Abstract
Background
Lateral ankle sprains are among the common injuries in the physically active population in different age groups and progress to chronic ankle instability (CAI). Accordingly, the current study assesses the effectiveness of strengthening and proprioceptive training programs on proprioception and balance in those suffering from CAI.
Design
Quasi-experimental design.
Methods
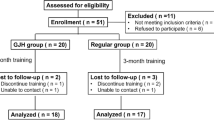
Thirty-six individuals with self-reported CAI were assigned into three groups based on age: group 1 (23 ± 1.84), group 2 (35.80 ± 1.68), group 3 (44.25 ± 4.86), then performed strength and balance exercises for 6 weeks. The study furthermore measured pre- and post-training of joint position sense (JPS), static balance, dynamic balance, chronic ankle instability tool (CAIT) and lower extremity functional scale (LEFS).
Results
Statistical analysis showed significant improvement (P < 0.01) on all outcome measures among all groups. In group 1, mainly the plantar flexion JPS improved to 3.7°, while in group 2 and group 3 the eversion JPS improved to 3.1° and 1.78° (P < 0.01). With reference to static balance with one’s eyes closed and eyes open, the improvement in group 1 was 4.46, 11.05 s, group 2 was 2.23, 7.85 s and group 3 was 1.69, 4.68 s. In relation to dynamic balance, the development in group 1 was 5.85 cm, while group 2 was 4.71 cm and group 3 was 2.49 cm. Moreover, both CAIT and LEFS showed significant differences (P < 0.01) after training.
Conclusion
This study found that combined strengthening and proprioceptive training effectively improves stability, proprioception, balance, and self-reported functional outcomes.




Similar content being viewed by others
References
Gribble, P. A., Delahunt, E., Bleakley, C., Caulfield, B., Docherty, C., Fourchet, F., et al. (2013). Selection criteria for patients with chronic ankle instability in controlled research: A position statement of the international ankle consortium. JOSPT, Inc. JOSPT, 1033 North Fairfax Street, Suite 304, Alexandria, VA
Kaufman, K. R., Brodine, S. K., Shaffer, R. A., Johnson, C. W., & Cullison, T. R. (1999). The effect of foot structure and range of motion on musculoskeletal overuse injuries. The American Journal of Sports Medicine, 27(5), 585–593.
Kannus, P., & Renstrom, P. (1991). Treatment for acute tears of the lateral ligaments of the ankle. Journal of Bone and Joint Surgery American Volume, 73(2), 305–312.
McCriskin, B. J., Cameron, K. L., Orr, J. D., & Waterman, B. R. (2015). Management and prevention of acute and chronic lateral ankle instability in athletic patient populations. World Journal of Orthopedics, 6(2), 161.
Hertel, J. (2000). Functional instability following lateral ankle sprain. Sports Medicine, 29(5), 361–371.
McKeon, P. O., Hubbard, T. J., & Wikstrom, E. A. (2012). Consequences of ankle inversion trauma: A novel recognition and treatment paradigm. An international perspective on topics in sports medicine and sports injury. Rijeka: IntechOpen.
Hertel, J. (2002). Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. Journal of Athletic Training, 37(4), 364.
Delahunt, E., Coughlan, G. F., Caulfield, B., Nightingale, E. J., Lin, C.-W. C., & Hiller, C. E. (2010). Inclusion criteria when investigating insufficiencies in chronic ankle instability. Medicine and Science in Sports and Exercise, 42(11), 2106–2121.
Zouita, A. B. M., Majdoub, O., Ferchichi, H., Grandy, K., Dziri, C., & Salah, F. B. (2013). The effect of 8-weeks proprioceptive exercise program in postural sway and isokinetic strength of ankle sprains of Tunisian athletes. Annals of Physical and Rehabilitation Medicine, 56(9–10), 634–643.
Park, S., Toole, T., & Lee, S. (1999). Functional roles of the proprioceptive system in the control of goal-directed movement. Perceptual and Motor Skills, 88(2), 631–647.
Freeman, M., Dean, M., & Hanham, I. (1965). The etiology and prevention of functional instability of the foot. The Journal of bone and joint surgery British Volume, 47(4), 678–685.
Glencross, D. (1981). Position sense following joint injury. Journal of Sports Medicine and Physical Fitness, 21, 23–27.
Skinner, H. B., Barrack, R. L., & Cook, S. D. (1984). Age-related decline in proprioception. Clinical Orthopaedics and Related Research, 184, 208–211.
Di Giulio, I., Maganaris, C. N., Baltzopoulos, V., & Loram, I. D. (2009). The proprioceptive and agonist roles of gastrocnemius, soleus and tibialis anterior muscles in maintaining human upright posture. The Journal of Physiology, 587(10), 2399–2416.
