Abstract
Background
The impact of informal caregiving is increasingly recognised as an important but often particularly neglected area of research in low and middle income countries. It is important to understand not only the effect of care on patient outcomes, but also the impact of caring on caregivers’ health and wellbeing.
Methods
Guided by the Arksey and O’Malley (Res Methodol 8:19–32, 2005) framework, this scoping review sought to collate and chart existing research on the needs, burdens and challenges experienced by caregivers in Uganda.
Results
The results of this review indicate that research focusing on the needs of caregivers for individuals with communicable disease, particularly HIV, has been well developed in Uganda, however, there is a lack of research on caregiving related to non-communicable diseases. Research has been dominated by small qualitative studies that are informative for understanding roles, burdens and contextually-specific aspects of care, but there is a need for larger studies that develop and test interventions designed to support the needs of caregivers.
Conclusions
Recurrent themes identified within this review, such as challenges in providing physical support and accessing treatment services, financial costs of care, psychological and mental health impacts and the experience of stigma, should help to inform well targeted and contextually-appropriate future research and interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Globally, caregivers experience high levels of burden. Challenges often relate to both the activity of care and the impact caring has on their own health [1, 2]. Research, however, remains limited on how care is experienced in Low and Middle Income Countries (LMICs) [3], and no review of research on the needs of caregivers has been undertaken in Uganda. This scoping review sought to collate and chart existing research on the needs, burdens and challenges experienced by caregivers in Uganda and sought to identify common themes and research gaps that could inform future research and interventions in this important area.
The health system in Uganda continues to experience challenges in service delivery, with patients often experiencing multiple barriers to accessing services. These include medication supplies, distance, staff shortages, and costs [4]. An estimated 35% of deaths in Uganda are attributed to non-communicable diseases [5] with this number expected to continue to rise in the future. Given the increased burden of non-communicable diseases (NCDs) [6, 7] and that Uganda is experiencing the beginning of an epidemiological transition, we also discuss whether needs related to caring for someone with an NCD in Uganda differ from those of caring for someone with communicable disease. The findings from this research may also be of relevance to other resource-constrained settings.
2 Methods
The scoping review was conducted according to the five-stage process described by Arskey and O’Malley [8]: identifying a research question; searching for relevant studies; selecting studies; charting the data; and collating, summarizing and presenting the results. To identify relevant studies, we searched the Titles and Abstracts of articles indexed in MEDLINE, Web of Science, PsychInfo, African Journals Online, and Social Policy and Practice using the keywords ‘Carers’ OR ‘Caregivers’ AND ‘Uganda’. Additional searches for grey literature from NGO (Non-Governmental Organisations) and Government reports and policies, were undertaken. The search was conducted from database inception through to 22 June 2020.
Inclusion criteria included studies and documents related to the needs, challenges and burden of care in Uganda; or interventions, policies and projects to address the needs, challenges and burden of caregivers in Uganda. All health condition types were included in the review. There were no language restrictions applied. Exclusion criteria included studies on needs of Ugandan caregivers who are migrants living in other countries; studies in which outcomes for caregivers were not described, measured or evaluated; and studies in which a specified health condition was not mentioned [9]. Abstracts, poster presentations, study protocols and studies only presenting aggregated data from multi-country studies were excluded. Studies solely on the roles of caregivers without discussion of needs and challenges were excluded [10,11,12] as were studies on care in the context of HIV but not explicitly caring for someone with HIV [13, 14] (e.g. grandparents caring for children orphaned by HIV), and studies focusing solely on challenges regarding disclosure of HIV status [15].
To select studies for inclusion, two researchers independently screened each Title and Abstract against the eligibility criteria and collaboratively resolved any conflicts with a third member of the research team. Full texts of accepted articles were then screened against the inclusion criteria. Data on study methods, study participants, region, and outcomes of each study were extracted and verified by a second reviewer. Data was charted, based on health condition, region and methods used, before a more detailed examination of key outcomes for caregivers. Screening and data extraction was managed using Covidence software. Thematic categories were inductively identified regarding different challenges and needs and were validated and agreed by the entire research team [16]. This process was guided by Green and Thorogood and involved collaborative familiarization, identification, coding, organising, and validating of all the data extracted from each study [15].
