Abstract
Annona squamosa is a medicinal plant that has been used in folk medicine since antiquity. The goal of this study is to see how effective Annona squamosa leaf extract (A.S.L.E) or its niosomal-entrapped preparation is at protecting skin from UVA irradiation. The prepared niosomal-entrapped A.S.L.E has been characterized via spectrophotometry and transmission electron microscopy imaging. Furthermore, the entrapment efficiency and in vitro release of A.S.L.E were determined. In this study, ex vivo and freshly prepared samples from the dorsal region of the rats’ skin were used as biological samples, which were divided into five groups: control UVA-unexposed, unprotected UVA-exposed, A.S.L.E-protected UVA-exposed, and niosomal-entrapped A.S.L.E UVA-exposed. UVA irradiation was performed by exposing the skin samples to a UVA-producing lamp for 4 h. Samples from various groups were then examined using FTIR spectroscopy, histopathology, and protein electrophoresis methods. The results showed that A.S.L.E has a skin protective effect against UVA irradiation. The niosomal-entrapped A.S.L.E was more effective than the native plant leaf extract in protecting skin from the damaging effects of UVA. Therefore, the nanotechnologically formulated preparation, niosomal-entrapped A.S.L.E, can be used as an effective photoprotector (sunscreen) against the adverse effects of UVA radiation.
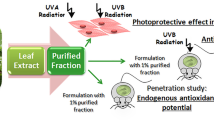
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Ultraviolet (UV) rays coming from the sun threaten the skin health of human beings. Skin erythema can occur as a result of prolonged exposure to UVB (280–320 nm) rays. While exposure to UVA (320–400 nm) has a cumulative effect that ultimately producing photo-aging and/or skin cancer [1, 2].
Because of the discomfort associated with the use of physical sunscreens, people prefer to use chemical sunscreens [3, 4]. However, most synthetic chemical sunscreens are unstable under UV irradiation and can be photo-degraded producing free radicals [4,5,6,7]. Free radicals accelerate the photo-aging of the skin and induce cells damage by coupling products [8,9,10].
Plant products were the basis for treating human diseases in traditional medicine. Nowadays, the natural pharmaceuticals, food, and cosmetics products industry aiming to develop new drugs by investigating biologically active compounds obtained from plant species [11, 12]. Annona squamosa is a fruit tree that belongs to the Annonaceae family. It grows in different countries around the world. This plant has been reported as a rich source of therapeutic potential compounds [13]. Its extract is a rich origin of phenolic compounds which can act as a free radical scavenger.
Annona squamosa leaf extracts (A.S.L.E) proved to have anti-inflammatory [14,15,16,17,18], antifungal [19, 20], anti-bacterial [21, 22], and antiviral [23] activities. Furthermore, there are many agents from A.S.L.E that are active against cancer [24,25,26].
Tannins, steroids, saponins, phenols, and flavonoids are among the active compounds found in the extract of different parts of A.S.L.E. These compounds can scavenge and reduce the cellular free radicals’ adverse effects [27,28,29,30]. However, the presence of these compounds depends on the solvents used for the extraction and the plant part used for the study [31].
Nanocarriers introduced development in drug delivery concerning its protection from degradation, controlled release, and increase in drug bioavailability [32]. Niosomes are non-ionic surfactant vesicles that are used in the delivery of both hydrophilic and hydrophobic drugs. Niosomes are considered as a promising drug carrier with several advantages such as high stability, small purity variability, and biocompatibility, in addition to their economic and simple production [33]. Therefore, entrapping of active compounds in niosome vesicles could enhance its efficacy and avoid some of its undesired properties.
The present study aims to examine the skin protective effect of the native A.S.L.E and niosomal-entrapped A.S.L.E against UVA radiation exposure. To this end, several techniques were implemented: FTIR spectroscopy, histopathological investigation, and protein electrophoresis.
2 Materials and methods
2.1 Materials
Methanol was purchased from Fisher Scientific UK. Phosphate buffer tablets pH 7.4 (purity ≥ 99%) was purchased from Bio Shop Canada Inc. Ethanol (purity ≥ 99.7%), Tween 80 (purity ≥ 99%) and cholesterol (M Wt. 386.65, purity ≥ 99.7%) were purchased from Sigma Aldrich.
2.2 Extraction method
Annona squamosa leaves were collected from a local Farm (Giza, Egypt). The leaves of the plant were washed with tap water to clean them of dust. The leaves were air-dried for three days and then oven-dried at 55 °C and an electric mixer was used to crush them into powder [34]. The formed powder was stored in clean plastic bags. A 15 g of the powder (A.S. leaves) were extracted with 60 ml of methanol and distilled water (8:2), Then the extract was centrifuged (655×g for 15 min). The supernatant was then collected and filtered by Whatman No. 1. Finally, the solvents were evaporated with a rotary evaporator (RV05-ST, Germini BV laboratory) at 45 °C to obtain the concentrated extract. The yield of the extraction was based on the powder used in the beginning [35].