Röijezon, U., Clark, N. C., & Treleaven, J. (2015). Proprioception in musculoskeletal rehabilitation. Part 1: Basic science and principles of assessment and clinical interventions. Manual Therapy, 20(3), 368–377.
McGuine, T. A., & Keene, J. S. (2006). The effect of a balance training program on the risk of ankle sprains in high school athletes. The American Journal of Sports Medicine, 34(7), 1103–1111.
Janssen, K. W., Hendriks, M. R., van Mechelen, W., & Verhagen, E. (2014). The cost-effectiveness of measures to prevent recurrent ankle sprains: Results of a 3-arm randomized controlled trial. The American Journal of Sports Medicine, 42(7), 1534–1541.
Ha, S.-Y., Han, J.-H., & Sung, Y.-H. (2018). Effects of ankle strengthening exercise program on an unstable supporting surface on proprioception and balance in adults with functional ankle instability. Journal of Exercise Rehabilitation, 14(2), 301.
Docherty, C. L., Moore, J. H., & Arnold, B. L. (1998). Effects of strength training on strength development and joint position sense in functionally unstable ankles. Journal of Athletic Training, 33(4), 310.
Uh, B. S., Beynnon, B. D., Helie, B. V., Alosa, D. M., & Renstrom, A. (2000). The benefit of a single-leg strength training program for the muscles around the untrained ankle: A prospective, randomized, controlled study. The American Journal of Sports Medicine, 28(4), 568–573.
Tropp, H. (1986). Pronator muscle weakness in functional instability of the ankle joint. International Journal of Sports Medicine, 7(05), 291–294.
Fitzgerald, D., Trakarnratanakul, N., Smyth, B., & Caulfield, B. (2010). Effects of a wobble board-based therapeutic exergaming system for balance training on dynamic postural stability and intrinsic motivation levels. Journal of Orthopaedic and Sports Physical Therapy, 40(1), 11–19.
McKeon, P. O., Ingersoll, C. D., Kerrigan, D. C., Saliba, E., Bennett, B. C., & Hertel, J. (2008). Balance training improves function and postural control in those with chronic ankle instability. Medicine and Science in Sports and Exercise, 40(10), 1810–1819.
Hiller, C. E., Refshauge, K. M., Herbert, R. D., & Kilbreath, S. L. (2008). Intrinsic predictors of lateral ankle sprain in adolescent dancers: A prospective cohort study. Clinical Journal of Sport Medicine, 18(1), 44–48.
Binkley, J. M., Stratford, P. W., Lott, S. A., Riddle, D. L., & Network NAORR. (1999). The Lower Extremity Functional Scale (LEFS): Scale development, measurement properties, and clinical application. Physical Therapy, 79(4), 371–383.
Witchalls, J., Blanch, P., Waddington, G., & Adams, R. (2012). Intrinsic functional deficits associated with increased risk of ankle injuries: A systematic review with meta-analysis. British Journal of Sports Medicine, 46(7), 515–523.
Baier, M., & Hopf, T. (1998). Ankle orthoses effect on single-limb standing balance in athletes with functional ankle instability. Archives of physical Medicine and Rehabilitation, 79(8), 939–944.
Duncan, P. W., Weiner, D. K., Chandler, J., & Studenski, S. (1990). Functional reach: A new clinical measure of balance. Journal of Gerontology, 45(6), M192–M197.
Willems, T., Witvrouw, E., Verstuyft, J., Vaes, P., & De Clercq, D. (2002). Proprioception and muscle strength in subjects with a history of ankle sprains and chronic instability. Journal of Athletic Training, 37(4), 487.
Wester, J. U., Jespersen, S. M., Nielsen, K. D., & Neumann, L. (1996). Wobble board training after partial sprains of the lateral ligaments of the ankle: A prospective randomized study. Journal of Orthopaedic and Sports Physical Therapy, 23(5), 332–336.
Thacker, S. B., Stroup, D. F., Branche, C. M., Gilchrist, J., Goodman, R. A., & Weitman, E. A. (1999). The prevention of ankle sprains in sports. The American Journal of Sports Medicine, 27(6), 753–760.
Kaminski, T., Buckley, B., Powers, M., Hubbard, T., & Ortiz, C. (2003). Effect of strength and proprioception training on eversion to inversion strength ratios in subjects with unilateral functional ankle instability. British Journal of Sports Medicine, 37(5), 410–415.
Goble, D. J., Coxon, J. P., Van Impe, A., Geurts, M., Van Hecke, W., Sunaert, S., et al. (2012). The neural basis of central proprioceptive processing in older versus younger adults: An important sensory role for right putamen. Human Brain Mapping, 33(4), 895–908.