3 Results
A total of 40 articles were included in our review (see Table 1). Of these, 38 were sourced from international databases and 2 from the grey literature (see Fig. 1). Articles disproportionately focused on the needs of caring for someone with HIV (n = 16); with other articles exploring care related to cancer (n = 2); nodding syndrome (n = 4); malaria (n = 3); depression (n = 1); severe mental illness e.g. schizophrenia (n = 2); dementia (n = 2); Ebola (n = 2); sickle cell disease (n = 1); stroke (n = 1); spina bifida (n = 1); palliative care (n = 1); and disability (general) (n = 1). Four articles looked at a combination of health conditions; for example, cancer and HIV.
Methodologically, most of the studies completed were either qualitative designs (n = 26) or cross-sectional survey designs (n = 8). Remaining design types included mixed/multi method designs (n = 1); cluster randomised trials (n = 2); non-randomised trials (n = 1); rapid evaluation design (n = 1); and case study design (n = 1). Studies were spread evenly across Uganda, with most taking place in hospital-based facilities in Kampala (n = 9). Seven studies compared different areas (normally rural/urban comparisons). Half the studies (n = 20) were conducted between 2016 and 2020; with ten conducted between 2011 and 2015; eight between 2006 and 2010; and two prior to 2005. Most studies reviewed the roles, needs and challenges of women as caregivers, although a small number of other studies focused on the roles of men, children and the elderly.
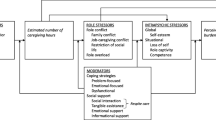
All identified studies focused on the needs of informal caregivers (those not in professional employment). Five themes identified from the reviewed articles included: the extensive and essential roles provided by caregivers, and the burden of care (including economic burden, practical daily challenges, providing support for treatment with limited knowledge of the patient’s health condition). The papers in our review described the impact of care on caregivers’ quality of life, mental health, and the extended family. In addition, caregivers reported experiencing stigma and discrimination, relationship challenges, and receiving variable levels of support. Additional themes identified included the prevalence of reciprocal care relationships and the importance of coping mechanisms and peer support.
3.1 The extensive and essential role of caregivers
Roles of caregivers in Uganda are described as both extensive and essential in supporting the health of individuals they care for. In broad terms, these roles include counselling, administering medication, supporting logistics around hospital appointments; doing day-to-day household tasks like cooking, washing clothes, shopping; and providing social support and companionship [17]. Caregiving is described as an act of caring, helping, welcoming, nurturing and attending to the needs of others [18]. Studies in our review highlight specific roles in supporting palliative care regarding providing economic support, nutrition and food, and bereavement support [12], and that often such roles are supported by wide community networks and systems.
Care is often provided by family members, with studies indicating that care was often provided by women, spouses, grandparents and children. Women play more active caring roles than men in many of the studies we reviewed [19,20,21] with some participants describing caring as a full-time job [22]. In one study on malaria, male involvement in caring was described as centering on the purchasing of medication and food supplies, provision of water, and transport for the sick person to the clinic and paying for medical expenses, while care provided by women often involved household tasks and emotional support [23].
Family and community networks were described as essential in a number of studies on how care is conceptualised and undertaken. Streid et al. [24] in their study among HIV and cancer caregivers describe care as being provided to children in the community particularly when there were multiple cases of HIV infection in the same family. In a rural sub-county in Masaka District, however, Seeley et al. [25] challenged the assumption that the extended family provides a safety net for individuals in times of need. This theme was echoed by Nakigudde et al. [26] and Matua & Van der Wal [27] and appears to be a specific sub theme related to stigmatised illnesses, for example nodding syndrome and epileptic conditions.
Care, particularly related to HIV, was described as reciprocal between grandparents and children, with children with HIV depending on grandparents for material support, basic and health needs; and grandparents relying on children to do household tasks [28]. Most of the studies in this review were focused on care at home, and/or care in the community, highlighting the lack of institutional support for caregiving outside of Kampala-based and specialised health centres. Additional common themes present across the reviewed studies were marginalisation and isolation of caregivers, and a lack of specific recognition from the formal health system [29,30,31].
3.2 The economic burden of care
Lack of economic resources and the financial burden of care were consistently highlighted themes within studies. Caregivers across studies described struggling to afford medicine, transport, and costs associated with staying with people admitted to hospital. Caregivers in Districts with older populations in southwestern Uganda (Nyakabungo in Kabale, Kasharira in Ntungamo, and Nyakakoni in Mbarara) described financial stress related to the need for food, medication, and transport costs to the clinic or hospital. Sadigh et al. [32] for example, found that informal caregivers in Mulago Hospital’s internal medicine wards were economically burdened by having insufficient funds to buy prescriptions.