2.3 Preparation of A.S.L.E-entrapped niosomes
Niosomes nanoparticles were prepared by the hydration method. The surfactant tween 80 and cholesterol were dissolved in ethanol in the ratio of 2:1 in a round flask with a 1 ml of A.S.L.E. A dry thin film was formed after evaporation of ethanol using a rotary evaporator at 50 rpm at 45 °C under reduced pressure. The formed thin film was hydrated using phosphate buffer saline (PBS) (pH 7.4) to form niosomes which subjected to sonication (WUC-A03H, Daihan, Korea) for 5 min to produce small niosomes vesicles. A high-speed cooling centrifuge (VS-18000 M, Korea) (8809×g for 30 min) was used to precipitate niosomes [36].
2.4 Transmission electron microscopy (TEM)
The image of niosomes was investigated using TEM (JEOL JEM.1230, Japan). Niosomes suspension-entrapped extracts sample was negatively stained with a 1% of phosphotungstic acid and left to air-dry, then sample was incubated for approximately 10 min on the grid, and then analyzed.
2.5 Spectrophotometry
The absorption spectra of A.S.L.E, niosomal-entrapped A.S.L.E, and Phenylbenzimidazole-5-sulfonic acid (PBSA) were determined using UNICO UV-2000 spectrophotometer, China.
2.6 Entrapment efficiency
The centrifugation method was used to determine the capacity of niosomes to entrap A.S.L.E [37]. Samples were centrifuged (10,483×g for 30 min) (VS-18000 M, Korea), to separate the supernatant from the pellets containing the free extract or the encapsulated extract. The supernatant was collected, while the resulting pellets were diluted with saline (10 ml, pH 7.4) and sonicated for 5 min for further use. Each process was repeated three times. The A.S.L.E absorbance was measured at 270 nm at different concentrations using a UV–Vis spectrophotometer (JENWAY 6405, U.K.). The calibration curve of A.S.L.E was made by plotting the absorbance against different concentrations of the extract. The absorbance of the free A.S.L.E in the supernatant was determined at 270 nm spectrophotometrically. The entrapment efficiency for niosomes was calculated from the following Eq. [38]:
2.7 In vitro release
The dialysis technique was used to find in vitro release of A.S.L.E from niosomes in PBS (pH 7.4) [39, 40]. Two milliliters of niosomes-entrapped A.S.L.E suspension were put into a cellulose acetate dialysis bag (Spectra/Por, MW cutoff12,000, Spectrum, Canada) and immersed in 100 ml of PBS with magnetically stirring at 50 rpm (Model TK22, Kartell, Italy). One milliliter was taken at fixed time intervals (every 1 h) of the immersed solution, replacing it with an equal volume of fresh PBS. The samples absorbance was measured at 270 nm using UNICO UV-2000 spectrophotometer, China. The experiment was ended when the concentration of the extract in the receiving medium became constant (i.e., a plateau was obtained in the absorption curve).
2.8 The experimental design
The experiment was carried out using fresh skin samples of adult albino male rats weighing ~ 120 g. The skin was obtained from the dorsal skin of recently scarified (decapitated under anesthesia) animals and cut into small pieces of same dimensions (5 × 3 cm2). Then samples were divided into four groups (5 samples /group). The first group represents the control unexposed group, the second group was exposed to UV radiation (UV lamps: Bioblock Scientific, Illkirch, France, λ = 365 nm, P = 6 W) without protection. The radiant energy was measured with a radiometer (VLX-3 W; Cole-Parmer, Vernon Hills, Ill., USA) with a microprocessor, equipped with two variable sensors. The total UV radiation dose reaching the skin was 1.667 J/cm2. The distance between the source and the skin surface was 8 cm and the exposure time was 4 h. The hair on the rat’s skin was removed using a depilatory cream and the niosomal preparations were applied directly on the skin in equal amounts. In the third and fourth groups, 0.5 ml of A.S.L.E or niosomes-entrapped A.S.L.E was applied to the skin, and samples were then subjected to UVA irradiation, respectively. The exposure of the third and fourth groups was carried out under the same conditions as the second group.
2.9 Fourier-transform infrared spectroscopy (FTIR)
FTIR spectra were measured on lyophilized skin samples. Tissues were grounded with KBr at a ratio of 1:100 and are pressurized with a hydraulic press under a pressure of 15,000 lbs. The pellets of the samples have been scanned over the spectrum range 400–4000 cm−1 by type A FT/IR-4100 (A Basic Vector, Germany).
2.10 Histopathology
Skin samples were kept in 10% neutral formalin and then were inserted into paraffin blocks. Samples were sectioned into very thin pieces at 4–5 µm thickness and stained with hematoxylin and eosin (H&E) [41, 42]. Sections were investigated by an optical microscope (BX50Olympus microscope, Tokyo, Japan) and captured using Olympus DP27 camera linked to cell Sens dimensions software (Olympus).