Refshauge, K. M., Kilbreath, S. L., & Raymond, J. (2000). The effect of recurrent ankle inversion sprain and taping on proprioception at the ankle. Medicine and Science in Sports and Exercise, 32(1), 10–15.
Taira, T., & Hori, T. (2003). The role of neurosurgical interventions for control of spasticity in neurorehabilitation: New findings on functional microanatomy of the tibial nerve. Neurosurgical re-engineering of the damaged brain and spinal cord (pp. 103–105). Berlin: Springer.
Ryan, L. (1994). Mechanical stability, muscle strength and proprioception in the functionally unstable ankle. Australian Journal of Physiotherapy, 40(1), 41–47.
Powers, M. E., Buckley, B. D., Kaminski, T. W., Hubbard, T. J., & Ortiz, C. (2004). Six weeks of strength and proprioception training does not affect muscle fatigue and static balance in functional ankle instability. Journal of Sport Rehabilitation, 13(3), 201–227.
Jam, B. (2006). Evaluation and retraining of the intrinsic foot muscles for pain syndromes related to abnormal control of pronation. Advanced Physical Therapy Education Institute, 21, 1–8.
Bongiovanni, L., & Hagbarth, K. (1990). Tonic vibration reflexes elicited during fatigue from maximal voluntary contractions in man. The Journal of Physiology, 423(1), 1–14.
Moritani, T. (1979). Neural factors versus hypertrophy in the time course of muscle strength gain. American Journal of Physical Medicine, 58(3), 115–130.
Lee, E., Cho, J., & Lee, S. (2019). Short-foot exercise promotes quantitative somatosensory function in ankle instability: A randomized controlled trial. Medical Science Monitor: International Medical Journal of expErimental and Clinical Research, 25, 618.
Pollock, R. D., Woledge, R. C., Martin, F. C., & Newham, D. J. (2011). Effects of whole body vibration on motor unit recruitment and threshold. Journal of Applied Physiology, 112(3), 388–395.
Torvinen, S., Kannus, P., Sievänen, H., Järvinen, T. A., Pasanen, M., Kontulainen, S., et al. (2002). Effect of four-month vertical whole body vibration on performance and balance. Medicine and Science in Sports and Exercise, 34(9), 1523–1528.
Kim, K.-J., Kim, Y.-E., Jun, H.-J., Lee, J.-S., Ji, S.-H., Ji, S.-G., et al. (2014). Which treatment is more effective for functional ankle instability: Strengthening or combined muscle strengthening and proprioceptive exercises? Journal of Physical Therapy Science, 26(3), 385–388.
Bleakley, C. M., O’Connor, S. R., Tully, M. A., Rocke, L. G., MacAuley, D. C., Bradbury, I., et al. (2010). Effect of accelerated rehabilitation on function after ankle sprain: randomised controlled trial. BMJ, 340, c1964.
Robbins, S., Waked, E., & McClaran, J. (1995). Proprioception and stability: foot position awareness as a function of age and footware. Age and Ageing, 24(1), 67–72.
Miwa, T., Miwa, Y., & Kanda, K. (1995). Dynamic and static sensitivities of muscle spindle primary endings in aged rats to ramp stretch. Neuroscience Letters, 201(2), 179–182.
Masliah, E., Mallory, M., Hansen, L., DeTeresa, R., & Terry, R. (1993). Quantitative synaptic alterations in the human neocortex during normal aging. Neurology, 43(1 Part 1), 192.
Horak, F. B., Shupert, C. L., & Mirka, A. (1989). Components of postural dyscontrol in the elderly: A review. Neurobiology of Aging, 10(6), 727–738.
Stelmach, G. E., & Sirica, A. (1986). Aging and proprioception. Age, 9(4), 99–103.
Acknowledgements
This research work was funded by a Grant (R.G.P1/167/41) from the King Khalid University, Abha, Saudi Arabia.
Author information
Authors and Affiliations
Contributions
KAA and VNK—responsible for the conception and design of study, acquisition and analysis of data. VNK, RSR and PS—drafted the article and approved the final manuscript after critical revision. JST, IA and KR—contributed towards acquisition of data. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard statement
This study involved participation of human subjects and recieved approval from Ethical Committee of King Khalid University (ECM #2019-08).
Informed consent
Informed consent was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alahmari, K.A., Kakaraparthi, V.N., Reddy, R.S. et al. Combined Effects of Strengthening and Proprioceptive Training on Stability, Balance, and Proprioception Among Subjects with Chronic Ankle Instability in Different Age Groups: Evaluation of Clinical Outcome Measures. JOIO 55 (Suppl 1), 199–208 (2021). https://doi.org/10.1007/s43465-020-00192-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-020-00192-6