Abstract
Objectives
Our aim was to compare Health Link utilization in urban and rural Alberta by metrics relevant to the ED.
Methods
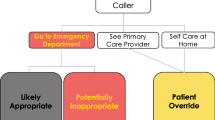
Data on Health Link callers from January 1, 2018–December 31, 2019 was extracted from the National Ambulatory Care Reporting System, including postal code, location of ED attended, Canadian Triage Acuity Scale (CTAS) assigned at ED, age, and self-identified gender. Usage density (presentations/100/year), patient demographics (age, self-identified gender), and ED metrics (CTAS, investigations, admission) were compared for Health Link ED referrals and direct ED visits.
Results
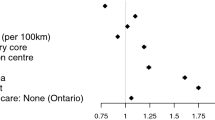
In this period, 900,196 individuals called Health Link, 241,103 were referred to the ED, 58% (140,614) of which presented to the ED within 24 h of their call. These referrals constituted 3.4% of the total ED visit population (4,194,735). Looking at the density of ED utilization, this is greater in rural than urban settings with respect to patients who present directly to the ED (90.9 vs. 36.5 presentations/100/year). There is a sparser density of Health Link ED visits in rural settings than in urban centres (1.5 vs. 1.6).
Urban ED presentations were more often triaged as a CTAS 1–3 than a CTAS 4–5 if they had presented after a Health Link referral (76.0% CTAS 1–3) than a direct ED visit (63.0% CTAS 1–3). This effect is greater for rural patients, who also more likely to present as a CTAS 1–3 than a CTAS 4–5 if they were referred through Health Link (61.1% CTAS 1–3) compared to those who directly went to the ED (39.0% CTAS 1–3).
Conclusions
This study on Health Link describes how tele-health can often triage higher acuity patients to appropriately receive ED level care, which may be important for future development of health care and ED infrastructure.
Résumé
Objectifs
Notre objectif était de comparer l'utilisation de Health Link dans les zones urbaines et rurales de l'Alberta en fonction de paramètres pertinents pour l'urgence.
Méthodes
Les données sur les appelants de Health Link du 1er janvier 2018 au 31 décembre 2019 ont été extraites du Système national d'information sur les soins ambulatoires, y compris le code postal, le lieu de l'urgence fréquentée, l'échelle canadienne de triage et de gravité (ETG) attribuée à l'urgence, l'âge et le sexe auto-identifié. La densité d'utilisation (présentations/100/an), les caractéristiques démographiques des patients (âge, sexe déclaré) et les paramètres des urgences (ETG, investigations, admission) ont été comparés pour les orientations vers les urgences de Health Link et les visites directes aux urgences.
Résultats
Au cours de cette période, 900 196 personnes ont appelé Health Link, 241 103 ont été dirigées vers les urgences, dont 58 % (140 614) se sont présentées aux urgences dans les 24 heures suivant leur appel. Ces renvois représentaient 3,4 % du nombre total de visites aux urgences (4 194 735). La densité d'utilisation des urgences est plus élevée dans les zones rurales que dans les zones urbaines en ce qui concerne les patients qui se présentent directement aux urgences (90,9 contre 36,5 présentations/100/an). La densité des visites aux urgences de Health Link est plus faible dans les zones rurales que dans les centres urbains (1,5 contre 1,6).
Les patients qui se présentaient aux urgences en milieu urbain étaient plus souvent classés dans l'ETG 1-3 que dans l'ETG 4-5 s'ils avaient été orientés par Health Link (76,0 % ETG 1-3) que s'ils s'étaient rendus directement aux urgences (63,0 % ETG 1-3). Cet effet est plus important pour les patients des zones rurales, qui sont également plus susceptibles de présenter un ÉTG 1-3 qu'un ÉTG 4-5 s'ils ont été orientés par Health Link (61,1 % d'ÉTG 1-3) que s'ils se sont rendus directement aux urgences (39,0 % d'ÉTG 1-3).
Conclusions
Cette étude sur Health Link décrit comment la télésanté permet souvent de trier les patients les plus graves pour qu'ils reçoivent les soins appropriés au niveau des urgences, ce qui peut être important pour le développement futur des infrastructures de soins de santé et des urgences.
Similar content being viewed by others
Data availability
The data that support the findings of this study are not openly available due to privacy consideration with Alberta Health Services.
References
Ho K, Lauscher HN, Stewart K, Abu-Laban RB, Scheuermeyer F, Grafstein E, et al. Integration of virtual physician visits into a provincial 8-1-1 health information telephone service during the COVID-19 pandemic: a descriptive study of HealthLink BC Emergency iDoctor-in-assistance (HEiDi). CMAJ Open. 2021;9(2):E635–41.
Hall Dykgraaf S, Desborough J, de Toca L, Davis S, Roberts L, Munindradasa A, et al. “A decade’s worth of work in a matter of days”: the journey to telehealth for the whole population in Australia. Int J Med Inf. 2021;151: 104483.
Letourneau S. Health link Alberta: a model for successful health service integration. Healthc Q. 2009;13:56–60.
Services AH. Health Link [Internet]. Alberta Health Services. [Cited 2023 Jan 16]. Available from: https://www.albertahealthservices.ca/info/Page12630.aspx
Nataraj J, Stempien J, Netherton S, Wahba MY, Oyedokun TO. Emergency department referrals from a provincial medical call centre: is it more than just 1–800-go-to-emerg? Can J Emerg Med. 2020;22(2):241–4.
O’Connell JM, Towles W, Yin M, Malakar CL. Patient decision making: use of and adherence to telephone-based nurse triage recommendations. Med Decis Mak Int J Soc Med Decis Mak. 2002;22(4):309–17.
Lewis J, Stone T, Simpson R, Jacques R, Okeeffe C, Croft S, et al. Patient compliance with NHS 111 advice: analysis of adult call and ED attendance data 2013–2017. PLoS ONE. 2021;16(5):251362 (Ashkenazi I, editor).
Tran DT, Gibson A, Randall D, Havard A, Byrne M, Robinson M, et al. Compliance with telephone triage advice among adults aged 45 years and older: an Australian data linkage study. BMC Health Serv Res. 2017;17(1):512.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schmaus, A., Cooper, I.R., Whitten, T. et al. Impact of Health Link utilization on emergency department visits. Can J Emerg Med 25, 429–433 (2023). https://doi.org/10.1007/s43678-023-00504-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43678-023-00504-3