Financial stress was compounded by the inability to work due to increasing caregiver requirements in the home [32, 33]. Providing care was described by participants in one study as all-encompassing, stating that “ogoye gima katho malo” (nothing can continue) when a child is sick [34]. Similar themes were described by caregivers of children with nodding syndrome in Hoima and Kampala who reported that in the absence of healthcare services or support groups, full-time caregiving was done at the expense of other activities that could help support the home such as finding paid work [35]. Across different health conditions, caregivers were described as having to make the challenging decisions on whether to prioritise the needs of the healthy children over those of their sick child [26, 36].
3.3 Practical daily challenges
Across the reviewed studies caregivers expressed a variety of challenges in providing daily care and supporting treatment of family members. For caregivers providing care in an in-patient setting, challenges were described as a lack of sanitation, lack of mosquito nets, infection control, and heat. Lack of bedding and seating were reported as pressing difficulties. Lack of toilet sanitation was voiced as a crucial concern, as well as the close proximity of toilet facilities to beds. The large number of beds packed close together without curtains for partition was described as inhibiting privacy and infection control, which was compounded by the admission of patients with a variety of conditions to the same wards. Providing care within this environment was described as challenging [28, 32].
Studies also highlighted numerous challenges in providing care in the home and community. In one study on caring for a child with mental ill health and HIV, caring was described as a complex process that included taking children to multiple providers, procuring and appropriately administering medicine or home remedies, and continually monitoring [37]. In another study girls were taken out of school if help with care was needed, demonstrating the disruptive nature of providing care on other areas of life such as education.
3.4 Impact of care on emotions, mental health and Quality of Life
A number of studies indicated significant mental health challenges and impact on QoL related to caregiving roles [38]. These challenges were similar in nature across disease type, and largely stemmed from the emotional impact of caregiving. In one study on the health of caregivers caring for someone with severe mental illness such as schizophrenia, bipolar affective disorder and major depressive disorder at the National Referral Hospitals of Uganda, 49% reported being very dissatisfied with their state of health. Of the 300 caregivers that participated in the study, 172 (57.30%) had a poor QoL. QoL decreased with increasing age of the participants; while it increased with physical health, psychological wellbeing, environment, and social relationships [39]. For carergivers of someone with cancer, Kizza and Muliira [37] reported low Quality of Life (QoL) in the domains of burden (50.7%), disruptiveness (53.5%), and support (56.7%), while family caregivers of patients with dementia in the Rukiga and Rubanda districts of southwestern Uganda reported not having enough time for themselves [40].
Other studies described the challenges of coping with the stress and emotion associated with seeing their child ill, such as crying, kumo (sorrow), pain in the heart, and most predominantly, worry or ka paro teki teki (over thinking) [34]. Anxiety and depression were commonly reported, particularly in male caregivers in studies on people caring for someone with a cancer diagnosis [41], while helplessness, desperation, isolation, fear and sadness were reported by caregivers of people who had contracted Ebola [27]. Chronic sorrow, grief-related feelings, sadness, shock, confusion, despair, fear, devastation, pain, anger, were all described by caregivers of people with schizophrenia [42].
3.5 Experiences of stigma and discrimination
Caregivers of particular conditions described experiencing stigmatization, discrimination and social isolation within both communities and families. This was described by caregivers caring for someone with poor mental health [34], schizophrenia [42], Ebola [27], nodding syndrome [26] and HIV [22, 43]. Experiences of stigmatization led to caregivers reporting similar themes of living in fear, ostracism, and social isolation. Isolation often compounded challenges of providing care by reducing support from the community and family members.
Positive changes were noted with some conditions such as HIV, in which stigmatization was reported by some study participants as having reduced over time. Caregivers associated this change with the spread of the epidemic and that many families have been affected by HIV/AIDS, and therefore it was no longer new within the community. Others reported stigma is still prevalent among many households making it difficult for people to disclose their HIV/AIDS diagnosis and for caregivers to provide care and avail of support from the wider community [22].
4 Discussion
The majority of studies examined within this review focused on the needs of caregivers providing care for someone living with HIV/AIDS. Given the scale of the impact of the HIV pandemic on Ugandan communities this may be expected. However, as Uganda undergoes the beginnings of an epidemiological transition with the increasing burden of NCDs [7] and as caring for the needs of people with other long-term, chronic conditions becomes more common, more research will be required to understand the specific challenges that arise from the management of e.g. cancer, diabetes and stroke. Most of the literature returned by this review indicated that research on NCDs has largely been located in specialised centres in Kampala. Needs of caregivers in the community and in rural areas are less well understood. This is a significant research gap, not just regarding the health of caregivers, but also for patient outcomes given the fundamental role informal caregivers play [2].
