Abstract
Background
Drug resistant (DR) osteoarticular TB (OATB) is a challenge in view of it being deep seated lesion and paucibacillary disease. Case definition, investigation protocol, treatment of proven DR and those cases where DR could not be demonstrated lacks clarity and evidence. Hence, a series of studies were conducted to develop an algorithm to investigate and treat therapeutically refractory disease (TRD) or presumptive drug resistance (PDR) cases of OATB.
Patients and methods
6 studies were conducted. Study one and two evaluated criteria to label TRD/PDR. Three subsequent studies were conducted where TDR/PDR or fresh cases of OATB cases were investigated by AFB smear, Bactec/liquid culture, histology and genotypic DST by CBNAAT & LPA. Sixth study was a retrospective evaluation of all DR cases treated for proven or clinical drug resistance (CDR).
Results
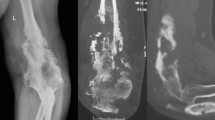
Patient of bone/spine TB on ATT for 5 months or more show poor clinico-radiological treatment response as worsening of lesion, increased spinal deformity, persistent discharging sinus/ulcer, appearance of fresh lesion, recurrence of previous lesion, wound dehiscence of post-operative surgical scar cab labelled as PDR cases. These cases on histology ascertained TB and were proven DR on genotypic and phenotypic DST and are treated successfully. The patients of histologically ascertained TB and no/indeterminate phenotypic and genotypic DST were successfully treated as clinical drug resistance on MDR protocol.
Conclusions
We described an algorithm. We must suspect PDR(TRD) based on criteria described. The tissue must be procured and submitted for AFB smear, histology and phenotypic and genotypic DST for diagnosis of TB. Genotypic and phenotypic DST will be useful to prove (90% instances) type of drug resistance. Remaining on strong clinical suspicion of DR and yet inconclusive on phenotypic/genotypic DST (<10%), may be treated as CDR as MDR. The adverse drug reactions and hepatic side-effects should be monitored diligently and these cases to be treated till healed status is demonstrated.

Similar content being viewed by others
Data availability
Not applicable.
Abbreviations
- DR-TB:
-
Drug resistant tuberculosis
- OATB:
-
Osteoarticular TB
- TRD:
-
Therapeutically refractory disease
- PDR:
-
Presumptive drug resistance
- AFB:
-
Acid fast bacilli
- CBNAAT:
-
Cartridge based nucleic acid amplification test
- LPA:
-
Line Probe Assay
- CDR:
-
Clinical drug resistance
- DST:
-
Drug susceptibility testing
- MDR:
-
Multi drug resistance
- RR:
-
Rifampicin resistance
- XDR:
-
Extensively drug resistant
- TB/STB:
-
Tuberculosis/spinal tuberculosis
- PCR:
-
Polymerase chain reaction
- INH:
-
Isoniazid
- RIF:
-
Rifampicin
- KAN:
-
Kanamicin
- AMK:
-
Amikacin
- CAP:
-
Capreomycin
- ETH:
-
Ethionamide
- LEV:
-
Levaflox
- Mox:
-
Moxiflox
- LNZ:
-
Linezolid
- PAS:
-
Para amino salicylic acid
- BDQ:
-
Bedaquiline
- DLM:
-
Delamanid
- CFO:
-
Clofazimin
References
Global tuberculosis report 2020. Retrieved October 20, 2020, from https://www.who.int/publications/i/item/global-tuberculosis-report-2020
Tiemersma, E. W., van der Werf, M. J., Borgdorff, M. W., Williams, B. G., & Nagelkerke, N. J. D. (2011). Natural history of tuberculosis: Duration and fatality of untreated pulmonary tuberculosis in HIV negative patients: A systematic review. PLoS ONE, 6(4), e17601.
Jain, A. K. (2010). Tuberculosis of the spine: A fresh look at an old disease. Journal of Bone and Joint Surgery. British Volume, 92(7), 905–913.
Keshavjee, S., & Farmer, P. E. (2012). Tuberculosis, drug resistance, and the history of modern medicine. New England Journal of Medicine, 367(10), 931–936.
Crofton, J., & Mitchison, D. A. (1948). Streptomycin resistance in pulmonary tuberculosis. British Medical Journal, 2(4588), 1009–1015.
