Abstract
Introduction
Competency-based education has been commonly used to enhance the healthcare workforce for some time. A translational discipline that is integral to drug development and impactful on healthcare and public health is clinical pharmacology. With such contribution, it is essential that the clinical pharmacology workforce is adequately equipped to address the demands of emerging trends of drug development.
Objectives
The primary objective of this study was to determine the most significant competencies needed for a clinical pharmacologist in the regulatory environment.
Methods
A two round modified Delphi technique was administered to 29 clinical pharmacologists within the Office of Clinical Pharmacology (OCP) between November 2021–January 2022.
A questionnaire consisting of core and technical competencies was administered electronically using SurveyMonkey ® to gain consensus about essential clinical pharmacology competencies. Participants used a Likert scale to rank importance of competencies from strongly agree (1), agree (2), neutral (3), disagree (4), strongly disagree (5). Participants also suggested topics to be included in the next round. Consensus was set at 60%. The competencies receiving the most consensus at 60% in round one and the new topics proceeded to the second round. In the second and final round, participants ranked the suggested competencies. Descriptive statistics and a McNemar change test were utilized to analyze data. Only data from the participants who completed both rounds was used in the study.
Results
In round one participants ranked all fifty-six core and technical competencies as essential with consensus of at least 60%. In round two, participants ranked sixty-two competencies as essential with consensus of at least 60%. A McNemar change test demonstrated stability of ranking between rounds.
Conclusion
Essential core and technical competencies can build education programs to sustain the emerging clinical pharmacology workforce in the Office of Clinical Pharmacology. The Delphi technique is a suitable approach to determine essential competencies because it cultivates consensus and gains insight from experts in the forefront of drug development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to the Georgetown University Health Policy Institute [1] 66 percent of adults in the United States take prescription drugs. It is vital that our nation’s drug supply is both safe and effective. An area of healthcare that is cutting edge, translational among disciplines and integral to drug development is clinical pharmacology. With such an impact on public health, it is vital that the clinical pharmacology workforce is properly skilled and trained. A deficit in proper training and skills set will have a negative effect on the workforce’s ability to cope with the dynamic changes impacting drug development [2].
Many healthcare professionals support the use of competencies for education development. Competency is an ability that is observable and integrates several parts such as attitudes, knowledge, skill, and values according to Silva et al. [3] Competencies can be used to validate skills sets in workplace education and have been used in healthcare for quite some time. Competency-based education can significantly prepare the pharmaceutical physician and drug development scientific workforce for opportunities and challenges in the next decade [3]. Recognizing the importance of competency development, the Office of Personnel Management (OPM) launched a Federal Workforce Competency Initiative in April 2021 to ensure the federal workforce has the necessary skills to be successful by recruiting, training, and retaining its people [4]. The initiative will be administered in a series of phases focusing on core and technical competencies. As cutting-edge science emerges, competencies can enable professionals to remain current and well-equipped in the field.
Competencies in clinical pharmacology can develop current staff and the future pipeline [5]. Additionally, the development of a task force to explore the need for leadership competencies in clinical pharmacology can advance the workforce because of their interrelatedness among clinical discipline, science, policy, and public health [5]. The aim of this study was to determine the most significant competencies needed for a clinical pharmacologist in the regulatory environment. Our question sought to determine which competencies would receive the greatest amount of consensus among clinical pharmacologists to address the demands of drug development and emerging trends.
Methods
Delphi Technique
The study design used a modified Delphi technique as shown in Fig. 1.
Diagram of the Delphi Technique. This figure depicts the iterative process in this Modified Delphi Study [6].
This is because instead of initially generating questions in the first round, the study created questions from an existing knowledge matrix previously used in OCP based on Nieforth [7]. The Delphi technique permits effective decision making in healthcare and facilitates consensus in multiple stages [8]. It considers structured group communication where issues that are unknown or incomplete are evaluated by using an iterative process [9]. The objectives for Delphi techniques in health sciences are: “identifying the current state of knowledge; improving predictions of possible future circumstances; resolving controversial judgements; identifying and formulating standards or guidelines for theoretical and methodological issues; developing measurement tools and identifying indicators; formulating recommendations for action and prioritizing measures” [9] (p. 2). The Delphi technique is appropriate to obtain consensus by using questionnaires for data collection from a panel of subject matter experts [10].
