Abstract
Background
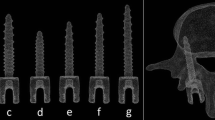
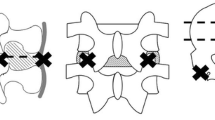
Cervical pedicle screw-rod fixation presents a complex approach in spinal surgery, offering enhanced spine stabilization in variable conditions considering traumatic injuries, degenerative changes, as well as orthopaedic and oncological ailments. This technique employs small diameter screw implants strategically placed to bolster the mechanical integrity of the spine. Notably, it involves minimally invasive procedures, resulting in smaller incisions and reduced patient discomfort. This study aims to assess the effects of trapezoidal thread screws in pedicle sections of the cervical spine during flexion-extension loadings, focusing on factors such as range of motion (ROM), implant stress, and stress on adjacent bone.
Methods
Utilizing CT scan data, a finite element model of the cervical spine (C2-C7 vertebrae) was prepared. Trapezoidal thread screws were integrated into a single-level pedicle screw-rod fixation at the C5-C6 vertebrae. The C2 vertebra were given a compressive load of 50 N along with a moment of 1 Nm, resulting in the immobilization of the C7.
Results and Discussion
The results indicate a reduction in ROM at the C5-C6 level by 69% to 77% compared to the intact spine during flexion-extension loading, with a slight increase in ROM observed at adjacent cervical spine levels. Stress analysis revealed that the trapezoidal thread screws induced stresses ranging from 24 MPa to 29 MPa in PEEK trapezoidal screw-rod implants, which fall below the material's yield stress.
Conclusions
This suggests that the trapezoidal thread profile may be advantageous in minimizing stress concentration, attributed to its larger contact area with the vertebrae bone between the threads.







Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are fully available and can be obtained from the corresponding author upon request. No external repository has been used to store the data, but comprehensive datasets can be provided following any ethical and legal guidelines upon request to the corresponding author.
References
Chen, P., Li, Z., & Hu, Y. (2016). Prevalence of osteoporosis in China: A meta-analysis and systematic review. BMC Public Health, 16, 1–11.
Yu, Y., Xie, Y., Jian, Q., Shi, Y., Zhang, G., & Fan, X. (2020). Biomechanical analysis and optimization of screw fixation technique for the cortical bone channel of lower thorax: Study protocol clinical trial (SPIRIT Compliant). Medicine, 99(7), e19046.
Weiser, L., Huber, G., Sellenschloh, K., et al. (2017). Insufficient stability of pedicle screws in osteoporotic vertebrae: Biomechanical correlation of bone mineral density and pedicle screw fixation strength. European Spine Journal, 26, 2891–2897.
Bullmann, V., Schmoelz, W., Richter, M., et al. (2010). Revision of cannulated and perforated cement-augmented pedicle screws: A biomechanical study in human cadavers. Spine, 35, E932–E939.
Kueny, R. A., Kolb, J. P., Lehmann, W., et al. (2014). Influence of the screw augmentation technique and a diameter increase on pedicle screw fixation in the osteoporotic spine: Pullout versus fatigue testing. European Spine Journal, 23, 2196–2202.
Kim, H. J., Chun, H. J., et al. (2012). The biomechanical effect of pedicle screws’ insertion angle and position on the superior adjacent segment in 1 segment lumbar fusion. Spine, 37, 1637–1644.
Sven, H., Yannick, L., Daniel, B., et al. (2014). Influence of screw augmentation in posterior dynamic and rigid stabilization systems in osteoporotic lumbar vertebrae. Spine, 39, E384–E389.
Zindrick, M. R., Wiltse, L. L., et al. (1987). Analysis of themorphometric characteristics of the thoracic and lumbar pedicles. Spine, 12, 160–166.
Da, L., Shi, L., Lei, W., et al. (2016). Biomechanical comparison of expansive pedicle screw and polymethylmethacrylate-augmented pedicle screw in osteoporotic synthetic bone in primary implantation: An experimental study. Clinical Spine Surgery, 29, E351–E357.
Ghermandi, R., Pipola, V., Colangeli, S., et al. (2018). Polymethylmethacrylate-augmented fenestrated pedicle-screw fixation in low bone quality patients: A case series and literature review. Journal of Biological Regulators and Homeostatic Agents, 12, 71–76.
Rajaee, S. S., Bae, H. W., Kanim, L. E. A., & Delamarter, R. B. (2012). Spinal fusion in the United States: Analysis of trends from 1998 to 2008. Spine, 37, 67–76.