2.11 One-dimensional sodium dodecyl sulfate gel electrophoresis (1D SDS-PAGE)
1D SDS-PAGE was performed to observe protein bands in the skin tissue sample. 100 mg of each sample were homogenized with 300 µl saline and were then subjected to cooling centrifugation (VS-18000 M, Korea, power 220 V/50 Hz) (12,303×g for 30 min at 4 °C). 100 µl from the supernatant proteins were mixed with 500 µl acetone and left overnight at − 20 °C. Before measurement, samples were centrifuged at 12,303×g for 3 min at 4 °C. Proteins were diluted with sample buffer (10% SDS, 20% Glycerol, 0.2 M trispH6.8, 10 mM beta-mercapto-ethanol, and 0.05% bromophenol blue) at the ratio of 1:4 and were then heated for 5 min at 95 °C. Proteins were loaded into the well of kD™ Mini-PROTEAN® TGX™ Precast Gel (Bio-Rad, Hercules, CA), and were run with Mini-PROTEAN electrophoresis cells (Bio-Rad, Hercules, CA) at 80 V for 4 h. EZ-Run Pre-stained Rec Protein Ladder (Fisher Bioreagents, Pittsburgh, PA) containing proteins from 16 to 270 kDa was used as a protein marker. Gels were stained with staining solution (50% dH2O, 40% methanol, and 10% glacial acetic acid) [43].
3 Results
3.1 Niosomal-entrapped A.S.L.E characterization
3.1.1 Transmission electron microscope
TEM examination showed non-aggregated nanoparticles with spherical shape of the prepared A.S.L.E-entrapped niosomes as shown in Fig. 1, the average size of the prepared niosomal-entrapped A.S.L.E was 100 ± 2 nm.
3.1.2 Spectrophotometry
The UV–Vis spectrum of A.S.L.E, niosomal-entrapped A.S.L.E, and PBSA (standard) is presented in Fig. 2. As shown in the figure, A.S.L.E and niosomal-entrapped A.S.L.E have a broad peak in the UV wavelength range (200–400 nm) compared to the commercial compound that is used as a reference material (PBSA).
3.1.3 Entrapment efficiency
Niosomes exhibit a high efficiency for entrapping A.S.L.E. The calculated average percentage of entrapping efficiency was 90 ± 3%. The high entrapment efficiency could be attributed to the high affinity of A.S.L.E to the bilayers of niosomes.
3.1.4 In vitro release
The release of A.S.L.E from the dialysis bag was rapid and reached equilibrium within 4 h (Fig. 3) due to its particles were unrestricted and had freedom of movement. The release of A.S.L.E from niosomes took a longer time interval (Fig. 3) since A.S.L.E was located within the niosome. It is worth mentioning that our formulation has been designed to prolong the release of A.S.L.E as the nano-entrapment saves the extract from premature degradation, improves its solubility, and promotes controlled release. The sustained release of A.S.L.E from niosomes is shown in Fig. 3. The release was measured at room temperature, pH 7.4 in PBS buffer and within 12 h. A.S.L.E is released steadily and slowly over the period of the experiment which supports that niosomes are good stable carriers for the sustained release of A.S.L.E and this could reinforce the therapeutic effects of A.S.L.E. Niosomes leading to a lower diffusion compared to diffusion seen in A.S.L.E alone, which encourages their release for long periods. This emphasizes that niosomes are good vehicles for the sustained release of A.S.L.E.
A.S.L.E in methanol solvent contain alkaloids, phenols, flavonoids, carbohydrate and tannins compounds as reported in Tables 1, 2. This screening reveals that A.S.L.E has several bioactive chemical compounds which may be useful in the discovery of new pharmacological drugs, especially against UV exposure [29].
3.2 FTIR spectroscopy analysis
FTIR analysis is an informative technique, and it could be used for skin damage detection. The average IR spectra were recorded for all samples in the range of 4000–400 cm−1.Transmission spectra of the different group samples are shown in Fig. 4.The broad peak at approximately 3430 cm−1 corresponds to the amide A band of hyaluronic acid due to N–H stretching vibrations. This band decreases in intensity due to degradation in the hyaluronic acid chain. Peaks showed a decrease in the intensity in the unprotected UVA-exposed skin samples with respect to the control unexposed samples.
Peaks at 2926 and 2856 cm−1 correspond to absorption caused by C–H, N–H, and O–H single bonds from Lipid. As shown in Fig. 4, a great increase in these bands’ intensity was observed in the spectra of skin samples exposed to UVA radiation without protection. Interestingly, niosomal-entrapped A.S.L.E peak in this region looks very similar to the UVA-unexposed skin samples. The band at 2856 cm–1 is indicated to branched alkyl chain. Due to the exposure to UVA radiation, free alkyl radicals were produced.
