Abstract
Purpose
Lateral epicondylitis or lateral elbow tendinopathy is a common condition which needs to be addressed appropriately. This condition usually responds well to non-operative treatment. However, an orthopaedic physician needs to be aware of the recalcitrant cases and equip surgical armamentarium to provide adequate care.
Methodology
The literature search was performed on PubMed, Medline and Google scholar using the keywords Tennis elbow, recalcitrant, thorntons technique, surgical options, for this narrative review.
Conclusion
This article focuses on the causes for recalcitrant tendinopathy and review of its surgical options.



Similar content being viewed by others
References
Briggs, C. A., & Elliott, B. G. (1985). Lateral epicondylitis. A review of structures associated with tennis elbow. Anatomy Clinical, 7(3), 149–153.
Stasinopoulos, D., & Johnson, M. I. (2006). “Lateral elbow tendinopathy” is the most appropriate diagnostic term for the condition commonly referred-to as lateral epicondylitis. Medical Hypotheses, 67(6), 1400–1402.
Ali, M., & Lehman, T. A. (2009). Lateral elbow tendinopathy: A better term than lateral epicondylitis or tennis elbow. Journal of Hand Surgery American, 34(8), 1575. (author reply 6).
Nirschl, R. P. (1973). Tennis elbow. Orthopedic Clinics of North America, 4, 787–800.
Regan, W., Wold, L. E., Coonrad, R., & Morrey, B. F. (1992). Microscopic histopathology of chronic refractory lateral epicondylitis. American Journal of Sports Medicine, 20(6), 746–749.
Chard, M. D., Cawston, T. E., Riley, G. P., Gresham, G. A., & Hazleman, B. L. (1994). Rotator cuff degeneration and lateral epicondylitis: A comparative histological study. Annals of the Rheumatic Diseases, 53(1), 30–34.
Milz, S., Tischer, T., Buettner, A., Schieker, M., Maier, M., Redman, S., et al. (2004). Molecular composition and pathology of entheses on the medial and lateral epicondyles of the humerus: A structural basis for epicondylitis. Annals of the Rheumatic Diseases, 63(9), 1015–1021.
Greenbaum, B., Itamura, J., Vangsness, C. T., Tibone, J., & Atkinson, R. (1999). Extensor carpi radialis brevis. An anatomical analysis of its origin. Journal Bone and Joint Surgery British, 81(5), 926–929.
Nayak, S. R., Ramanathan, L., Krishnamurthy, A., Prabhu, L. V., Madhyastha, S., Potu, B. K., et al. (2010). Extensor carpi radialis brevis origin, nerve supply and its role in lateral epicondylitis. Surgical and Radiologic Anatomy, 32(3), 207–211.
Lieber, R. L., Ljung, B. O., & Friden, J. (1997). Sarcomere length in wrist extensor muscles. Changes may provide insights into the etiology of chronic lateral epicondylitis. Acta Orthopaedica Scandinavica, 68(3), 249–254.
Bunata, R. E., Brown, D. S., & Capelo, R. (2007). Anatomic factors related to the cause of tennis elbow. Journal Bone and Joint Surgery American, 89(9), 1955–1963.
Smith, R. W., Papadopolous, E., Mani, R., & Cawley, M. I. (1994). Abnormal microvascular responses in a lateral epicondylitis. British Journal of Rheumatology, 33(12), 1166–1168.
Vedung, T., Werner, M., Ljung, B. O., Jorfeldt, L., & Henriksson, J. (2011). Blood flow to the extensor carpi radialis brevis muscle following adrenaline infusion in patients with lateral epicondylitis. Journal of Hand Surgery American, 36(12), 1974–1980.
Bales, C. P., Placzek, J. D., Malone, K. J., Vaupel, Z., & Arnoczky, S. P. (2007). Microvascular supply of the lateral epicondyle and common extensor origin. Journal of Shoulder and Elbow Surgery, 16(4), 497–501.
Mitsuyasu, H., Yoshida, R., Shah, M., Patterson, R. M., & Viegas, S. F. (2004). Unusual variant of the extensor carpi radialis brevis muscle: A case report. Clinical Anatomy, 17(1), 61–63.
Fairbank, S. M., & Corlett, R. J. (2002). The role of the extensor digitorum communis muscle in lateral epicondylitis. Journal of Hand Surgery British, 27(5), 405–409.