Study Location and Administration
The study location was in the Office of Clinical Pharmacology (OCP) at the Food and Drug Administration, Silver Spring, MD. The study was approved and determined as exempt research by the FDA and Drexel University Institutional Review Board because it was intended to enhance quality. The researcher discussed the purpose, goals, and contribution of the study with office leadership and subject matter experts by thoroughly explaining the study process and details. The researcher also emphasized the importance of the study to gain support and boost participation. To develop and review the survey questions, the researcher collaborated with subject matter experts for accuracy to gain intended responses and to ensure content validity. Additionally, the researcher prepared the Delphi study participants by explaining the purpose of the study, the amount of time the study required, the number of study rounds, and the outcome of information gained from the study [8].
Participants
The study enrolled 34 participants, which is within the recommended number for panelists for a Delphi study [11]. The sampling approach used was purposive, a type of non-probability sampling [12]. The participants who served as the Delphi expert panel were clinical pharmacologists and reviewers within the divisions in OCP. As members of OCP, the participants have a vested interest and knowledge which can help increase content validity [8]. Staff in the Immediate Office, fellows, summer students, contractors, interns, and division level leadership who served as experts to develop and review study questions were excluded. All participants received management approval and completed informed consent forms. The participants who were selected because of their education, training, and experience in the discipline could serve as experts to appropriately address the research question. Additionally, participation from all of the divisions promoted diversity in subject matter expertise which is significant for robustness of findings and influential for quality of data [8].
Questionnaire
The modified Delphi study consisted of a questionnaire which was administered electronically using SurveyMonkey ® in two rounds. The questionnaire began with a demographic section about participants’ degree, years of experience, length of time in OCP, length of time at the employer, and length of time in the field. Next, questions were categorized as core competencies and technical competencies with subdomains. The core competency domains were the following: communication, time management, negotiation skills, problem solving, customer service, and functional skills. The technical competency domains were the following: Drug Disposition, Pharmacology and Biomarkers, Quantitative Methods, Drug Safety, Pharmacotherapy, Clinical Trial Methods, and Guidance and Policy. Participants used a Likert scale to rank the importance of the competency from strongly agree (1), agree (2), neutral (3), disagree (4), strongly disagree (5). In the first round of questions, participants ranked the suggested competencies and suggested topics to be included in the next round [13]. The competencies receiving the most consensus at 60% and the new topics proceeded to the next round. In the second and final round, participants ranked the suggested competencies and competencies receiving the most consensus at 60% were determined the essential clinical pharmacology competencies. Only the information from the participants who completed all of the rounds was used in the study.
Data Analysis
Descriptive and nonparametric statistics were used for data analysis. von der Gracht summarized consensus measurement by descriptive data and indicated consensus is meaningful if nominal or Likert scales are used to show agreement [14]. The level of agreement can be used as those suitable in political voting systems such as simple majority, two-third majority and absolute [14] and in this study, 60% indicated the majority. Nonparametric statistics were used because the questionnaire uses a Likert scale, and the measurement should analyze central tendency and level of dispersion [8]. Often Delphi studies use descriptive statistics with a central tendency. Analyzing the data over iterations allows the strength of consensus and merging of opinions [14]. Statistical Package for the Social Sciences (SPSS) (IBM® SPSS® Statistics Subscription) was used to analyze the data of the survey rounds.
A McNemar change test was conducted to determine the stability between the rounds. This was done between the same competencies that were ranked both in rounds one and two. The McNemar change test is a repeated measures test used with nominal data. The McNemar change test is appropriate when comparing the results of the same samples twice in Delphi studies [14]. In this study the consensus of the ranked competencies was compared between the rounds using the same participants. All competencies that ranked strongly agree or agree were coded to yes for consensus and all competencies ranked neutral, disagree, and strongly disagree were coded to no for non-consensus.
Consensus
There is no standardization for consensus in the Delphi method and consensus spans from 51–100% [15]. According to Belton et al. the selection for consensus should provide confidence in the outcome suited to meet the needs of the research topic and has flexibility [11]. The researcher used 60% for consensus with the option to further analyze data for trends among the rounds. According to Pew research 60% is considered a large majority and considers any possible margin of error [16]. Since there is no standardization for consensus, the researcher determined consensus should be representative of the majority with allowance for further evaluation for trends in subsequent rounds. Furthermore, consensus agreement may not have to be set as high if there is not a critical decision and general opinion of trends may be more appropriate [11].