There were strong C=O, C=N, C=C, and C–H stretching bands in the region 2000 cm−1–1500 cm−1 which belonging to Amide I band (1600–1780 cm−1). The absorption band at1750 cm−1 which is characteristic of the carbonyl (C=O) stretching vibrations of ester bonds in membrane phospholipids. Protein secondary structures appear in amide I band. All samples have peaks at 1640 cm−1 refers to proteins with random coil conformation and overlapping with 1648–1660 cm−1 corresponds to the alpha helix. In the unprotected sample, there is an increase in the peak at 1745 cm−1 which assigns to the presence of the β-structure band and turns indicating the increase in the β-structure protein content compared to the control group [44].
The spectral fingerprint region (1500 to 400 cm−1) contains a large number of peaks due to fatty acids, amino acids, phospholipids, polysaccharides, symmetric stretching modes, PO2 and C-O-C vibrations groups (1163 cm−1). There is an increase in the observed 1163 cm−1 band in the unprotected sample and a slight increase in the protected with A.S.L.E sample compared to the control group indicating a reduction in the amount of hydrogen-bonded C-OH groups of cellular proteins and an accumulation of carbohydrates.
3.3 Histopathological analysis
Figure 5 shows the histopathological results of the skin samples of the different groups and the effects of UV exposure on the tissue structure. Photomicrographs of the skin samples exposed to UVA radiation without protection showed thickening of stratum corneum (hyperkeratosis), parakeratosis, and hypertrophy of epidermal cell layer (yellow arrow) with edema in the dermis (red arrow) which were associated with few inflammatory cells infiltration and necrosis of dermal collagen. Skin samples protected with A.S.L.E showed a focal necrosis of dermal collagen, slight thickening of stratum corneum, and slight hypertrophy of epidermal cell layer after exposure to UVA radiation. Therefore, these histopathological findings revealed that A.S.L.E was unable to fully protect the skin from the destructive effects of UVA radiation.
Photomicrograph of normal H & E stained (scale bars 100 µm and 25 µm, magnification × 100) skin sections taken from the dorsal skin of the rats. A Normal, showing normal epidermal and dermal layers. B irradiated with UV for 4 h showing thickening of stratum corneum (hyperkeratosis) (black arrow), hypertrophy of epidermal cell layer (yellow arrow), and necrosis of dermal collagen (blue arrow). C treated with annona free and UV irradiated for 4 h showing slight thickening of stratum corneum (black arrow), slight hypertrophy of epidermal cell layer (yellow arrow), and focal necrosis of dermal collagen (blue arrow). D treated with niosomal A. Squamosa for 4 h showing no or slight histopathological alterations
On the other hand, normal epidermal and dermal layers with no histopathological alterations were obtained in control unexposed skin samples and in samples protected with niosomes-entrapped A.S.L.E after a continuous exposure for 4 h of UVA. Thus, the histopathological investigation indicated that the niosomal A.S.L.E is, on structural basis, capable of protecting the skin from the adverse effects of UVA irradiation.
3.4 Electrophoresis results
Figure 6 shows the different protein patterns obtained via gel electrophoresis of the skin samples in different groups. Clear differences have been obtained in the protein pattern of skin samples irradiated with UVA without protection with respect to the control unexposed samples. Changes have been obtained in case of A.S.L.E used in protecting skin samples. However, only negligible changes appeared in the skin samples protected by niosome-entrapped A.S.L.E.
SDS-PAGE pattern of protein in C = control UVA-unexposed skin samples, UV = Skin samples exposed to UVA for 4 h, AS + UV = A. Squamosa leaf extract protected UV-exposed skin, and NAS + UV = Skin samples protected with niosomal-entrapped A. Squamosa leaf extract and exposed for 4 h to UVA radiation. M = Protein marker
4 Discussion
The photo-damaging effect of UV radiation from sunlight or artificial sources is a dermatological problem that affects many populations worldwide [45, 46]. UVA in the range from 320 to 400 nm is absorbed in the skin tissues and reaches the dermal layer producing reactive oxygen species (ROS) that cause lipid peroxidation in the cell membrane leading to skin aging, inflammation, and melanoma [47, 48]. Therefore, protecting the skin from these adverse effects is crucial for healthy skin and the whole health of the subject.
Annona squamosa is a plant that grows in many places worldwide. A.S.L.E has a broad absorption band in the UV region [49]. This property makes this natural material a good candidate for the protection of biological tissues from the adverse effects of UV radiation exposure. To investigate this hypothesis in the present study, ex vivo skin samples were exposed under controlled conditions to UVA radiation with and without protection by A.S.L.E and compared to the unexposed skin samples. Furthermore, to enhance the efficacy of this natural material a nanosized entrapment has been implemented via the preparation of niosomes as a nanocarrier loaded with A.S.L.E.