Literature from other contexts suggests that long-term care is expensive and requires technical skills and knowledge creating specific burdens on caregivers [3]. While literature on HIV in Uganda likely provides insights into themes around long-term care and stigma, specific and targeted research on other conditions would be beneficial in informing the design of future policies, interventions and services. Unlike HIV, programmatic support for caregivers of people suffering other ill health are likely less developed, as demonstrated by our analysis within this review. This likely deepens all challenges associated with life-long care. Research that has focused on NCDs suggests that care is demanding across all domains of daily life, finances, and emotional and mental health. The long-term nature of care for many NCDs often has life-shaping consequences for caregivers, particularly for women given the often gendered nature of care. Given that this scoping review has suggested that the burden of care in Uganda often falls on women, and that girls may be taken out of school to support caregiving thus exacerbating existing gender inequalities, further research within the area is essential.
The incidence of NCDs are rising yet there is limited understanding of its impact on families in low middle income countries. The development, testing, and evaluation of services designed to support caregivers should be considered an urgent priority. While in resource-constrained contexts it is understandable that funding priorities are often directed towards patients given their immediate needs, international research has demonstrated the importance of caregivers in the health and wellbeing of patients [1]. Other studies have demonstrated the importance of culturally tailoring interventions for caregivers, given the specific ways that care is conceptualized in different contexts [44].
Other research gaps also exist. This review has indicated that there is a relatively large amount of qualitative data related to informal caregiving in Uganda. Only a small number of large-scale surveys, and an even smaller number of trials have been undertaken. Larger datasets that quantify the scale of this challenge, and studies exploring the economic impact of care would be hugely valuable, given that one avenue for supporting caregivers may be providing financial assistance.
This scoping review has provided an insight into common themes and challenges experienced by caregivers in Uganda. A strength of this review is that data was analyzed by a diverse and multidisciplinary team with expertise across cancer, social care and different methodologies. Grey literature and a wider number of databases were additionally searched, thus providing a fuller picture of all available data. Limitations included that studies were not quality checked, as is the norm with scoping reviews. As a result, caution and further research is required when interpreting these results.
5 Conclusion
Irrespective of age, gender, and type of illness, caregivers of individuals with chronic conditions in Uganda face similar challenges. Caregivers are not only challenged to support daily care and treatment of unwell family members, but also experience distress and financial hardship. Time and effort is invested in caring and in turn caregivers’ quality of life and economic livelihoods are often affected and disrupted, with caregivers also often experiencing stigma and discrimination. Interventions, programmes and policies addressing the needs of caregivers of individuals with chronic illnesses should be further developed, with clear strategies on how to improve support to caregivers given their crucial and often invisible role.
Data availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Abbreviations
- AIDS:
-
Acquired immune deficiency syndrome
- HIV:
-
Human immunodeficiency virus
- NCDs:
-
Noncommunicable diseases
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- QoL:
-
Quality of Life
References
Northouse LL, Katapodi MC, Schafenacker AM, Weiss D. The impact of caregiving on the psychological well-being of family caregivers and cancer patients. Oncol Fam Caregiv. 2012;28(4):236–45.
Stenberg U, Ruland CM, Miaskowski C. Review of the literature on the effects of caring for a patient with cancer. Psychooncology. 2010;19(10):1013–25.
Treanor CJ, Santin O, Prue G, Coleman H, Cardwell CR, O’Halloran P, et al. Psychosocial interventions for informal caregivers of people living with cancer. Cochrane Database Syst Rev. 2019;6(6):CD009912.
Koutsoumpa M, Odedo R, Banda A, Meurs M, Hinlopen C, Kramer K, et al. Health workforce financing in Uganda: challenges and opportunities. Eur J Public Health. 2020;30(5):ckaa165-525.
Ministry of Health, Uganda. Non-Communicable Disease Risk Factor Baseline Survey: Uganda 2014 Report. Ministry of Health Uganda; 2014.
Meghani A, Ssemugabo C, Pariyo G, Hyder AA, Rutebemberwa E, Gibson DG. Curbing the rise of noncommunicable diseases in Uganda: perspectives of policy actors. Glob Health Sci Pract. 2021;9(1):149–59.
