Abstract
Background
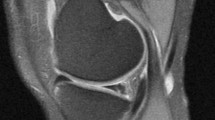
Considering various factors that influence meniscal repairability, Ortho One PROMT score (OPS) was proposed in 2019. With an increased understanding of factors influencing meniscal repair and by analysis of OPS predictions and repair results, a modified PROMT score (MPS) has been formulated. The objective of this study is to assess the superiority of MPS over OPS.
Methods
Age, chronicity, and pattern of tears were found to be important contributors to false-negative results of OPS. Considering these factors, MPS was designed. A prospective, double-blinded study was conducted between November 2020 and May 2021. Sensitivity, specificity, positive likelihood ratio, negative likelihood ratio, positive predictive value, negative predictive value, and accuracy of both scores were calculated. Receiver Operating Characteristic (ROC) curve was plotted.
Results
Of 133 meniscal tears, 100 met the inclusion criteria. In predicting meniscal repairability, OPS demonstrated sensitivity and specificity of 90.32% and 83.33% medially and 64.71% and 79.41% laterally. MPS had sensitivity and specificity of 96.77% and 88.89% medially and 82.35% and 88.24% laterally. Both scores showed good statistical significance (p < 0.05) in predicting meniscal reparability. For medial meniscus repairability, area under the ROC curve was 0.868 for OPS and 0.928 for MPS. For lateral repairability, the area under the curve was 0.721 for OPS and 0.853 for MPS.
Conclusion
MPS will serve as a simple and more effective tool for surgeons to predict meniscal repairability, thus enhancing their pre-surgical preparedness. This tool will also help surgeons to realistically counsel their patients and to achieve optimal patient.



Similar content being viewed by others
Availability of data and material
Available upon request.
References
Makris, E. A., Hadidi, P., & Athanasiou, K. A. (2011). The knee meniscus: Structure-function, pathophysiology, current repair techniques, and prospects for regeneration. Biomaterials, 32, 7411–7431. https://doi.org/10.1016/j.biomaterials.2011.06.037
Kopf, S., Beaufils, P., Hirschmann, M. T., Rotigliano, N., Ollivier, M., Pereira, H., et al. (2020). Management of traumatic meniscus tears: The 2019 ESSKA meniscus consensus. Knee Surgery, Sports Traumatology, Arthroscopy, 28, 1177–1194. https://doi.org/10.1007/s00167-020-05847-3
Paxton, E. S., Stock, M. V., & Brophy, R. H. (2011). Meniscal repair versus partial meniscectomy: A systematic review comparing reoperation rates and clinical outcomes. Arthroscopy, 27, 1275–1288. https://doi.org/10.1016/j.arthro.2011.03.088
Stein, T., Mehling, A. P., Welsch, F., von Eisenhart-Rothe, R., & Jäger, A. (2010). Long-term outcome after arthroscopic meniscal repair versus arthroscopic partial meniscectomy for traumatic meniscal tears. American Journal of Sports Medicine, 38, 1542–1548. https://doi.org/10.1177/0363546510364052
Rogers, M., Dart, S., Odum, S., & Fleischli, J. (2019). A cost-effectiveness analysis of isolated meniscal repair versus partial meniscectomy for red-red zone, vertical meniscal tears in the young adult. Arthroscopy, 35, 3280–3286. https://doi.org/10.1016/j.arthro.2019.06.026
Svantesson, E., Cristiani, R., HamrinSenorski, E., Forssblad, M., Samuelsson, K., & Stålman, A. (2018). Meniscal repair results in inferior short-term outcomes compared with meniscal resection: A cohort study of 6398 patients with primary anterior cruciate ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy, 26, 2251–2258. https://doi.org/10.1007/s00167-017-4793-2
Matava, M. J., Eck, K., Totty, W., Wright, R. W., & Shively, R. A. (1999). Magnetic resonance imaging as a tool to predict meniscal reparability. American Journal of Sports Medicine, 27, 436–443. https://doi.org/10.1177/03635465990270040601