Results
Round One
Participant Demographics
Survey one was sent to thirty-four participants. Thirty-two of thirty-four participants completed round one of the Delphi study with a response rate of 94%. 8 (25%) respondents held a PharmD degree. 16 (50%) respondents held a PhD in pharmaceutical sciences. 8 (25%) respondents held a PhD in another discipline, e.g., chemical engineering, pharmacology and toxicology, biochemistry, pathobiology and molecular medicine, cytogenetics. One respondent with a PharmD also indicated an additional degree, a PhD in pharmaceutical sciences. 4 (12.5%) indicated having 0–3 years of experience in drug development. 9 (28.1%) indicated having 4–10 years of experience in drug development. 7 (22%) indicated having 11–14 years of experience in drug development. 12 (37.5%) indicated having more than 14 years of experience in drug development. 14 (43.8%) indicated having 0–5 years of experience at the Agency. 6 (18.8%) indicated having 6–10 years of experience, 11–14 years of experience and more than 14 years at the Agency, respectively. 15 (46.9%) respondents indicated having 0–5 years of experience in the Office of Clinical Pharmacology (OCP). 8 (25%) indicated having 6–10 years of experience in OCP. 4 (12.5%) indicated having 11–14 years of experience in OCP and 5 (15.6%) indicated having more than 14 years of experience in OCP. As shown in Table 1, responses were representative of the divisions in OCP.
Competencies
All fifty-six competencies were rated as essential; 60% of participants or more rated strongly agree or agree (see Online Resource 1). There was a total of twenty-three core competencies and thirty-three technical competencies. The participants suggested six additional competencies: Domain: Negotiation: Uses listening skills when negotiating; Domain: Drug Disposition: Recognize that drug-drug interactions being translated through the understanding of the drug development program in certain therapeutic areas is essential to public health mission; Domain: Pharmacology and Biomarker: Identifies when to consider targeted biomarker variability, pediatric development variability or diversity of (ethnic/racial) population frequent of biomarker during negotiation of final communication in labeling with stakeholders; Domain: Quantitative Methods: Applies knowledge of disease frequency and prevalence to understand the full spectrum of safety/efficacy evaluation for decision making and communication; Domain: Drug Safety: Utilizes the most appropriate metrics and outcomes in analyses by working closely with drug safety and clinical teams and Apply relevant drug safety competencies in labeling.
Round Two
Participant Demographics
Survey two was sent to thirty-two participants. Twenty-nine participants completed questions in round two with a response rate of 90.6%. 8 (27.6%) respondents held a PharmD. 13 (44.8%) respondents held PhD in Pharmaceutical Sciences. 8 (27.6%) respondents held a PhD in another discipline, e.g., Pharmacology, Chemical Engineering, Pathobiology and Molecular Medicine, Chemistry, Cytogenetics, Cell Biology and Biochemistry. 4 (13.8%) indicated having 0–3 years of experience in drug development. 9 (31.0%) indicated having 4–10 years of experience in drug development. 5 (17.2%) indicated having 11–14 years of experience in drug development. 11 (37.9%) indicated having more than 14 years of experience in drug development. 12 (41.4%) indicated having 0–5 years of experience at the Agency. 5 (17.2) indicated having 6–10 years of experience. 6 (20.7%) indicated having 11–14 years of experience and more than 14 years at the Agency, respectively. 13 (44.8%) respondents had 0–5 years of experience in the Office of Clinical Pharmacology (OCP). 5 (17.2%) indicated having 6–10 years of experience in OCP. 6 (20.70%) indicated having 11–14 years of experience in OCP and 5 (17.2%) indicated having greater than 14 years of experience in OCP. As seen in Table 2, responses were representative of the divisions in OCP.
Competencies
All sixty-two competencies which included the additional six competencies gained from round one were rated as essential; 60% of participants or more rated strongly agree or agree (see Online Resource 2). The following six additional competencies received consensus of 75% or greater: Question 15, Domain: Negotiation: Uses listening skills when negotiating received 96.4% consensus; Question 35, Domain: Drug Disposition: Recognize that drug-drug interactions being translated through the understanding of the drug development program in certain therapeutic areas is essential to public health mission received 93.1% consensus; Question 40, Domain: Pharmacology and Biomarker: Identifies when to consider targeted biomarker variability, pediatric development variability or diversity of (ethnic/racial) population frequent of biomarker during negotiation of final communication in labeling with stakeholders received 79.3% consensus; Question 46, Domain: Quantitative Methods: Applies knowledge of disease frequency and prevalence to understand the full spectrum of safety/efficacy evaluation for decision making and communication received 79.3%; Questions 52–53, Domain: Drug Safety: Utilizes the most appropriate metrics and outcomes in analyses by working closely with drug safety and clinical teams received 89% consensus and Apply relevant drug safety competencies in labeling received 75.9%.