Schwartz JI, Guwatudde D, Nugent R, Kiiza CM. Looking at non-communicable diseases in Uganda through a local lens: an analysis using locally derived data. Glob Health. 2014;10(1):77.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Matovu SN, Wallhagen MI. Perceived caregiver stress, coping, and quality of life of older Ugandan grandparent-caregivers. J Cross-Cult Gerontol. 2020;35(3):311–28.
Nankinga PN, Maling S, Chemali Z, Wakida EK, Obua C, Okello ES. Informal support for people with Alzheimer’s disease and related dementias in rural Uganda: a qualitative study. Int J Ment Health Syst. 2020;14(1):33.
Ntozi JPM. AIDS morbidity and the role of the family in patient care in Uganda. Health Transit Rev. 1997;7:1–22.
Mburu G, Oxenham D, Hodgson I, Nakiyemba A, Seeley J, Bermejo A. Community systems strengthening for HIV care: experiences from Uganda. J Soc Work End-Life Palliat Care. 2013;9(4):343–68.
Nabunya P, Ssewamala FM, Ilic V. Family economic strengthening and parenting stress among caregivers of AIDS-orphaned children: results from a cluster randomized clinical trial in Uganda. Child Youth Serv Rev. 2014;44:417–21.
Matovu S, Rankin S, Wallhagen M. Ugandan Jajjas: antecedents and rewards of caring for grandchildren in the context of HIV. Int J Older People Nurs. 2020;15:e12304.
Kiwanuka J, Mulogo E, Haberer JE. Caregiver perceptions and motivation for disclosing or concealing the diagnosis of HIV infection to children receiving HIV care in Mbarara, Uganda: a qualitative study. PloS ONE. 2014;9(3): e93276
Green J, Thorogood N. Qualitative methods for health research. 4th ed. New York: Sage Publications; 2018.
Muhwezi WW, Okello ES, Neema S, Musisi S. Caregivers’ experiences with major depression concealed by physical illness in patients recruited from central Ugandan primary health care centers. Qual Health Res. 2008;18(8):1096–114.
Kizza IB, Maritz J. Family caregivers for adult cancer patients: knowledge and self-efficacy for pain management in a resource-limited setting. Support Care Cancer. 2019;27(6):2265–74.
Hartley S, Ojwang P, Baguwemu A, Ddamulira M, Chavuta A. How do carers of disabled children cope? The Ugandan perspective. Child Care Health Dev. 2005;31(2):167–80.
Osafo J, Knizek BL, Mugisha J, Kinyanda E. The experiences of caregivers of children living with HIV and AIDS in Uganda: a qualitative study. Glob Health. 2017;13(1):72–72.
Mugisha JO, Schatz E, Seeley J, Kowal P. Gender perspectives in care provision and care receipt among older people infected and affected by HIV in Uganda. Afr J AIDS Res. 2015;14(2):159–67.
Kipp W, Tindyebwa D, Rubaale T, Karamagi E, Bajenja E. Family caregivers in rural Uganda: the hidden reality. Health Care Women Int. 2007;28(10):856–71.
Taylor L, Seeley J, Kajura E. Informal care for illness in rural southwest Uganda: the central role that women play. Health Transit Rev. 1996;6:49–56.
Streid J, Harding R, Agupio G, Dinat N, Downing J, Gwyther L, et al. Stressors and resources of caregivers of patients with incurable progressive illness in Sub-Saharan Africa. Qual Health Res. 2014;24(3):317–28.
Seeley J, Kajura E, Bachengana C, Okongo M, Wagner U, Mulder D. The extended family and support for people with AIDS in a rural population in south west Uganda: a safety net with holes? AIDS Care. 1993;5(1):117–22.
Nakigudde J, Mutamba BB, Bazeyo W, Musisi S, James O. An exploration of caregiver burden for children with nodding syndrome (lucluc) in Northern Uganda. BMC Psychiatry. 2016;16(1):255.
Matua GA, Wal DMVD. Living under the constant threat of ebola: a phenomenological study of survivors and family caregivers during an ebola outbreak. J Nurs Res. 2015;23(3):217–24.
Rutakumwa R, Zalwango F, Richards E, Seeley J. Exploring the care relationship between grandparents/older carers and children infected with HIV in south-western Uganda: implications for care for both the children and their older carers. Int J Environ Res Public Health. 2015;12(2):2120–34.