Ruch, D. S., Papadonikolakis, A., & Campolattaro, R. M. (2006). The posterolateral plica: A cause of refractory lateral elbow pain. Journal of Shoulder and Elbow Surgery, 15(3), 367–370.
Aguililla Linan, J. M., Miguel Perez, M. I., Palau Gonzalez, J., Moller Parera, I., & Martinoli, C. (2020). A comprehensive review of radiohumeral synovial plicae for a correct clinical interpretation in intractable lateral epicondylitis. Current Reviews in Musculoskeletal Medicine, 13, 385–390.
Lee, S. W., Kim, S. G., & Oh-Park, M. (2013). Ganglion cyst of radiocapitellar joint mimicking lateral epicondylitis: Role of ultrasonography. American Journal of Physical Medicine and Rehabilitation, 92(5), 459–460.
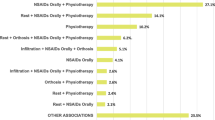
Ma, K. L., & Wang, H. Q. (2020). Management of lateral epicondylitis: A narrative literature review. Pain Research and Management, 2020, 6965381.
Saroja, G., Aseer, P. A., & Venkata Sai, P. M. (2014). Diagnostic accuracy of provocative tests in lateral epicondylitis. International Journal of Physiotherapy and Research, 2(6), 815–823.
Paoloni, J. A., Appleyard, R. C., & Murrell, G. A. (2004). The Orthopaedic Research Institute-Tennis Elbow Testing System: A modified chair pick-up test—interrater and intrarater reliability testing and validity for monitoring lateral epicondylosis. Journal of Shoulder and Elbow Surgery, 13(1), 72–77.
Nirschl, R. P. (1992). Elbow tendinosis/tennis elbow. Clinics in Sports Medicine, 11(4), 851–870.
Almeer, G., Azzopardi, C., Kho, J., & Botchu, R. (2020). Myositis ossificans of mobile wad of Henry-Tennis elbow mimic. The Indian Journal of Radiology & Imaging, 30(1), 89–91.
Faro, F., & Wolf, J. M. (2007). Lateral epicondylitis: Review and current concepts. The Journal of Hand Surgery American, 32(8), 1271–1279.
Walz, D. M., Newman, J. S., Konin, G. P., & Ross, G. (2010). Epicondylitis: Pathogenesis, imaging, and treatment. Radiographics, 30(1), 167–184.
Keijsers, R., de Vos, R. J., Kuijer, P. P., van den Bekerom, M. P., van der Woude, H. J., & Eygendaal, D. (2019). Tennis elbow. Shoulder & Elbow, 11(5), 384–392.
Nirschl, R. P., & Pettrone, F. A. (1979). Tennis elbow. The surgical treatment of lateral epicondylitis. Journal of Bone & Joint Surgery American, 61(6), 832–839.
Dunn, J. H., Kim, J. J., Davis, L., & Nirschl, R. P. (2008). Ten-to 14-year follow-up of the Nirschl surgical technique for lateral epicondylitis. American Journal of Sports Medicine, 36(2), 261–266.
Fridén, J., & Lieber, R. L. (1994). Physiologic consequences of surgical lengthening of extensor carpi radialis brevis muscle-tendon junction for tennis elbow. The Journal of Hand Surgery, 19(2), 269–274.
Barth, J., Mahieu, P., & Hollevoet, N. (2013). Extensor tendon and fascia sectioning of extensors at the musculotendinous unit in lateral epicondylitis. Acta Orthopaedica Belgica, 79(3), 266–270.
Manon-Matos, Y., Oron, A., & Wolff, T. W. (2013). Combined common extensor and supinator aponeurotomy for the treatment of lateral epicondylitis. Techniques in Hand & Upper Extremity Surgery, 17(3), 179–181.
Solheim, E., Hegna, J., & Øyen, J. (2011). Extensor tendon release in tennis elbow: results and prognostic factors in 80 elbows. Knee Surgery, Sports Traumatology, Arthroscopy, 19(6), 1023–1027.
Reddy, V., Satheesan, K. S., & Bayliss, N. (2011). Outcome of Boyd-McLeod procedure for recalcitrant lateral epicondylitis of elbow. Rheumatology International, 31(8), 1081–1084.
Coleman, B., Quinlan, J. F., & Matheson, J. A. (2010). Surgical treatment for lateral epicondylitis: A long-term follow-up of results. Journal of Shoulder and Elbow Surgery, 19(3), 363–367.
Dwyer, A. J., Govindaswamy, R., Elbouni, T., & Chambler, A. F. (2010). Are “knife and fork” good enough for day case surgery of resistant tennis elbow? International Orthopaedics, 34(1), 57–61.