Niosomal-entrapped A.S.L.E offers several advantages over the native material when it is used to cover the skin for protection. It increases the duration of the existence of the active material over the skin as indicated from its long-time release compared to the native compound. Moreover, it facilitates with its nanosize the transdermal entrance of the material into the skin layers [50,51,52] and therefore provides deep protection to the skin structure.
The present study utilized different techniques to investigate the protective effects of A.S.L.E and its niosomal-entrapped preparation on skin samples irradiated for 4 h with the UVA lamp. FTIR spectroscopy, histopathological, and protein electrophoresis data revealed several structural changes in the unprotected skin samples exposed to UVA radiation. Oxidative stress, hyaluronic degradation, and protein secondary structure changes are the main alterations in the UV-exposed skin samples in the present/ work. The FTIR intense amide A band of hyaluronic band for skin samples protected with niosomes-entrapped A.S.L.E could be assigned to the significant preserving potential of the nano-formulated for the skin internal structure. Furthermore, increase in lipid bands in UVA-irradiated skin indicates that the membrane environment has changed, and the surrounding matrix has become more lipophilic, and this can be considered as a marker of the oxidative stress, i.e., indicators of lipids peroxidation [53]. Protecting the skin with A.S.L.E before the UVA irradiation has succeeded in preventing the increase in the intensity of these peaks.
These changes are well documented for skin tissue exposed to UV radiation due to the interaction of the radiation with the cellular structure of the skin tissue [53, 54]. Also it caused numerous histopathological changes, characterized by thickening of stratum corneum (hyperkeratosis), parakeratosis, and hypertrophy of epidermal cell layer with edema in the dermis associated with few inflammatory cells infiltration and necrosis of dermal collagen in accordance with the findings of [55], excessive deposition of keratin in the epidermis and an increase in epidermal thickness for protection of the dermis from UV damage [56].
Protein electrophoresis revealed that skin samples that exposed to UV radiation had a loss in proteins corresponding to the standard regions (30–37 KDa) and (37–52 KDa) which may refer to proteins of molecular weight ~ 30 KDa, ~ 36–38 KDa, ~ 34–42 KDa”.These changes are corresponding to transforming growth factor beta, connective tissue growth factor, vascular endothelial growth factor and alpha smooth muscle actin [57] while niosomal A.S.L.E formulation may have protected those proteins during UV exposure.
The protection of the skin samples with A.S.L.E and niosomal A.S.L.E has succeeded, by different proportion, in protecting skin from the adverse and photo-damaging effects of UVA radiation. This protection could be attributed to the elevated and broad absorption of A.S.L.E to UV radiation in addition to its anti-oxidant effects [58, 59] that act as a scavenger to the ROS formed due to the interaction. The superior protection obtained by the niosomal A.S.L.E in comparison to A.S.L.E which was explored in the histopathological and protein electrophoresis investigations could be attributed to the stability offered by the nanoformulation and the sustained release of the A.S.L.E from the niosomes, which prolonged skin tissue protection. Furthermore, the free A.S.L.E may be greatly degraded as a result of its interaction with UVA under the continuous exposure. Thus, it provides lower protection to the skin tissues than the sustained niosomal A.S.L.E which provides full protection to the skin epidermal and dermal structures.
To the best of our knowledge, this is the first study that provides evidence for using niosomal-entrapped A.S.L.E as a UVA-protecting agent for the skin tissues, making this material a powerful candidate for sunscreen production. The simple method for extracting the material and the inexpensive way for the present preparation are considered as an added value to its powerful action in protecting the skin from the photo-damaging effects of UVA radiation. Furthermore, the biological origin of the A.S.L.E enhances its compatibility with biological tissues in comparison to the chemically synthesized compounds that are used as sunscreens. However, further investigations concerning the study of the molecular and cellular changes due to exposure to UV radiation and the protecting effects of niosomal A.S.L.E against these adverse effects are warranted.
References
Hanson, K. M., Gratton, E., & Bardeen, C. J. (2006). Sunscreen enhancement of UV-induced reactive oxygen species in the skin. Free Radical Biology & Medicine, 41, 1205–1212.
Rass, K., & Reichrath, J. (2008). UV damage and DNA repair in malignant melanoma and non-melanoma skin cancer. Advances in Experimental Medicine and Biology, 624, 162–178. https://doi.org/10.1007/978-0-387-77574-6_13
Reisch, M. S. (2001). Spotlight on sunscreens. Chemical & Engineering News, 79, 25–29.
Mohamad, E. A., Rageh, M. M., & Darwish, M. M. (2022). A sunscreen nanoparticles polymer based on prolonged period of protection. Journal of Bioactive and Compatible Polymers., 37(1), 17–27.
Pattanaargson, S., & Limphong, P. (2001). Stability of octyl methoxycinnamate and identification of its photo-degradation product. International Journal of Cosmetic Science, 23, 153–160.
Scalia, S., Molinari, A., Casolari, A., & Maldotti, A. (2004). Complexation of the sunscreen agent, phenyl benzimidazole sulphonic acid with cyclodextrins: Effect on stability and photo-induced free radical formation. European Journal of Pharmaceutical Sciences, 22, 241–249.
