; 1968.
Fay MP, Feuer EJ. Confidence intervals for directly standardized rates: a method based on the gamma distribution. Stat Med. 1997;16:791–801. https://doi.org/10.1002/(SICI)1097-0258(19970415)16:7%3C791::AID-SIM500%3E3.0.CO;2-%23.
Veenstra G, Vanzella-Yang A. Does household income mediate the association between education and health in Canada. Scand J Public Health. 2020;49(8):857–64. https://doi.org/10.1177/2F1403494820917534.
Stringhini S, Sabia S, Shipley M, Brunner E, Nabi H, Kivimaki M, et al. Association of socioeconomic position with health behaviors and mortality. JAMA. 2010;303(12):1159–66. https://doi.org/10.1001/jama.2010.297.
Schillinger D, Barton LR, Karter AJ, Wang F, Adler N. Does literacy mediate the relationship between education and health outcomes: a study of a low-income population with diabetes. Public Health Rep. 2006;121(3):245–54. https://doi.org/10.1177/003335490612100305.
Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q Health Soc. 1973;51(1):95–124.
Corscadden L, Levesque JF, Lewis V, Strumpf E, Breton M, Russell G. Factors associated with multiple barriers to access to primary care: an international analysis. Int J Equity Health. 2018;17:28. https://doi.org/10.1186/s12939-018-0740-1.
Spooner C, Lewis V, Scott C, Dahrouge S, Haggerty J, Russell G, Levesque J-F, Dionne E, Stocks N, Harris MF. Improving access to primary health care: a cross-case comparison based on an a priori program theory. Int J Equity Health. 2021;20:223. https://doi.org/10.1186/s12939-021-01508-0.
Sanmartin C, Ross N. Experiencing difficulties accessing first-contact health services in Canada. Health Policy. 2006;1(2):103–19.
Clarke J. Difficulty accessing health care services in Canada. Ottawa: Statistics Canada; 2016. Catalogue No. 82–624-X.
Sibley LM, Weiner JP. An evaluation of access to health care services along the rural-urban continuum in Canada. BMC Health Serv Res. 2011. https://doi.org/10.1186/1472-6963-11-20.
Lavergne M, Bodner A, Peterson S, et al. Do changes in primary care service use over time differ by neighbourhood income? Population-based longitudinal study in British Columbia, Canada. Int J Equity Health. 2022;21:80. https://doi.org/10.1186/s12939-022-01679-4.
Public Health Agency of Canada. Social determinants of health and health inequalities. 2020. https://www.canada.ca/en/public-health/services/health-promotion/population-health/what-determines-health.html. Accessed 21 Sept 2021.
Pampalon R, Gamache P, Hamel D. A Deprivation Index for health in Canada. Quebec City: Institut national de santé publique du Québec; 2006.
Availability of research data in Statistics Canada Research Data Centres. https://www.statcan.gc.ca/en/microdata/data-centres/data. Accessed 6 July 2022.
Canadian Institute for Health Information. Data quality documentation, discharge abstract database. Last Accessed 2 September 2022. https://www.cihi.ca/sites/default/files/document/dad-data-quality_14-15_en.pdf. Accessed 2 Sept 2022.
McIntyre L, Dutton DJ, Kwok C, Emery JCH. Reduction of food insecurity among low-income Canadian seniors as a likely impact of a guaranteed annual income. Can Public Policy. 2016;42(3):274–86. https://doi.org/10.3138/cpp2015-069.
Acknowledgements
These results were previously presented at the International Population Data Linkage Network Conference in 2018. We wish to thank Dr. William Ghali for comments on an earlier version of the paper, and the Statistics Canada staff in the Prairie Regional Data Centre for all of their expertise and assistance.
Funding
None to declare.
Author information
Authors and Affiliations
Contributions
JG and KT conceptualized and designed the study. JG did the statistical analysis and wrote the first draft of the paper. Both authors read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The University of Calgary Conjoint Faculties Research Ethics Board waived the requirement for local ethics review as the data were collected by Statistics Canada, and use of the data is covered by the Canadian Statistics Act. https://laws-lois.justice.gc.ca/eng/acts/S-19/FullText.html In accordance with the Canadian Tri-Council Policy Statement on the Ethical Conduct for Research Involving Humans (TCPS2, 2018), Article 2.2, this research was exempt from ethics review because it relies on information that is “publicly available through a mechanism set out by legislation or regulation and that is protected by law.” (TCPS2, p. 15). All participants gave informed consent when their data was collected by Statistics Canada.
Consent for publication
The authors give consent for publication.
Competing interests
None to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Godley, J., Tang, K.L. Income, education, and hospitalization in Canada: results from linked census and administrative data. Discov Soc Sci Health 2, 19 (2022). https://doi.org/10.1007/s44155-022-00023-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44155-022-00023-z