Stability of Rounds One and Two
A McNemar change test was conducted to show stability between rounds [14]. A total of 29 participants ranked competencies for round one and round two. There were some instances where participants skipped responses. The competencies for both rounds one and two received consensus with at least 60% or higher. The results of the McNemar change test were not significant for all competencies, p > 0.05. This signifies stability of ranking between the rounds because there was no difference in consensus between rounds.
Discussion
A well-designed Delphi study determining essential competencies can contribute to the field because it consults regulatory clinical pharmacologists who are at the intersection of drug development [14]. In this Delphi study participants ranked all competencies in rounds one and two as essential competencies in clinical pharmacology for success in the regulatory environment. Delphi studies are commonly done in two to three rounds [8, 9] and this study was concluded in two rounds instead of three because consensus was reached at 60% in the first round. This was attributed to several factors. The preliminary work done to administer the study survey contributed to study success. The researcher was not a clinical pharmacologist by training and remained neutral to administer the study [8]. The researcher modified statements from an existing knowledge matrix to develop the competencies for the study which was time efficient. Additionally, there was a working group consisting of the researcher and subject matter clinical pharmacologists from the office who drafted the questions for the competency study. An additional group of managers reviewed the questions developed by the working group for content and comprehensibility. This approach was similar to Schmalz et al [17] who indicated a well-planned Delphi study in can be done in two rounds.
Participants in this study ranked all competencies as essential with consensus of 60% or greater of strongly agree or agree as 60% is considered a large majority [16]. Most of the competencies in this study received consensus of 70% which is commonly used for consensus [9] or greater with a few exceptions (see online Resource 1 & 2). As 60% was the marker for consensus in this study and most competencies in the study received consensus of at least 70%, the competencies reaching consensus of 80% or greater as shown in Table 3 are considered to be the most significant [13].
The core competency domains are as follows: communication, time management, negotiation skills, problem solving, customer focus, and functional/skills. The core competencies consist of knowledge, skills, and abilities that all clinical pharmacologists in OCP should employ irrespective of their specialization. These competencies describe knowledge and interpersonal skills that staff need when collaborating with multi-disciplinary teams. The technical competency domains are as follows: drug disposition, pharmacology and biomarkers, quantitative methods, drug safety, pharmacotherapy, clinical trial methods, and guidance and policy. The technical competencies consist of foundational knowledge of pharmacology as well as specific subject matter and specialized skill sets.
Delphi studies are also successful when participants have a vested interest and are adequately prepared [8]. The number of respondents who participated, twenty-nine in total, was acceptable for a Delphi study [14]. The researcher prepared study participants by explaining the purpose of the study, the amount of time required, the number of study rounds, and the outcome of information gained from the study and those efforts yielded good results. The information gained from this study can be applied to education efforts within the office and contribute to strategic planning. Participants who volunteered were able to provide their input regarding competencies needed for their work success in the office. Furthermore, competency development directly aligns with one of the areas of the New Drugs Regulatory Program Modernization for the Agency and this work supports that initiative [18].
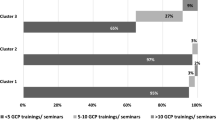
The diversity of the participant backgrounds also strengthened the study [17]. There was representation among all the divisions in OCP as seen in Tables 1 and 2. Participants had work history in different settings. Many participants had a greater number of years of experience in drug development than in OCP and the Agency. In round one 59.5% of participants had 11 or more years of experience in drug development. In comparison 46.9% of participants in round one had 0–5 years of experience in OCP and 43.8% of participants had 0–5 years of experience at the Agency. In round two 55.1% of participants had 11 or more years of experience in drug development. In comparison 41.4% of participants only had 0–5 years of experience at the Agency and 44.8% of participants had 0–5 years of experience in OCP. This suggests that participants may have had experience in the pharmaceutical industry settings or academia and that experience enabled them to rank the competencies. There were several participants who had many years of experience in the government setting. In round one 28.1% of participants had 11 plus years of experience in OCP. In round two 37.9% of participants had 11 or more years of experience in OCP. This mixture of participant experience added value to the study. Participants who had experience in drug development as both as a regulator and in industry had a unique perspective regarding competencies needed for success in the work setting.