Rayan, F., Rao, V., Sr., Purushothamdas, S., Mukundan, C., & Shafqat, S. O. (2010). Common extensor origin release in recalcitrant lateral epicondylitis-role justified? Journal of Orthopaedic Surgery and Research, 5(1), 31.
Cho, B. K., Kim, Y. M., Kim, D. S., Choi, E. S., Shon, H. C., Park, K. J., et al. (2009). Mini-open muscle resection procedure under local anesthesia for lateral and medial epicondylitis. Clinics in Orthopedic Surgery, 1(3), 123–127.
Svernlöv, B., & Adolfsson, L. (2006). Outcome of release of the lateral extensor muscle origin for epicondylitis. Scandinavian Journal of Plastic and Reconstructive Surgery and Hand Surgery, 40(3), 161–165.
Thomas, S., & Broome, G. (2007). Patient satisfaction after open release of common extensor origin in treating resistant tennis elbow. Acta Orthopaedica Belgica, 73(4), 443–445.
Zingg, P. O., & Schneeberger, A. G. (2006). Debridement of extensors and drilling of the lateral epicondyle for tennis elbow: A retrospective follow-up study. Journal of Shoulder and Elbow Surgery, 15(3), 347–350.
Balk, M. L., Hagberg, W. C., Buterbaugh, G. A., & Imbriglia, J. E. (2005). Outcome of surgery for lateral epicondylitis (tennis elbow): Effect of worker’s compensation. American Journal of Orthopedics, 34(3), 122–126.
Thornton, S. J., Rogers, J. R., Prickett, W. D., Dunn, W. R., Allen, A. A., & Hannafin, J. A. (2005). Treatment of recalcitrant lateral epicondylitis with suture anchor repair. American Journal of Sports Medicine, 33(10), 1558–1564.
Pruzansky, M. E., Gantsoudes, G. D., & Watters, N. (2009). Late surgical results of reattachment to bone in repair of chronic lateral epicondylitis. American Journal of Orthopedics (Belle Mead NJ), 38(6), 295–299.
Wang, W., Chen, J., Lou, J., Shentu, G., Xu, G. (2019). Comparison of arthroscopic debridement and open debridement in the management of lateral epicondylitis: A systematic review and meta-analysis. Medicine, 98(44):44.
Donaldson, C. T., Finley, Z. J., & O’Brien, M. J. (2019). Lateral epicondylitis debridement and repair using knotless suture anchor. Arthroscopy Techniques, 8(7), e775–e779.
Grifka, J., Boenke, S., & Krämer, J. (1995). Endoscopic therapy in epicondylitis radialis humeri. Arthroscopy, 11(6), 743–748.
Cohen, M. S., Romeo, A. A., Hennigan, S. P., & Gordon, M. (2008). Lateral epicondylitis: Anatomic relationships of the extensor tendon origins and implications for arthroscopic treatment. Journal of Shoulder and Elbow Surgery, 17(6), 954–960.
Mullett, H., Sprague, M., Brown, G., & Hausman, M. (2005). Arthroscopic treatment of lateral epicondylitis: Clinical and cadaveric studies. Clinical Orthopaedics and Related Research, 439, 123–128.
Baker, C. L., Jr., Murphy, K. P., Gottlob, C. A., & Curd, D. T. (2000). Arthroscopic classification and treatment of lateral epicondylitis: Two-year clinical results. Journal of Shoulder and Elbow Surgery, 9(6), 475–482.
Moradi, A., Pasdar, P., Mehrad-Majd, H., & Ebrahimzadeh, M. H. (2019). Clinical outcomes of open versus arthroscopic surgery for lateral epicondylitis, evidence from a systematic review. Archives of Bone and Joint Surgery, 7(2), 91.
Pomerantz, M. L. (2016). Complications of lateral epicondylar release. Orthopedic Clinics, 47(2), 445–469.
Shapiro, G. S., & Weiland, A. J. (2002). Reactive bone formation after surgery for lateral epicondylitis. Journal of Shoulder and Elbow Surgery, 11(4), 383–385.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical standard statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
For this type of study informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Herald, J., Ashraf, M., Sundar, M.S. et al. Lateral Epicondylitis-Narrative Review on Surgical Options for Recalcitrant Cases. JOIO 55, 318–324 (2021). https://doi.org/10.1007/s43465-021-00364-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-021-00364-y