Van Dyck, P., Vanhoenacker, F. M., Lambrecht, V., Wouters, K., Gielen, J. L., Dossche, L., et al. (2013). Prospective comparison of 1.5 and 3.0-T MRI for evaluating the knee menisci and ACL. Journal of Bone and Joint Surgery, 95, 916–924. https://doi.org/10.2106/JBJS.L.01195
Kumaraswamy, V., Ramaswamy, A. G., Sundar, S., Rajan, D. V., Selvaraj, K., Sahanand, S., et al. (2019). A new scoring system for prediction of meniscal repair in traumatic meniscal tears. Knee Surgery, Sports Traumatology, Arthroscopy, 27, 3454–3460. https://doi.org/10.1007/s00167-019-05377-7
Cristiani, R., Rönnblad, E., Engström, B., Forssblad, M., & Stålman, A. (2018). Medial meniscus resection increases and medial meniscus repair preserves anterior knee laxity: a cohort study of 4497 patients with primary anterior cruciate ligament reconstruction. American Journal of Sports Medicine, 46, 357–362. https://doi.org/10.1177/0363546517737054
Becker, R., & Awiszus, F. (2001). Physiological alterations of maximal voluntary quadriceps activation by changes of knee joint angle. Muscle and Nerve, 24, 667–672. https://doi.org/10.1002/mus.1053
Bernthal, N. M., Seeger, L. L., Motamedi, K., Stavrakis, A. I., Kremen, T. J., McAllister, D. R., et al. (2011). Can the reparability of meniscal tears be predicted with magnetic resonance imaging? American Journal of Sports Medicine, 39, 506–510. https://doi.org/10.1177/0363546510387507
Pujol, N., Tardy, N., Boisrenoult, P., & Beaufils, P. (2013). Magnetic Resonance Imaging is not suitable for interpretation of meniscal status ten years after arthroscopic repair. International Orthopaedics, 37, 2371–2376. https://doi.org/10.1007/s00264-013-2039-6
Orlando Júnior, N., de Souza Leão, M. G., & de Oliveira, N. H. C. (2015). Diagnosis of knee injuries: Comparison of the physical examination and magnetic resonance imaging with the findings from arthroscopy. Rev Bras Ortop, 50, 712–719. https://doi.org/10.1016/j.rboe.2015.10.007
Misir, A., Kizkapan, T. B., Yildiz, K. I., Arikan, Y., Ozcafer, R., & Cetinkaya, E. (2019). Using only MRI is moderately reliable in the prediction of meniscal tear reparability. Knee Surgery, Sports Traumatology, Arthroscopy, 27, 898–904. https://doi.org/10.1007/s00167-018-5187-9
Eggli, S., Wegmüller, H., Kosina, J., Huckell, C., & Jakob, R. P. (1995). Long-term results of arthroscopic meniscal repair. An analysis of isolated tears. American Journal of Sports Medicine, 23, 715–720. https://doi.org/10.1177/036354659502300614
Rothermel, S. D., Smuin, D., & Dhawan, A. (2018). Are outcomes after meniscal repair age dependent? A Systematic Review. Arthroscopy, 34, 979–987. https://doi.org/10.1016/j.arthro.2017.08.287
Everhart, J. S., Higgins, J. D., Poland, S. G., Abouljoud, M. M., & Flanigan, D. C. (2018). Meniscal repair in patients age 40 years and older: A systematic review of 11 studies and 148 patients. The Knee, 25, 1142–1150. https://doi.org/10.1016/j.knee.2018.09.009
Barrett, G. R., Field, M. H., Treacy, S. H., & Ruff, C. G. (1998). Clinical results of meniscus repair in patients 40 years and older. Arthroscopy, 14, 824–829. https://doi.org/10.1016/s0749-8063(98)70018-0
Michel, P. A., Domnick, C. J., Raschke, M. J., Hoffmann, A., Kittl, C., Herbst, E., et al. (2021). Age-related changes in the microvascular density of the human meniscus. American Journal of Sports Medicine, 49, 3544–3550. https://doi.org/10.1177/03635465211039865
Petersen, W., & Tillmann, B. (1995). Age-related blood and lymph supply of the knee menisci. A cadaver study. Acta Orthopaedica Scandinavica, 66, 308–312. https://doi.org/10.3109/17453679508995550