MacManus-Spencer Laura, A., Tse Monica, L., Klein Jacob, L., & Kracunas, A. E. (2011). Environmental Science & Technology, 45(9), 3931–3937.
Miura, Y., Hirao, T., & Hatao, M. (2012). Influence of application amount on sunscreen photodegradation in in vitro sun protection factor evaluation: Proposal of a skin-mimicking substrate. Photochemistry and Photobiology, 88(2), 475–482. https://doi.org/10.1111/j.1751-1097.2011.01042.x
Wakefield, G., Green, M., Lipscomb, S., & Flutter, B. (2004). Modified titanianano materials for sunscreen applications–reducing free radical generation and DNA damage. Materials Science and Technology, 20, 985–988.
Karlsson, I., Hillerstrom, L., Stenfeldt, A. L., Mårtensson, J., & Borje, A. (2009). Photodegradation of dibenzoylmethanes: Potential cause of photo contact allergy to sunscreens. Chemical Research in Toxicology, 22, 1881–1892.
Abd-Elghany, A. A., Mohamad, E. A., El-Sakhawy, M. A., Mansouri, S., Ismail, S. H., & Elneklawi, M. S. (2022). Enhancement of mechanical properties of chitosan film by doping with sage extract-loaded niosomes. Materials Research Express., 9, 035006. https://doi.org/10.1088/2053-1591/ac600a
Mohamad, E. A., Mohamed, Z. N., Hussein, M. A., & Elneklawi, M. S. (2022). GANE can improve Lung fibrosis by reducing inflammation via promoting p38MAPK/TGF-β1/NF-κB singling pathway down-regulation. ACS Omega, 7(3), 3109–3312.
Liaw, C.-C., Wu, T.-Y., Chang, F.-R., & Wu, Y.-C. (2010). Historic perspectives on annonaceous acetogenins from the chemical bench to preclinical trials. Planta Medica, 76, 1390–1404.
Yeh, S. H., Chang, F. R., Wu, Y. C., Yang, Y. L., Zhuo, S. K., & Hwang, T. L. (2005). An anti-inflammatory ent-kaurane from the stems of Annona squamosa that inhibits various human neutronphil functions. Planta Medica, 71, 904–909.
Yang, Y. L., Hua, K. F., Chuang, P. H., Wu, S. H., Wu, K. Y., Chang, F. R., & Wu, Y. C. (2007). New cyclic peptides from the seeds of Annona squamosa L. and their anti-inflammatory activities. Journal of Agricultural and Food Chemistry, 56, 386–392.
Dellai, A., Maricic, I., Kumar, V., Arutyunyan, S., & Bouraoui, A. (2010). Parallel synthesis and anti-inflammatory activity of cyclic peptides cyclosquamosin D and Metcherimolacyclo peptide B and their analogs. Bioorganic & Medicinal Chemistry Letters, 20, 5653–5657.
Chavan, M. J., Wakte, P. S., & Shinde, D. B. (2010). Analgesic and anti-inflammatory activity of Caryophyllene oxide from Annonasquamosa L. bark. Phytomedicine, 17, 149–151.
Chavan, M. J., Wakte, P. S., & Shinde, D. B. (2011). Analgesic and anti-inflammatory activities of 18-acetoxy-ent-kaur-16-ene from Annona squamosa L. bark. Inflammopharmacology, 19(2), 111–115. https://doi.org/10.1007/s10787-010-0061-5
Dang, Q. L., Kim, W. K., Nguyen, C. M., Choi, Y. H., Choi, G. J., Jang, K. S., Park, M. S., Lim, C. H., Luu, N. H., & Kim, J. C. (2011). Nematicidal and antifungal activities of Annona ceousacetogenins from Annona squamosa against various plant pathogens. Journal of Agricultural and Food Chemistry, 59, 11160–11167.
Kalidindi, N., Thimmaiah, N. V., Jagadeesh, N. V., Nandeep, R., Swetha, S., & Kalidindi, B. (2015). Antifungal and antioxidant activities of organic and aqueous extracts of Annona squamosa Linn, leaves. Journal of Food and Drug Analysis, 23, 795–802.
Dholvitayakhun, A., Trachoo, N., Sakee, U., & Cushnie, T. P. (2013). Potential applications for Annonasquamosa leaf extract in the treatment and prevention of foodborne bacterial disease. Natural Products Communications, 8, 385–388.
Padhi, L. P., Panda, S. K., Satapathy, S. N., & Dutta, S. K. (2011). In vitro evaluation of antibacterial potential of Annona squamosa L. and Annona reticulata L. from similipal biosphere reserve, Orissa, India. Journal of Agricultural Technology, 7, 133–142.