Fior Markets. (2020). Global pedicle screw system market by product, surgery type, indication, application, region, industry analysis, size, share, growth, trends, and forecast 2018 to 2025. Fior Markets.
Pfeiffer, F. M., & Abernathie, D. L. (2006). A comparison of pullout strength for pedicle screws of different designs: A study using tapped and untapped pilot holes. Spine, 31, E867–E870.
Seichi, A., Takeshita, K., Nakajima, S., Akune, T., Kawaguchi, H., & Nakamura, K. (2005). Revision cervical spine surgery using transarticular or pedicle screws under a computer-assisted image-guidance system. Journal of Orthopaedic Science, 10, 385–390.
Addevico, F., Morandi, M., Scaglione, M., & Solitro, G. F. (2020). Screw insertion torque as parameter to judge the fixation. Assessment of torque and pull-out strength in different bone densities and screw-pitches. Clinical Biomechanics, 72, 130–213.
Amirouche, F., Solitro, G. F., & Magnan, B. P. (2016). Stability and spine pedicle screws fixation strength—A comparative study of bone density and insertion angle. Spine Deformity, 4, 261–267.
Battula, S., Schoenfeld, A. J., Sahai, V., Vrabec, G. A., Tank, J., & Njus, G. O. (2008). The effect of pilot hole size on the insertion torque and pullout strength of self-tapping cortical bone screws in osteoporotic bone. Journal of Trauma, 64, 990–995.
Kim, Y. Y., Choi, W. S., & Rhyu, K. W. (2012). Assessment of pedicle screw pullout strength based on various screw designs and bone densities—An ex vivo biomechanical study. Spine Journal, 12, 164–168.
Brasiliense, L. B., Lazaro, B. C., Reyes, P. M., Newcomb, A. G., Turner, J. L., Crandall, D. G., et al. (2013). Characteristics of immediate and fatigue strength of a dual-threaded pedicle screw in cadaveric spines. Spine Journal, 13(8), 947–956.
Wang, T., Boone, C., Behn, A. W., Ledesma, J. B., & Bishop, J. A. (2016). Cancellous screws are biomechanically superior to cortical screws in metaphyseal bone. Orthopedics, 39(5), e828–e832.
Kumar, R., & Kumar, A. (2023). Biomechanical analysis of a single-level customized cage screw fixation for anterior cervical discectomy and fusion in the cervical spine: an in-silico study. Biomedical Physics & Engineering Express., 9(4), 045018.
Kumar, R. (2023). Biomechanical analysis of two-level novel cage type implant for anterior cervical discectomy and fusion: A finite element analysis. Journal of Long-Term Effects of Medical Implants., 33(4), 43–52.
Hsieh, M. K., Li, Y. D., Liu, M. Y., Lin, C. X., Tsai, T. T., Lai, P. L., & Tai, C. L. (2021). Biomechanical comparison of fixation stability among various pedicle screw geometries: Effects of screw outer/inner projection shape and thread profile. Applied Sciences, 11(21), 9901.
Sensale, M., Vendeuvre, T., Schilling, C., Grupp, T., Rochette, M., & Dall’Ara, E. (2021). Patient-specific finite element models of posterior pedicle screw fixation: Effect of screw’s size and geometry. Frontiers in Bioengineering and Biotechnology, 9, 643154.
Liu, M. Y., Tsai, T. T., Lai, P. L., Hsieh, M. K., Chen, L. H., & Tai, C. L. (2020). Biomechanical comparison of pedicle screw fixation strength in synthetic bones: Effects of screw shape, core/thread profile and cement augmentation. PLoS ONE, 15(2), e0229328.
Liu, G., Ma, W., Xu, R., Godinsky, R., Sun, S., Feng, J., Zhao, L., Hu, Y., Zhou, L., & Liu, J. (2013). Clinical application of combined fixation in the cervical spine using posterior transfacet screws and pedicle screws. Journal of Clinical Neuroscience, 20(4), 560–564.
Aydin, A. L., Sasani, M., Erbulut, D. U., Oktenoglu, T., & Ozer, A. F. (2020). A new concept of motion preservation surgery of the cervical spine: PEEK rods for the posterior cervical region. Bio-Medical Materials and Engineering, 31(4), 235–251.