Limitations
Delphi studies by design inherently use purposive sampling and not randomized because they rely on the expertise of its participants. The study participants were from one office located in one agency. Although the number of the participants was within the accepted number for the Delphi technique [14], increasing the number to include participants from the entire office or clinical pharmacologists from other offices could further diversify the findings. The participants being from one office also posed challenges with inferential statistics. A McNemar test was conducted to show stability between rounds as referenced by von der Gracht [14]. A McNemar test was performed although the selection of participants was not a true random sample. The results demonstrated no significant difference between the two rounds thus showing stability in responses. Furthermore, the newly gained competencies included in round two were only ranked once because the study concluded in two rounds. Therefore, the McNemar test could not be performed and there was no comparison of the newly gained competencies. As consensus of 60% was used to determine the essential competencies, descriptive statistics were utilized for the results and conclusion of study. It should be noted that these findings are applicable for this particular office. [19] However, these study findings can influence the use of competencies in the workforce beyond OCP.
Study Contributions/Implications for Practice
Our findings suggest core and technical competencies in the Office of Clinical Pharmacology can build essential training programs. This supports Brouwer et al. [2] who indicated training programs should include both specialized and essential competencies in clinical pharmacology and the importance of competency-based education [20]. These programs can enhance existing programs and provide an education framework to focus on staff development, scientific and regulatory training as well as pipeline development. Additionally, the Delphi method is a good consensus tool to determine essential competencies in clinical pharmacology in the regulatory environment. Regardless of technical background or specialization, the participants agreed on what they considered essential competencies for success in the workplace. An approach would be to utilize this information to enhance the knowledge, skills and, abilities of all OCP staff from beginner to experienced clinical pharmacologists. Since all core and technical competencies were deemed essential, the office could initially develop programs focusing on the core competencies, guidance competencies and the technical competencies receiving 80% or higher consensus until all of the competencies have been addressed [13]. These competencies can be a framework to establish and enhance education programs addressing workforce needs. Furthermore, competencies can be used to develop job profiles which specify the knowledge, skill, and abilities of suitable applicants [21].
Competencies are used for academic, self- assessment or professional purposes [21]. To further contribute to pipeline development universities could consider developing programs or curriculum that focus on the core and technical competencies in clinical pharmacology or other areas in drug development to develop the future workforce [20]. This can prepare students not only for academia, but other work settings such as industry or the government workforce [22]. Continued research is needed to align curriculum development to meet market demands promoting advancements in science [22]. Organizations could have a team dedicated to enhancing workforce development and education to remain abreast on ongoing research in competency development in pharmaceutical medicine and the drug development workforce to create competency-based programs.
It is important to establish a deliberate approach for developing scientists spanning from students to workforce professionals [5]. This study enhanced the previous knowledge matrix of core and technical clinical pharmacology competencies. There should be ongoing discussion about the use of competencies and relatedness to the emerging field because of the constant changes in drug development [21]. Competency development uses an iterative process and competencies need to be updated regularly since they have a span of 3–5 years to ensure the workforce has the necessary knowledge, skills, and abilities for optimal job performance [21]. Doing so prepares the workforce to handle the emerging landscape of drug development thus advancing public health.
Conclusion
Essential core and technical competencies can build education programs to sustain the emerging clinical pharmacology workforce in the Office of Clinical Pharmacology. A well-planned Delphi study is a suitable consensus tool to determine essential clinical pharmacology competencies. Competencies can motivate standardization of skills and knowledge needed in clinical pharmacology to maintain a robust workforce.
Data availability
Not applicable.
References
Prescription drugs. Health Policy Institute. Published February 13, 2019. Accessed February 27, 2022. https://hpi.georgetown.edu/rxdrugs/
Brouwer KLR, Schmidt S, Floren LC, Johnson JA. Clinical pharmacology education - the decade ahead. Clin Pharmacol Ther. 2020;107(1):37–9. https://doi.org/10.1002/cpt.1652.
Silva H, Stonier P, Buhler F, et al. Core competencies for pharmaceutical physicians and drug development scientists. Front Pharmacol. 2013. https://doi.org/10.3389/fphar.2013.00105.
US Office of Personnel Management launches Federal Workforce Competency Initiative FWCI) to build stronger federal workforce capability [Press release]. Office of Personnel Management. Accessed November 23, 2022. https://www.opm.gov/news/releases/2021/04/release-us-office-of-personnel-management-launches-federal-workforce-competency-initiative-fwci-to-build-stronger-federal-workforce-capability/. Published April 9, 2021.