Wu, Y. C., Hung, Y. C., Chang, F. R., Cosentino, M., Wang, H. K., & Lee, K. H. (1996). Identification of ent-16 beta, 17-dihydroxykauran-19-oic acid as an anti-HIV principle and isolation of the new diterpenoids annosquamosins A and B from Annona squamosa. Journal of Natural Products, 59, 635–637.
Chen, Y., Xu, S., Chen, J. W., Wang, Y., Xu, X., Fan, N., & Li, X. (2012). Antitumor activity of Annona squamosa seeds extract containing Annona ceousacetogenin compounds. Journal of Ethnopharmacology, 142(2), 462–466.
Yang, R. M., Li, W. M., Hu, W. J., Huang, W. H., Zhu, C. Y., Yu, J. G., Zhao, X., Cai, D. Y., & Gao, N. N. (2015). Anticancer effect of total Annona ceousacetogenins on hepato carcinoma. Chinese Journal of Integrative Medicine, 21, 682–688.
Miao, Y., Xu, X., Yuan, F., Shi, Y., Chen, Y., Chen, J., & Li, X. (2016). Four cytotoxic Annona ceousacetogenins from the seeds of Annona squamosa. Natural Product Research, 30, 1273–1279.
Jagtap, U. B., & Bapat, V. A. (2012). Antioxidant activities of various solvent extracts of custard apple (Annona squamosa L.) fruit pulp. Nutrafoods, 11, 137–144.
Luzia, D. M. M., & Jorge, N. (2012). Soursop (Annona muricata L.) and sugar apple (Annona squamosa L.): Antioxidant activity, fatty acids profile and determination of tocopherols. Nutrition & Food Science, 42, 434–441.
Nandhakumar, E., & Indumathi, P. (2013). In vitro antioxidant activities of methanol and aqueous extract of Annona squamosa (.L) fruit pulp. Journal of Acupuncture and Meridian Studies, 6, 142–148.
Tu, W., Zhu, J., Hen, D., Song, L., Wang, L., Zi, J., & Yu, R. (2016). Isolation and characterization and bioactivities of a new polysaccharide from Annona squamosa and its sulfated derivative. Carbohydrate Polymer, 152, 287–296.
Anon. (1986). The useful plants of India. Publications & Information Directorate.
Seleci, M., Seleci, D. A., Joncyzk, R., Stahl, F., Blume, C., & Scheper, T. (2016). Smart multifunctional nanoparticles in nanomedicine. Bio Nano Materials, 17(1–2), 33–41.
Mahale, N. B., Thakkar, P. D., Mali, R. G., Walunj, D. R., & Chaudhari, S. R. (2012). Niosomes: Novel sustained release nonionic stable vesicular systems-an overview. Advances in Colloid and Interface Science, 183, 46–54.
Kashyap, D., Sarmah, P., Sultana, S., & Hub, I. B. (2015). Evaluation of antioxidant activity and nutraceutical property of annonasquamosa L fruits found in Brahmaputra valley agro-climatic. WJPPS, 4(5), 1151–1157.
El-Chaghaby, A., Ahmad, F., & Ramis, S. (2011). Evaluation of the antioxidant and antibacterial properties of various solvent extracts of Annona squamosal leaves. Arabian Journal of Chemistry, 7(2), 227–233.
Sathali, H., & Rajalakshmi, G. (2010). Evaluation of transdermal targeted niosomal drug delivery of terbinafine hydrochloride. International Journal of PharmTech Research, 2(3), 2081–2089.
Fahmy, H. M., Idris, A. M. R., Elsayed, A. A., & Mohamad, E. A. (2021). Electroporation-enhanced entrapment of diclofenac sodium and ascorbic acid into DPPC liposomes. Research Journal of Biotechnology, 16(11), 19–26.
Bendas, R., & Tadros, I. (2007). Enhanced transdermal delivery of Salbutamol sulfate via ethosomes. An Official Journal of the American Association of Pharmaceutical Scientists, 8(4), 213–220.
Trotta, M., Peira, E., Debernardi, F., & Gallarate, M. (2002). Elastic liposomes for skin delivery of dipotassium glycyrrhizinate. International Journal of Pharmaceutics, 241(2), 319–327.
Fočo, A., Gašperlin, M., & Kristl, J. (2005). Investigation of liposomes as carriers of sodium ascorbyl phosphate for cutaneous photoprotection. International Journal of Pharmaceutics, 291(1–2), 21–29.
Bancroft, J. D., & Stevens, A. (2010). Theory and Practice of Histology Technique Chrichil Livingston E. Edinburgh.
Rageh, M. M., El-Garhy, M. R., & Mohamad, E. A. (2020). Magnetic fields enhance the anti-tumor efficacy of low dose cisplatin and reduce the nephrotoxicity. Naunyn-Schmiedeberg’s Archives of Pharmacology (NSAP), 393(8), 1475–1485. https://doi.org/10.1007/s00210-020-01855-9
Mohamad, E. A., Elfky, A. A., El-Gebaly, R. H., & Afify, A. (2022). Study the change in the mosquito larvae (Culex pipiens) in water treated with short pulses electric filed. Electromagnetic Biology and Medicine., 41(1), 80–92.