Gandhi, A. A., Grosland, N. M., Kallemeyn, N. A., Kode, S., Fredericks, D. C., & Smucker, J. D. (2019). Biomechanical analysis of the cervical spine following disc degeneration, disc fusion, and disc replacement: A finite element study. International journal of spine surgery, 13(6), 491–500.
Bhattacharya, S., Roy, S., Rana, M., Banerjee, S., Karmakar, S. K., & Biswas, J. K. (2019). Biomechanical performance of a modified design of dynamic cervical implant compared to conventional ball and socket design of an artificial intervertebral disc implant: A finite element study. Journal of Mechanics in Medicine and Biology, 19(4), 1950017.
Hua, W., Zhi, J., Ke, W., Wang, B., Yang, S., Li, L., & Yang, C. (2020). Adjacent segment biomechanical changes after one-or two-level anterior cervical discectomy and fusion using either a zero-profile device or cage plus plate: A finite element analysis. Computers in Biology and Medicine, 120, 103760.
Manickam, P. S., Ghosh, G., & Roy, S. (2022). Optimization of bone graft shapes of s-type cervical cage through genetic algorithm. International Journal for Multiscale Computational Engineering, 20(1), 55–68.
Rho, J. Y., Hobatho, M. C., & Ashman, R. B. (1995). Relations of mechanical properties to density and CT numbers in human bone. Medical Engineering & Physics, 17(5), 347–355.
Manickam, P. S., Roy, S., & Shetty, G. M. (2021). Biomechanical evaluation of a novel S-type, dynamic zero-profile cage design for anterior cervical discectomy and fusion with variations in bone graft shape: A finite element analysis. World Neurosurgy, 154, e199-214.
Biswas, J. K., Karmakar, S. K., Majumder, S., Banerjee, P. S., Saha, S., & Roychowdhury, A. (2014). Optimization of spinal implant screw for lower vertebra through finite element studies. Journal of Long-Term Effects of Medical Implants, 24(2–3), 99–108.
Panjabi, M. M., Crisco, J. J., Vasavada, A., Oda, T., Cholewicki, J., Nibu, K., & Shin, E. (2001). Mechanical properties of the human cervical spine as shown by three-dimensional load–displacement curves. Spine, 26(24), 2692–2700.
Kelly, N., & McGarry, J. P. (2012). Experimental and numerical characterisation of the elastoplastic properties of bovine trabecular bone and a trabecular bone analogue. Journal of the Mechanical Behavior of Biomedical Materials, 9, 184–197.
Katonis, P., Christoforakis, J., Aligizakis, A. C., Papadopoulos, C., Sapkas, G., & Hadjipavlou, A. (2003). Complications and problems related to pedicle screw fixation of the spine. Clinical Orthopaedics and Related Research®, 411, 86–94.
Biswas, J. K., Rana, M., Majumder, S., Karmakar, S. K., & Roychowdhury, A. (2018). Effect of two-level pedicle-screw fixation with different rod materials on lumbar spine: A finite element study. Journal of Orthopaedic Science, 23(2), 258–265.
Shi, L., Shen, K., Chu, L., Yu, K. X., Yu, Q. S., Deng, R., & Deng, Z. L. (2019). Biomechanical study of novel unilateral fixation combining unilateral pedicle and contralateral translaminar screws in the subaxial cervical spine. World Neurosurgery, 121, e684–e690.
Abumi, K., Itoh, H., Taneichi, H., & Kaneda, K. (1994). Transpedicular screw fixation for traumatic lesions of the middle and lower cervical spine: Description of the techniques and preliminary report. Clinical Spine Surgery, 7(1), 19–28.
Abumi, K., Shono, Y., Ito, M., Taneichi, H., Kotani, Y., & Kaneda, K. (2000). Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine, 25(8), 962–969.
Hilibrand, A. S., & Robbins, M. (2004). Adjacent segment degeneration and adjacent segment disease: The consequences of spinal fusion? Spine Journal, 4(6 Suppl), 190S-194S.
Ahn, Y. H., Chen, W. M., Lee, K. Y., Park, K. W., & Lee, S. J. (2008). Comparison of the load-sharing characteristics between pedicle based dynamic and rigid rod devices. Biomedical Materials, 3(4), 044101.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
For this type of study informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kumar, R., Kumar, A., Kumari, S. et al. Biomechanical Analysis of Trapezoidal Thread Screw–Rod Fixation in Pedicle Section of Cervical Spine: A Finite-Element Analysis. JOIO (2024). https://doi.org/10.1007/s43465-024-01170-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43465-024-01170-y