Buchmann K. “These nodding people”: experiences of having a child with nodding syndrome in postconflict Northern Uganda. Epilepsy Behav. 2015;42:71–7.
Kassam R, Sekiwunga R, MacLeod D, Tembe J, Liow E. Patterns of treatment-seeking behaviors among caregivers of febrile young children: a Ugandan multiple case study. BMC Public Health. 2016;16:160–160.
Park S-J, Akello G. The oughtness of care: fear, stress, and caregiving during the 2000–2001 Ebola outbreak in Gulu. Uganda Soc Sci Med. 2017;194:60–6.
Sadigh M, Nawagi F, Sadigh M. The economic and social impact of informal caregivers at Mulago National Referral Hospital, Kampala, Uganda. Curr Top Glob Health. 2016;82(5):866–74.
Owokuhaisa J, Rukundo GZ, Wakida E, Obua C, Buss SS. Community perceptions about dementia in southwestern Uganda. BMC Geriatr. 2020;20(1):135–135.
Murray SM, Familiar I, Nakasujja N, Winch PJ, Gallo JJ, Opoka R, et al. Caregiver mental health and HIV-infected child wellness: perspectives from Ugandan caregivers. AIDS Care. 2017;29(6):793–9.
Nasuuna E, Kigozi J, Muwanguzi PA, Babirye J, Kiwala L, Muganzi A, et al. Challenges faced by caregivers of virally non-suppressed children on the intensive adherence counselling program in Uganda: a qualitative study. BMC Health Serv Res. 2019;19(1):150–150.
Grant L, Brown J, Leng M, Bettega N, Murray SA. Palliative care making a difference in rural Uganda, Kenya and Malawi: three rapid evaluation field studies. BMC Palliat Care. 2011;10(1):8.
Kizza IB, Muliira JK. Determinants of quality of life among family caregivers of adult cancer patients in a resource-limited setting. Support Care Cancer. 2020;28(3):1295–304.
Wadhwa D, Burman D, Swami N, Rodin G, Lo C, Zimmermann C. Quality of life and mental health in caregivers of outpatients with advanced cancer. Psychooncology. 2013;22(2):403–10.
Ndikuno C, Namutebi M, Kuteesa J, Mukunya D, Olwit C. Quality of life of caregivers of patients diagnosed with severe mental illness at the national referral hospitals in Uganda. BMC Psychiatry. 2016;16(1):400.
Ainamani HE, Alele PE, Rukundo GZ, Maling S, Wakida EK, Obua C, et al. Caring for people with dementia in rural Uganda: qualitative study of caregiving burden experienced by informal and formal caregivers. J Glob Health Rep. 2020;4:e2020038.
Katende G, Nakimera L. Prevalence and correlates of anxiety and depression among family carers of cancer patients in a cancer care and treatment facility in Uganda: a cross-sectional study. Afr Health Sci. 2017;17(3):863–76.
Olwit C, Musisi S, Leshabari S, Sanyu I. Chronic sorrow: lived experiences of caregivers of patients diagnosed with Schizophrenia in Butabika Mental Hospital, Kampala, Uganda. Arch Psychiatr Nurs. 2015;29(1):43–8.
Rispel LC, Cloete A, Metcalf CA. “We keep her status to ourselves”: experiences of stigma and discrimination among HIV-discordant couples in South Africa, Tanzania and Ukraine. SAHARA J. 2015;12(1):10–7.
Santin O, Jenkins C, Nghiem HLP, Prue G, Reid J, Lohfeld L, et al. The development of a web-based resource to provide information and psychosocial support to informal cancer carers in hospitals in Vietnam. Psychooncology. 2020;29(5):920–6.
Funding
Department for the Economy (DfE)—Global Challenge Research Fund (GCRF) Awards, 2020/21 Round.
Author information
Authors and Affiliations
Contributions
AK and CJ lead the analyzing of data and writing of the paper; AK, CJ, PA, FG, FN, AE, CMcS, and LM supporting screening of articles; AK, CJ, FN, PA, FG, AE, JA, AKN, OS, MM, McS, CM, LM and RCN analysed data collaboratively; and RCN, LM, and CM supervised and managed the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Komuhangi, A., Jenkins, C., Nakaggwa, F. et al. The needs, challenges, and burden experienced by informal caregivers in Uganda: a scoping review. Discov Soc Sci Health 2, 1 (2022). https://doi.org/10.1007/s44155-022-00004-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44155-022-00004-2