Abstract
Purpose
The purpose of the study was to find the effectiveness of Extended Infection Control Measures (EICM) in reducing the rate of methicillin-resistant Staphylococcus aureus (MRSA) infection among orthopaedic surgery patients.
Methods
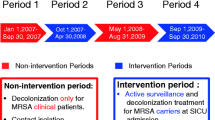
The study adopted a quasi-experimental design and was conducted in the orthopaedic units of a tertiary care hospital. This study recruited 168 orthopaedic patients and 154 healthcare professionals (HCPs). EICM included hand hygiene, decolonizing the patients and HCPS, staff education, feedback of surveillance data, treatment of high-risk and MRSA-infected patients, having separate equipment for MRSA-infected patients, and appropriate cleaning of patient’s unit.
Results
The EICM effectively reduced MRSA infection from 21.2 to 6% (p < 0.001). It also resulted in improving the knowledge of HCPs in the prevention and management of MRSA infection (p < 0.001), and all colonized HCPs were successfully (100%) decolonized.
Conclusion
EICM is a promising intervention to combat MRSA infection among orthopaedic wards. Hence, it can be executed in orthopaedic wards, thereby improving the treatment quality and reducing the infection-related consequences.


Similar content being viewed by others
Data Availability
Data are available.
Code Availability
Not applicable.
References
Word Health Organisation (2014) Antimicrobial resistance: global report on surveillance. World Health Organization. https://apps.who.int/iris/bitstream/handle/10665/112642/9789241564748_eng.pdf Accessed 26 Feb 2020
Word Health Organisation (2020) Key facts. Antimicrobial resistance. https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance Accessed 21 Mar 2021
Norris, G. R., Checketts, J. X., Scott, J. T., Vassar, M., Norris, B. L., & Giannoudis, P. V. (2019). Prevalence of deep surgical site infection after repair of periarticular knee fractures a systematic review and meta-analysis. JAMA Network Open, 2(8), 1–17. https://doi.org/10.1001/jamanetworkopen.2019.9951
Fahad, A.A.-M., Mohammed, A. B., Mir, S.-A., Abdallah, S. A., & Azam, M. Q. (2014). Prevalence of surgical site infection in orthopedic surgery: A 5-year analysis. International Surgery, 99(3), 264–268. https://doi.org/10.9738/INTSURG-D-13-00251
Latha, T., Anil, B., Manjunatha, H., Chiranjay, M., Elsa, D., Baby, N., et al. (2019). MRSA: The leading pathogen of orthopaedic infection in a tertiary care hospital, South India. African Health Sciences, 19(1), 1393–1401. https://doi.org/10.4314/ahs.v19i1.12
Oliveira, P. R., Carvalho, V. C., Paula, A. P. De, Santos-silva, J., Lucia, A., Munhoz, L. (2016) The incidence and microbiological profile of surgical site infections following internal fixation of closed and open fractures. Rev Bras Ortop 51(4):5–9. https://www.scielo.br/j/rbort/a/XwDQ99CGdTy6XcJKYnq3ZVc/abstract/?lang=en
De, A. G., Mutters, T. N., Minkley, L., Holderried, F., & Tacconelli, E. (2015). Prosthetic joint infections in the elderly. Infection, 43(6), 629–637. https://doi.org/10.1007/s15010-015-0806-6
Prabhoo, R., Chaddha, R., Iyer, R., Mehra, A., Ahdal, J., & Jain, R. (2019). Overview of methicillin-resistant Staphylococcus aureus mediated bone and joint infections in India. Orthopedic Reviews (Pavia), 11, 79–84. https://doi.org/10.4081/or.2019.8070
Silago, V., Mushi, M. F., Remi, B. A., Mwayi, A., Swetala, S., Mtemisika, C. I., et al. (2020). Methicillin-resistant Staphylococcus aureus causing osteomyelitis in a tertiary hospital, Mwanza, Tanzania. Journal of Orthopaedic Surgery and Research, 5(95), 1–6. https://doi.org/10.1186/s13018-020-01618-5
Graham, G. S. (2014). Healing outcomes of MRSA-infected wounds with a protocol combining Oakin dressing with elements of de-escalation theory objective: Method: Results: Conclusion: Declaration of interest. Journal of Wound Care, 23(Sup2a), 4–7. https://doi.org/10.12968/jowc.2014.23.Sup2a.S4
Badia, J. M., Casey, A. L., Petrosillo, N., Hudson, P. M., Mitchell, S. A., & Crosby, C. (2017). Impact of surgical site infection on healthcare costs and patient outcomes: A systematic review in six European countries. Journal of Hospital Infection, 96(1), 1–15. https://doi.org/10.1016/j.jhin.2017.03.004
Sartelli, M., Mckimm, J., & Bakar, M. A. (2018). Healthcare-associated infections–an overview. Infect Drug Resist., 11, 2321–2333.