Zineh I, Hartman D. What’s past is prologue: clinical pharmacology at the intersection of science, policy, and patients. Clin Pharmacol Ther. 2020;107(1):33–6. https://doi.org/10.1002/cpt.1650.
Birko S, Dove ES, Özdemir V. A Delphi technology foresight study: mapping social construction of scientific evidence on metagenomics tests for water safety. PLoS One. 2015;10(6):e0129706. https://doi.org/10.1371/journal.pone.0129706.
Nieforth KA, Abdallah HY, Smith P, et al. Clinical pharmacology knowledge, opportunities and working strengths (CPKNOWS): a competency model for pursuit of excellence in clinical pharmacology. Br J Clin Pharmacol. 2013;76(6):841–5. https://doi.org/10.1111/bcp.12119.
Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. 2000;32(4):1008–15.
Niederberger M, Spranger J. Delphi technique in health sciences: a map. Front Pub Health. 2020;8:457. https://doi.org/10.3389/fpubh.2020.00457.
Hsu CC, Sandford BA. The Delphi technique: making sense of consensus. Pract Assess, Res, Evaluat. 2007;12(1):10.
Belton I, MacDonald A, Wright G, Hamlin I. Improving the practical aplication of the Delphi method in group-based judgment: A six-step prescription for a well-founded and defensible process. Techn Fore and Soc Change. 2019;1(147):72–82.
Portney, L.G., & Watkins, M.P. 2015 Foundations of clinical research: Application to practice. (3rd edition). FA Davis Company
ENA Np Validation Work Team, Hoyt KS, Coyne EA, et al. Nurse practitioner delphi study: competencies for practice in emergency care. J Emerg Nurs. 2010;36(5):439–49. https://doi.org/10.1016/j.jen.2010.05.001.
von der Gracht. Consensus measurement in Delphi studies review and implications for future quality assurance. Techn Fore and Soc Change. 2013;79:1525–36. https://doi.org/10.1016/j.techfore.2012.04.013.
Barrett D, Heale R. What are Delphi studies? Evid Based Nurs. 2020;23(3):68–9. https://doi.org/10.1136/ebnurs-2020-103303.
5 things to know about the margin of error in election polls. Pew Research Center. Published September 8, 2016. Accessed November 23, 2021. http://pewrsr.ch/2ccg5zC
Schmalz U, Spinler S, Ringbeck J. Lessons learned from a two-round Delphi-based scenario study. MethodsX. 2020;8:101179. https://doi.org/10.1016/j.mex.2020.101179.
Bugin K, Woodcock J, Stein P, Sharma K, Tyberg Y. New drugs regulatory program modernization: vision, strategic objectives, and impact. Ther Innov Regul Sci. 2021;55(2):440–6. https://doi.org/10.1007/s43441-020-00234-z.
Andrade C. The inconvenient truth about convenience and purposive samples. Indian J Psychol Med. 2021;43(1):86–8. https://doi.org/10.1177/0253717620977000.
Dubois DJ, Jurczynska A, Kerpel-Fronius S, et al. Fostering competence in medicines development: the IFAPP perspective. Front Pharmacol. 2016;7:377. https://doi.org/10.3389/fphar.2016.00377.
Stonier PD, Silva H, Boyd A, et al. Evolution of the development of core competencies in pharmaceutical medicine and their potential use in education and training. Front Pharmacol. 2020;11:282. https://doi.org/10.3389/fphar.2020.00282.
McLaughlin JE, Minshew LM, Gonzalez D, et al. Can they imagine the future? a qualitative study exploring the skills employers seek in pharmaceutical sciences doctoral graduates. PLOS ONE. 2019. https://doi.org/10.1371/journal.pone.0222422.
Funding
Not applicable. Funding was not needed for this study as it was completed at a government agency.
Author information
Authors and Affiliations
Contributions
This work was the dissertation of BJ-W for the partial completion of the doctoral degree at Drexel University. Dr. AR† served as the dissertation chair and Drs. KR and JG served as committee members.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest associated with the publication and no significant financial support for this work that could have influenced the outcome.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Johnson-Williams, B., Reynolds, K., Gobburu, J. et al. A Modified Delphi Study to Establish Essential Clinical Pharmacology Competencies. Ther Innov Regul Sci 58, 473–482 (2024). https://doi.org/10.1007/s43441-023-00609-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43441-023-00609-y