Abstract
Study Design
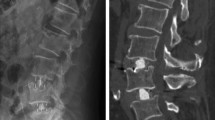
Finite element models of the L3-S1 vertebrae were reconstructed using computed tomography scans.
Objective
We compared the biomechanical performances of an oblique lateral interbody fusion (OLIF) cage in different bone density mode.
Summary of Background Data
Low bone density is an els.key factor limiting the use of stand-alone OLIF cage.
Methods
Four models—intact (M0), normal bone density with OLIF (M1), bone mass loss with OLIF (M2), and osteoporotic with OLIF (M3)—were created based on 3-dimensional scans. Flexion, extension, and lateral bending movements (each lasting 10 N·m) were performed on the superior surface of the L3 vertebra with a compressive preload of 500 N. Range of motion (ROM), peak stresses in the L4-5 cortical endplates, cage stress, and adjacent intervertebral disk stress were evaluated.
Results
ROMs during different physiological movements were similar to those reported by previous researchers. Compared with that in M0, L4-5 ROMs of all movements decreased in M1, M2 and M3, most evidently in M3. Stress distribution in the cortical endplates rose to 7.8% in M1 and M2, even 16.2% in M3. Cage stress increased by less than 8.1% in M1 and M2, but by 25.3% in M3, especially in the movements of extension and right rotation. Compared with that in M0, L3-4 and L5-S1 intervertebral disk stress increased with bone density in all the other models, by up to 69.8% and 98.3%, respectively. As osteoporosis worsened, stress in the adjacent intervertebral disk also increased.
Conclusion
Stand-alone OLIF in M3 is not recommended because of the risk of cage subsidence. OLIF in M1 and M2 achieved similar results in various lumbar spine movements. In M1 and M2 model (T > − 2.5), the L4–L5 showed reduced mobility in all directions, increased rigidity, limited cage displacement, lessened deformation, and better stability.







Similar content being viewed by others
References
Mobbs, R. J., Phan, K., Malham, G., et al. (2015). Lumbar interbody fusion: Techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF[J]. J Spine Surg., 1(1), 2–18.
Ohtori, S., Orita, S., Yamauchi, K., et al. (2015). Mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for lumbar spinal degeneration disease[J]. Yonsei Medical Journal, 56(4), 1051–1059.
Castellvi, A. E., Nienke, T. W., Marulanda, G. A., et al. (2014). Indirect decompression of lumbar stenosis with transpsoas interbody cages and percutaneous posterior instrumentation[J]. Clin Orthop Related Res., 472(6), 1784–1791.
Fujibayashi, S., Hynes, R. A., Otsuki, B., et al. (2015). Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease[J]. Spine, 40(3), 175–182.
Lykissas, M. G., Aichmair, A., Hughes, A. P., et al. (2014). Nerve injury after lateral lumbar interbody fusion: a review of 919 treated levels with identification of risk factors[J]. Spine J., 14(5), 749–758.
Silvestre, C., Mac-Thiong, J. M., Hilmi, R., et al. (2012). Complications and morbidities of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lumbar interbody fusion in 179 patients[J]. Asian Spine J., 6(2), 89–97.
Marchi, L., Abdala, N., Oliveira, L., Amaral, R., Coutinho, E., & Pimenta, L. (2013). Radiographic and clinical evaluation of cage subsidence after standalone lateral interbody fusion[J]. Clinical article J Neurosurg-Spine., 19, 110–118.
Liu, J., & Feng, H. (2020). Oblique Lateral Interbody Fusion (OLIF) with supplemental anterolateral screw and rod instrumentation: a preliminary clinical study. World Neurosurg., 134, e944–e950.
Feng, S., Tian, W., & Wei, Y. (2020). Clinical effects of oblique lateral interbody fusion by conventional open versus percutaneous robot-assisted minimally invasive pedicle screw placement in elderly patients. Orthopaedic Surg, 12(1), 86–93.
Lee, K. Y., Lee, J. H., Kang, K. C., et al. (2020). Minimally invasive multilevel lateral lumbar interbody fusion with posterior column osteotomy compared with pedicle subtraction osteotomy for adult spinal deformity. Spine J., 20(6), 925–933.
Agarwal, N., Faramand, A., Alan, N., et al. (2018). Lateral lumbar interbody fusion in the elderly: a 10-year experience: Presented at the 2018 AANS/CNS Joint section on disorders of the spine and peripheral nerves[J]. J Neurosurgery., 29(5), 525–529.
Yuan, W., Kaliya-Perumal, A. K., Chou, S. M., et al. (2020). Does lumbar interbody cage size influence subsidence? a biomechanical study[J]. Spine, 45(2), 88–95.
Bereczki, F., Turbucz, M., Kiss, R., et al. (2021). Stability evaluation of different oblique lumbar interbody fusion constructs in normal and osteoporotic condition - a finite element based study[J]. Front Bioeng Biotechnol., 9, 749914.
Zhao, X., Du, L., Xie, Y., & Zhao, J. (2018). Effect of lumbar lordosis on the adjacent segment in transforaminal lumbar interbody fusion: a finite element analysis. World Neurosurg., 114, e114–e120.
Ling, Q., He, E., Zhang, H., Lin, H., & Huang, W. (2019). A novel narrow surface cage for full endoscopic oblique lateral lumbar interbody fusion: A finite element study. J Orthopaed Sci, 24(6), 991–998.