Global tuberculosis report 2023. Retrieved January 28, 2024, from https://www.who.int/publications-detail-redirect/9789240083851
WHO Operational Handbook on Tuberculosis, Module 4: Treatment—Drug-Resistant Tuberculosis Treatment. Retrieved April 16, 2022, from https://www.who.int/publications-detail-redirect/9789240006997
India TB Report 2023, Ministry of Health & Family Welfare-Government of India Retrieved January 29, 2024, from https://tbcindia.gov.in/showfile.php?lid=3680
Mishra, G., & Mulani, J. (2018). First National Anti-Tuberculosis Drug Resistance Survey (NDRS) from India—an eye opener. Journal of Infectiology and Epidemiology, 1, 26–29.
Tuli, S. M. (2002). General principles of osteoarticular tuberculosis. Clinical Orthopaedics, 398, 11–19.
Jain, A. K., Jaggi, K. R., Bhayana, H., & Saha, R. (2018). Drug-resistant spinal tuberculosis. Indian Journal of Orthopaedics, 52(2), 100–107.
Lee, J. Y. (2015). Diagnosis and treatment of extrapulmonary tuberculosis. Tuberculosis and Respiratory Diseases, 78(2), 47–55.
Jain, A. K., Rajasekaran, S., Jaggi, K. R., & Myneedu, V. P. (2020). Tuberculosis of the spine. Journal of Bone and Joint Surgery, 102(7), 617–628.
Jain, A., Dhammi, I., Modi, P., Kumar, J., Sreenivasan, R., & Saini, N. (2012). Tuberculosis spine: Therapeutically refractory disease. Indian Journal of Orthopaedics, 46(2), 171–178.
Jaggi, K. R. J. A. (2006). Diagnosis and therapeutic outcome of suspected multidrug resistant cases of spinal tuberculosis on second line anti tubercular therapy. University of Delhi.
Abhimanyu, S., Jain, A. K., Myneedu, V. P., Arora, V. K., Chadha, M., & Sarin, R. (2021). The role of cartridge-based nucleic acid amplification test (CBNAAT), line probe assay (LPA), liquid culture, acid-fast bacilli (AFB) smear and histopathology in the diagnosis of osteoarticular tuberculosis. Indian Journal of Orthopaedics, 55(Suppl 1), 157–166.
Yadav, M., Jain, A. K., Singhal, R., Chadha, M., Arora, V. K., & Bhargava, A. (2023). Incidence and patterns of drug resistance in patients with spinal tuberculosis: A prospective, single-center study from a tuberculosis-endemic country. Indian Journal of Orthopaedics, 57(11), 1833–1841.
Gain, A., Jain, A. K., Bhalla, M., Aggarwal, A. N., Dhammi, I. K., Arora, V. K., et al. (2023). Drug resistance in osteoarticular tuberculosis: A study from an endemic zone. Cureus. https://doi.org/10.7759/cureus.44173
Gupta, H., Jain, A. K. et al. Treatment outcomes of drug resistant skeletal tuberculosis : A retrospective analysis. Indian Journal of Orthopaedics (Accepted for publication)
Arora, A., Nadkarni, B., Dev, G., Chattopadhya, D., Jain, A. K., Tuli, S. M., et al. (2006). The use of immunomodulators as an adjunct to antituberculous chemotherapy in non-responsive patients with osteo-articular tuberculosis. The Journal of Bone and Joint Surgery. British Volume, 88-B(2), 264–269.
Ogwang, S., Mubiri, P., Bark, C. M., Joloba, M. L., Boom, W. H., & Johnson, J. L. (2015). Incubation time of Mycobacterium tuberculosis complex sputum cultures in BACTEC MGIT 960: Four weeks of negative culture is enough for physicians to consider alternative diagnoses. Diagnostic Microbiology and Infectious Disease, 83(2), 162–164.
Tuli, S. (2002). Challenge of therapeutically refractory and multidrug resistant tuberculosis in orthopaedic practice. Indian Journal of Orthopaedics, 36(4), 211–213.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Standard Statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed Consent
For this type of study informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This Paper was delivered as “Golden Jubilee Oration” at 60th Annual Conference of Indian Orthopaedic Association, 14–17 Dec 2023 at Lucknow.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jain, A.K., Jain, P., Jaggi, K. et al. Drug-Resistant Bone, Joint and Spine Tuberculosis: Evolution of Diagnosis and Treatment. JOIO 58, 661–668 (2024). https://doi.org/10.1007/s43465-024-01138-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-024-01138-y