Fukuda, H., Sato, D., Iwamoto, T., Yamada, K., & Matsushita, K. (2020). Healthcare resources attributable to methicillin-resistant Staphylococcus aureus orthopaedic surgical site infections. Science and Reports, 10, 17059. https://doi.org/10.1038/s41598-020-74070-4
Loveday, H. P., Pellowe, C. M., Jones, S. R. L. J., & Pratt, R. J. (2006). A systematic review of the evidence for interventions for the prevention and control of methicillin-resistant Staphylococcus aureus (1996–2004): Report to the joint MRSA working party (subgroup A). Journal of Hospital Infection, 635, 545–570. https://doi.org/10.1016/j.jhin.2006.01.002
Yamada, K., Abe, H., Higashikawa, A., Tonosu, J., Kuniya, T., Nakajima, K., et al. (2018). Evidence-based care bundles for preventing surgical site infections in spinal instrumentation surgery. Spine (Phila Pa 1976), 43(24), 1765–1773. https://doi.org/10.1097/BRS.0000000000002709
World Health Organisation (2009) Hand Hygiene: Why, How & Wehn? World health & population. https://www.who.int/gpsc/5may/Hand_Hygiene_Why_How_and_When_Brochure.pdf
Romney, M. H., Jane, A., Stephanie, L. M., Mariana, C., Tanis, D., Janet, A. H., et al. (2018). CLSI methods development and standardization working susceptibility tests. Journal of Clinical Microbiology, 56(4), e01934-e2017. https://doi.org/10.1128/JCM.01934-17.01934-17
Sun, Y., Wang, H., Tang, Y., Zhao, H., Qin, S., Xu, L., et al. (2018). Incidence and risk factors for surgical site infection after open reduction and internal fixation of ankle fracture: A retrospective multicenter study (Cdc). Medicine. https://doi.org/10.1097/MD.0000000000009901
Jain, B., Banerjee, M. (2013) Surgical site infections and its risk factors in orthopaedics: a prospective study in teaching hospital of central India. Int J Res Med Sci 2(1):110–3. http://www.ijorim.com/siteadmin/article_issue/1368097582Ijorim24.pdf Accessed 21 Mar 2020
Lee, A. S., Cooper, B. S., Malhotra-kumar, S., Chalfine, A., Daikos, G. L., Fankhauser, C., et al. (2013). Comparison of strategies to reduce methicillin-resistant Staphylococcus aureus rates in surgical patients: A controlled multicentre intervention trial. British Medical Journal Open, 3, e003126. https://doi.org/10.1136/bmjopen-2013-003126
Shrestha, N. K., Fraser, T. G., & Gordon, S. M. (2019). Methicillin resistance in Staphylococcus aureus infections among patients colonized with methicillin-susceptible Staphylococcus aureus. Clinical Microbiology & Infection, 25(1), 71–75. https://doi.org/10.1016/j.cmi.2018.03.045
Sapna, M., Scott, H., Lorraine, H., James, S., Michael, P., Joseph, B. A. (2013) Impact of preoperative MRSA screening and decolonization on hospital-acquired MRSA Burden. Clinical Orthopaedics & Related Research 471(2):2367–2371. https://link.springer.com/content/pdf/https://doi.org/10.1007/s11999-013-2848-3.pdf
Schweizer, M. L., Chiang, H. Y., Septimus, E., Moody, J., Braun, B., Hafner, J., et al. (2015). Association of bundled intervention with surgical site infection among patients undergoing cardiac, hip or knee surgery. JAMA, 313(21), 2162–2171.