Lu, T., & Lu, Y. (2019). Comparison of biomechanical performance among posterolateral fusion and transforaminal, extreme, and oblique lumbar interbody fusion: a finite element analysis[J]. World Neurosurg., 129, e890–e899.
Rohlmann, A., Bauer, L., Zander, T., Bergmann, G., & Wilke, H. J. (2006). Determination of trunk muscle forces for flflexion and extension by using a validated fifinite element model of the lumbar spine and measured in vivo data. Journal of Biomechanics, 39(6), 981–989.
Polikeit, A., Nolte, L. P., & Ferguson, S. J. (2003). The effect of cement augmentation on the load transfer in an osteoporotic functional spinal unit: finite-element analysis[J]. Spine, 28(10), 991–996.
Yamamoto, I., Panjabi, M. M., Crisco, T., & Oxland, T. (1989). Three-dimensional movements of the whole lumbar spine and lumbosacral joint. Spine, 14(11), 1256–1260.
Xiao, Z., Wang, L., Gong, H., et al. (2012). Biomechanical evaluation of three surgical scenarios of posterior lumbar interbody fusion by finite element analysis. Biomedical Engineering Online, 11, 1.
Grimm, B. D., Leas, D. P., Poletti, S. C., et al. (2016). Postoperative complications within the first year after extreme lateral interbody fusion: experience of the first 108 patients[J]. Clin Spine Surg., 29(3), E151–E156.
Pimenta, L., Marchi, L., Oliveira, L., Coutinho, E., & Amaral, R. (2013). A prospective, randomized, controlled trial comparing radiographic and clinical outcomes between stand-alone lateral interbody lumbar fusion with either silicate calcium phosphate or rh-BMP2. J Neurol Surg A Cent Eur Neurosurg., 74, 343–350.
Hresko, M. T., Labelle, H., Roussouly, P., & Berthonnaud, E. (2007). Classification of high-grade spondylolistheses based on pelvic version and spine balance: possible rationale for reduction. Spine, 32(20), 2208–2213.
Huo, Y., Yang, D., Ma, L., et al. (2020). Oblique lumbar interbody fusion with stand-alone cages for the treatment of degenerative lumbar spondylolisthesis: a retrospective study with 1-year follow-Up[J]. Pain Research & Management, 2020, 1–6.
Youssef, J. A., McAfee, P. C., Patty, C. A., et al. (2010). Minimally invasive surgery: lateral approach interbody fusion: results and review[J]. Spine, 35(26S), S302–S311.
Zhang, C., Wang, K., Jian, F., et al. (2018). Efficacy of oblique lateral interbody fusion in treatment of degenerative lumbar disease[J]. World neurosurg., 124, 17–24.
Schiffman, M., Brau, S. A., Henderson, R., et al. (2003). Bilateral implantation of low-profile interbody fusion cages: subsidence, lordosis, and fusion analysis[J]. Spine J., 3(5), 377–387.
Ahmadian, A., Bach, K., Bolinger, B., et al. (2015). Stand-alone minimally invasive laterallumbar interbody fusion: multicenter clinical outcomes[J]. J Clinical Neurosci., 22(4), 740–746.
Zeng, Z., Xu, Z., He, D., et al. (2018). Complications and prevention strategies of oblique lateral interbody fusion technique[J]. Orthopaedic Surgery, 10(2), 98–106.
Guo, H. Z., Tang, Y. C., Guo, D. Q., et al. (2020). Stability evaluation of oblique lumbar interbody fusion constructs with various fixation options: a finite element analysis based on three-dimensional scanning models. World Neurosurg., 138, e530–e538.
Wang, B., Hua, W., Ke, W., et al. (2019). Biomechanical evaluation of transforaminal lumbar interbody fusion and oblique lumbar interbody fusion on the adjacent segment: a finite element analysis. World Neurosurg., 126, e819–e824.
Song, C., Chang, H., Zhang, D., et al. (2021). Biomechanical evaluation of oblique lumbar interbody fusion with various fixation options: a finite element analysis[J]. Orthopaedic Surgery, 13(2), 517–529.
Du, C. F., Cai, X. Y., Gui, W., et al. (2021). Does oblique lumbar interbody fusion promote adjacent degeneration in degenerative disc disease: A finite element analysis[J]. Comp Biol Med, 128, 104122.
Ling, Q., Zhang, H., & He, E. (2021). Screws fixation for oblique lateral lumbar interbody fusion (ol-lif): a finite element study[J]. BioMed Res Inter, 2021, 5542595.
Choy, W., Mayer, R. R., Mummaneni, P. V., et al. (2020). Oblique lumbar interbody fusion with stereotactic navigation: technical note[J]. Global Spine J., 10(2 Suppl), 94S-100S.
Tohmeh, A. G., Khorsand, D., Watson, B., & Zielinski, X. (2014). Radiographical and clinical evaluation of extreme lateral interbody fusion: effects of cage size and instrumentation type with a minimum of 1-year follow-up. Spine, 39(26), 1582–1591.
Fang, G., Lin, Y., Wu, J., Cui, W., Zhang, S., Guo, L., Sang, H., & Huang, W. (2020). Biomechanical comparison of stand-alone and bilateral pedicle screw fixation for oblique lumbar interbody fusion surgery-a finite element analysis. World Neurosurg., 141, e204–e212.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
For this type of study informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xue, S., Wu, T. Biomechanical Performances of an Oblique Lateral Interbody Fusion Cage in Models with Different Bone Densities: A Finite Element Analysis. JOIO 57, 86–95 (2023). https://doi.org/10.1007/s43465-022-00775-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-022-00775-5