Abd-Elghany, A. A., & Mohamad, E. A. (2021). Antitumor impact of iron oxide nanoparticles in Ehrlich carcinoma-bearing mice. Journal of Radiation Research and Applied Sciences., 14(1), 314–321.
Laemmli, U. K. (1970). Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature, 227, 680–685.
World Health Organization (WHO). Ultraviolet radiation (UV): The known health effects of UV. https://www.who.int/uv/faq/uvhealtfac/en/index1.html, June,7, 2019.
Boniol, M., Autier, P., Boyle, P., & Gandini, S. (2012). Cutaneous melanoma attributable to sunbed use: Systematic review and meta-analysis. BMJ, 345, e4757.
Rinnerthaler, M., Bischof, J., Streubel, M.K., Trost, A., Richter, K. Oxidative stress in aging human skin. Biomolecules 5(2), 545–589 (2015). Published 2015 Apr 21. doi:https://doi.org/10.3390/biom502054536. Bendas, R., Tadros, I. Enhanced transdermal delivery of Salbutamol sulfate via ethosomes. AAPS Pharm Sci Tech 8(4), 213–220 (2007).
Mohamad, E. A., Aly, A. A., Ahmed, M. I., Kamel, R. M., Abdelnaby, S. M., Abdelzaher, Y. H., & Sedrak, M. G. (2021). Evaluation of natural bioactive-derived punicalagin niosomes in skin-aging processes accelerated by oxidant and ultraviolet radiation. Drug Design, Development and Therapy, 15, 3151–3162.
Jagtap, U. B., & Bapat, V. A. (2013). Biosynthesis, characterization and antibacterial activity of silver nanoparticles by aqueous Annona squamosa L leaf extract at room temperature. Journal of Plant Biochemistry and Biotechnology, 22, 434–440.
Shakeel, F., Baboota, S., Ahuja, A., Ali, J., & Shafiq, S. (2008). Skin permeation mechanism and bioavailability enhancement of celecoxib from transdermally applied nanoemulsion. Journal of Nanobiotechnology, 6, 8. https://doi.org/10.1186/1477-3155-6-8
Mohamad, E. A., & Fahmy, H. M. (2020). Niosomes and liposomes as promising carriers for dermal delivery of Annona squamosa extract. Brazilian Journal of Pharmaceutical Sciences, 56, e18096.
Abd-Elghany Amr, A., & Mohammad, E. A. (2020). Ex-vivo transdermal delivery of annona squamosa entrapped in niosomes by electroporation. Journal of Radiation Research and Applied Sciences, 13(1), 164–173.
D’Orazio, J., Jarrett, S., Amaro-Ortiz, A., & Scott, T. (2013). UV radiation and the skin. International Journal of Molecular Sciences, 14(6), 12222–12248. https://doi.org/10.3390/ijms140612222
Yaar, M., & Gilchrest, B. A. (2007). Photoageing: Mechanism, prevention and therapy. British Journal of Dermatology, 157(5), 874–887. https://doi.org/10.1111/j.1365-2133.2007.08108.x
Kim, H. K. (2016). Garlic supplementation ameliorates UV-induced photoaging in hairless mice by regulating antioxidative activity and MMPs expression. Molecules, 21, 70. https://doi.org/10.3390/molecules21010070
Mazumdar, S., Ghosh, A. K., Dinda, M., et al. (2021). Evaluation of wound healing activity of ethanol extract of Annona reticulata L. leaf both in vitro and in diabetic mice model. Journal of Traditional and Complementary Medicine, 11(1), 27–37. https://doi.org/10.1016/j.jtcme.2019.12.001
Nguyen, M. T., Nguyen, T., Le, V. M., Trieu, L. H., Lam, T. D., Bui, L. M., Nhan, L. T. H., & Danh, V. T. (2020). Assessment of preliminary phytochemical screening, polyphenol content, flavonoid content, and antioxidant activity of custard apple leaves (Annona squamosa Linn). IOP Conference Series: Materials Science and Engineering, 2, 736.
Yaar, M., & Gilchrest, B. A. (2001). Skin aging: Postulated mechanisms and consequent changes in structure and function. Clinics in Geriatric Medicine, 17, 617–630.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
EM: methodology, investigation, writing draft preparation. KA: histophathological investigations. HM: conceptualization, methodology, writing—review and editing.
Corresponding author
Ethics declarations
Competing interest
The authors declare that there is no conflict of interest.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mohamad, E.A., Ahmed, K.A. & Mohammed, H.S. Evaluation of the skin protective effects of niosomal-entrapped annona squamosa against UVA irradiation. Photochem Photobiol Sci 21, 2231–2241 (2022). https://doi.org/10.1007/s43630-022-00291-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43630-022-00291-3