Knight, G. M., Dyakova, E., Mookerjee, S., Davies, F., Brannigan, E. T., Otter, J. A., et al. (2018). Fast and expensive (PCR) or cheap and slow (culture )? A mathematical modelling study to explore screening for carbapenem resistance in UK hospitals. BMC Medicine, 14(141), 1–11. https://doi.org/10.1186/s12916-018-1117-4
Smith, M. N., Brotherton, A. L., Lusardi, K., Id, B., Tan, C. A., & Hammond, D. A. (2019). Systematic review of the clinical utility of methicillin-resistant Staphylococcus aureus (MRSA) nasal screening for MRSA Pneumonia. Annals of Pharmacother, 53(6), 627–638. https://doi.org/10.1177/1060028018823027
Borg, M. A., Suda, D., Scicluna, E., Brincat, A., & Zarb, P. (2021). Universal admission screening: A potential game-changer in hospitals with a high prevalence of MRSA. Journal of Hospital Infection, 113, 77–84. https://doi.org/10.1016/j.jhin.2021.03.024
Papastergiou, P., & Tsiouli, E. (2018). Healthcare-associated transmission of Panton-valentine leucocidin positive methicillin-resistant Staphylococcus aureus: The value of screening asymptomatic healthcare workers. BMC Infectious Diseases, 18, 484. https://doi.org/10.1186/s12879-018-3404-2
Sharma, P., & Tomar, R. (2021). Screening of methicillin-resistant Staphylococcus aureus (MRSA) carriage among health care workers and its antibiotic susceptibility pattern in a tertiary care hospital. International Journal of Research and Review, 8(4), 429–434. https://doi.org/10.52403/ijrr.20210451
Varghese, A., Gireesh, M., Janet, P., Jawadagi, S. K. (2021) Effectiveness of information booklet on knowledge regarding methicillin-resistant Staphylococcus aureus (MRSA) among staff nurses. Indian Journal of Public Health Research & Development 19(10):544–9 https://web.p.ebscohost.com/abstract?site=ehost&scope
Labi, A., Obeng-nkrumah, N., Bjerrum, S., Armah, N., Aryee, A., Ofori-adjei, Y. A., et al. (2018). Physicians’ knowledge, attitudes, and perceptions concerning antibiotic resistance: A survey in a Ghanaian tertiary care hospital. BMC Health Services Research, 18(126), 1–12. https://doi.org/10.1186/s12913-018-2899-y
Nicholas, H., Christopher, H.-L., & Nasia, S. (2016). Healthcare personnel attire and devices as fomites: A systematic review. Infection Control and Hospital Epidemiology, 37(11), 1367–1373. https://doi.org/10.1017/ice.2016.192
Grima, G., & Tai, B. (2015). Bedside medication lockers: The hidden danger upon discharge. Journal of Pharmacy Practice and Research, 45, 302–305. https://doi.org/10.1002/jppr.1128
Cheng, V. C. C., Chau, P. H., Lee, W. M., Ho, S. K. Y., Lee, D. W. Y., So, S. Y. C., et al. (2015). Hand-touch contact assessment of high-touch and mutual-touch surfaces among healthcare workers, patients, and visitors. Journal of Hospital Infection, 90, 220–225. https://doi.org/10.1016/j.jhin.2014.12.024
Yuen, J. W. M., Chung, T. W. K., & Loke, A. Y. (2015). Methicillin-resistant Staphylococcus aureus (MRSA) contamination in bedside surfaces of a hospital ward and the potential effectiveness of enhanced disinfection with an antimicrobial polymer surfactant. International Journal of Environmental Research and Public Health, 12, 3026–3041. https://doi.org/10.3390/ijerph120303026
Aboualizadeh, E., Bumah, V. V., Masson-meyers, D. S., Eells, J. T., Hirschmugl, C. J., & Enwemeka, C. S. (2017). Understanding the antimicrobial activity of selected disinfectants against methicillin-resistant Staphylococcus aureus (MRSA). PLoS ONE, 12(7), e0186375. https://doi.org/10.1371/journal.pone.0186375
Brown, N. M., Goodman, A. L., Horner, C., Jenkins, A., & Brown, E. M. (2021). Treatment of methicillin-resistant Staphylococcus aureus (MRSA): updated guidelines from the UK. JAC-Antimicrobial Resistance, 3(1), d114. https://doi.org/10.1093/jacamr/dlaa114
Acknowledgements
We acknowledge the experts for validating the questionnaires and teaching materials; Dr Elissa Ladd, PhD, RN, FNP-BC, Associate Professor, Coordinator -Adult/Gerontology Nurse Practitioner Program, MGH Institute of Health Professions, Boston, Dr Muralidhar Varma, Associate Professor and Chairperson, Hospital Infection Control Committee, Kasturba Hospital Manipal, Manipal Academy of Higher Education, Manipal, Dr Christopher Sudhaker, Professor and Deputy Director, Quality Compliance, Manipal Academy of Higher Education, Manipal, Dr Judith Noronha, Professor and Associate Dean, Manipal College of Nursing Manipal, Manipal Academy of Higher Education, Manipal and Dr Mamatha S. Pai, Professor, Manipal College of Nursing Manipal, Manipal Academy of Higher Education, Manipal.
Funding
Authors of this study did not receive any funding for this study.
Author information
Authors and Affiliations
Contributions
Conceptualization: LT and AKB. Data curation: LT and CM. Formal analysis: LT, AK, and BSN. Investigation: CM, ESD, and BSN. Methodology: LT, AKB, HMH, BSN, and AG. Project administration: LT, AKB, and ESD. Supervision: AKB, HMH, and AG. Validation: LT, AKB, CM, and AG. Writing–original draft: LT, AKB, and ESD. Writing–review and editing: LT, AKB, HMH, CM, ESD, BSN, and AG.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
Institutional research board and Institutional Ethics Committee have approved the study (Reference No: IEC 224/2012).
Consent to Participate
Informed written consent was obtained from all the participants.
Consent for Publication
Consent was obtained from all the participants for publication of their data without disclosing their identity.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Latha, T., Bhat, A.K., Hande, H.M. et al. Effectiveness of Extended Infection Control Measures on Methicillin-Resistant Staphylococcus aureus Infection Among Orthopaedic Patients. JOIO 56, 1804–1812 (2022). https://doi.org/10.1007/s43465-022-00713-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-022-00713-5