Metcalf, M. H., & Barrett, G. R. (2004). Prospective evaluation of 1485 meniscal tear patterns in patients with stable knees. American Journal of Sports Medicine, 32, 675–680. https://doi.org/10.1177/0095399703258743
Shelbourne, K. D., & Carr, D. R. (2003). Meniscal repair compared with meniscectomy for bucket-handle medial meniscal tears in anterior cruciate ligament-reconstructed knees. American Journal of Sports Medicine, 31, 718–723. https://doi.org/10.1177/03635465030310051401
Espejo-Reina, A., Serrano-Fernández, J. M., Martín-Castilla, B., Estades-Rubio, F. J., Briggs, K. K., & Espejo-Baena, A. (2014). Outcomes after repair of chronic bucket-handle tears of medial meniscus. Arthroscopy, 30, 492–496. https://doi.org/10.1016/j.arthro.2013.12.020
Cetinkaya, E., Gursu, S., Gul, M., Aykut, U. S., & Ozcafer, R. (2018). Surgical repair of neglected bucket-handle meniscal tears displaced into the intercondylar notch: Clinical and radiological results. The Journal of Knee Surgery, 31, 514–519. https://doi.org/10.1055/s-0037-1604146
Beatrice Tan, J.-N., & James Loh, S.-Y. (2021). An approach to chronic and displaced bucket handle meniscal tear—assessment, repair (push-and-pull technique), or salvage. Arthroscopy Techniques, 10, e1853–e1857. https://doi.org/10.1016/j.eats.2021.04.005
Yik, J. H., Koh, B. T. H., & Wang, W. (2017). A novel technique for modified all-inside repair of bucket-handle meniscus tears using standard arthroscopic portals. Journal of Orthopaedic Surgery and Research, 12, 188. https://doi.org/10.1186/s13018-017-0692-y
Yuen, W. L. P., Kuo, C. L., Goh, K. M. J., & Lee, Y. H. D. (2021). Technique for all-inside repair of bucket-handle meniscus tears. Arthroscopy Techniques, 10, e743–e750. https://doi.org/10.1016/j.eats.2020.10.063
Moatshe, G., Cinque, M. E., Godin, J. A., Vap, A. R., Chahla, J., & LaPrade, R. F. (2017). Comparable outcomes after bucket-handle meniscal repair and vertical meniscal repair can be achieved at a minimum 2 years’ follow-up. American Journal of Sports Medicine, 45, 3104–3110. https://doi.org/10.1177/0363546517719244
Tengrootenhuysen, M., Meermans, G., Pittoors, K., van Riet, R., & Victor, J. (2011). Long-term outcome after meniscal repair. Knee Surgery, Sports Traumatology, Arthroscopy, 19, 236–241. https://doi.org/10.1007/s00167-010-1286-y
Popescu, D., Sastre, S., Caballero, M., Lee, J. W. K., Claret, I., Nuñez, M., et al. (2010). Meniscal repair using the FasT-Fix device in patients with chronic meniscal lesions. Knee Surgery, Sports Traumatology, Arthroscopy, 18, 546–550. https://doi.org/10.1007/s00167-009-0926-6
Funding
No external funding was received for study.
Author information
Authors and Affiliations
Contributions
SS, PP—conceptualization, data curation, formal analysis, investigations, methodology, administration, resources, supervision, validation, visualization, writing original drafts and reviewing drafts. GC, PC—conceptualization, data curation, formal analysis, investigations, methodology, supervision, validation, visualization, writing original drafts and reviewing drafts. VK, SS, DVR—conceptualization, data curation, formal analysis, investigations, methodology, administration, resources, supervision, validation, and visualization.
Corresponding author
Ethics declarations
Ethics approval
Obtained from institutional ethics committee.
Consent for participation
Obtained.
Consent for publication
Obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sundar, S., Pandian, P., Chellamuthu, G. et al. The Modified PROMT Score: A Better Prognosticative Tool to Assess Traumatic Meniscal Tear Reparability. JOIO 57, 495–504 (2023). https://doi.org/10.1007/s43465-023-00838-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-023-00838-1