Abstract
Introduction
Promptly providing new drugs to fulfill unmet medical needs requires changes in drug development and registration processes. Health Authorities (HAs) considered as reference due to their experience and acknowledgement (Food and Drug Administration [FDA] among others) already consider innovative clinical trial (CT) designs and flexible approval procedures, but Latin America (LATAM) regulations are still far. A comparison was performed to identify gaps.
Materials and Methods
CT requirements for drug Marketing Authorization Application (MAA) and CT approval regulations were compared between LATAM and reference HAs (FDA/European Medicines Agency [EMA]/Health-Canada/Swissmedic/Therapeutic Goods Administration [TGA]/Pharmaceuticals and Medical Devices Agency [PMDA]), as of August 2022. Procedure included reference HAs regulations review, item selection, identification in LATAM regulations, and International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) guidelines (ICH-E6[R2]/ICH-E8[R1]) implementation revision.
Results
For MAA, specific application requirements or ICH guideline M4(R4) on common technical document (CTD) adoption are generally stated, and phase-I/III performance is mandatory (explicitly/implicitly). Faster patient access procedures are infrequent: Priority-drug programs, conditional authorizations, or expedited procedures are scarce or non-existent. Regulatory reliance procedures are adopted through different pathways. Regarding CT approval, innovative/complex CT designs are not prohibited but usually omitted. Some countries implemented adapted CT conducting during the COVID-19 pandemic. Early scientific advice meetings (HA-sponsor) are occasionally considered. Most countries are not formally ICH-joined.
Conclusions
LATAM regulations must adapt to new regulatory standards (FDA/EMA/ICH) through implementation of frequent updates, reliance/expedited procedures, early HA-sponsor interactions, innovative/complex CTs, mandatory phase-III reaching elimination, and decentralized elements for CT conducting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The need to provide innovative drugs promptly to patients to fulfill unmet medical needs is changing the drug development scene. It has been demonstrated that the traditional approach to evidence generation poses challenges to achieving the necessary efficient development that could lead to rapid drug approval [1, 2]. In most countries, the necessary change is hindered at marketing and pre-marketing authorization levels: Requirements for new drug/indication approval still entail data obtained from the traditional phase I–III studies, and CT authorization regulations do not always consider new CT designs.
Advances in research methodologies and new technologies offer tools to implement innovative and efficient ways to investigate drugs [3, 4], fostering their availability faster [4].
New CT approaches include enrichment designs [5], adaptive designs [6], master protocols (umbrella, basket, or platform designs) [5], and use of historical controls [5].
These strategies are already being implemented and accepted, by the Food and Drug Administration (FDA), for authorization of new treatments in many pathologies, especially in oncology [7, 8]. In this sense, a survey performed in 32 pharmaceutical companies [9] revealed that 66% had conducted innovative CTs to provide evidence for many purposes, including for first drug approval in 59% of the companies.
Some Health Authorities (HAs), considered as reference due to their experience and international acknowledgement, through continuous updating, have taken actions (guidelines and initiatives) to be open to evidence coming from innovative CTs. The FDA led this change, beginning in 2004 (“Critical Path Initiative for transforming development, evaluation, and manufacturing of medical products”) [10] and continuing afterward (in 2018, “Complex Innovative Trial Designs Pilot Meeting Program”) [5]. The European Medicines Agency (EMA) started in 2007 (“Reflection Paper on Methodological Issues in Confirmatory Clinical Trials Planned with an Adaptive Design”) [10] and also carried out later actions (in 2019, “Recommendation Paper on the Initiation and Conduct of Complex Clinical Trials”) [11]. Health Canada and Medicines and Healthcare products Regulatory Agency (United Kingdom) consulted with stakeholders in 2020 and 2021, respectively, for the modernization of CT regulatory frameworks [12, 13]. Relevant questions were considered such as a more agile life cycle approach, including new types of innovative CTs and improving timelines, a risk-based approach, the performance of decentralized CTs, modernization of compliance and enforcement, collaboration across sectors, education on regulatory science, or the use of real-world data, among others [12, 13].
Reference HAs have also established alternative pathways to the traditional Marketing Authorization Application (MAA), such as priority-drug programs [14], expedited review [15], conditional approval [15], and reliance pathway [16].
In the case of Latin America (LATAM) countries and those Caribbean islands with regulations (Argentina, Aruba, Bolivia, Brazil, Chile, Colombia, Costa Rica, Cuba, Curacao, Dominican Republic, Ecuador, El Salvador, Guatemala, Guyana, Honduras, Jamaica, Mexico, Nicaragua, Panama, Paraguay, Peru, Sint Maarten, Trinidad and Tobago, Uruguay, and Venezuela), for MAA and traditional CT authorization, these are not as exhaustively described as those in other countries. Therefore, a new drug/indication may find delays, or even no chance, of being available to patients due to either a specific prohibitive regulation or the lack of flexibility in the regulation. On the other hand, some procedures and initiatives to overcome these challenges are implemented, albeit with differences across LATAM countries [17, 18]. However, there is no available analysis of the whole landscape that could help us to undertake accurate actions in each country to speed drug marketing approval.
Our primary objective was to evaluate the situation of the regulations for drug registration in relation to the CT requirements of LATAM. This was compared with those of the main reference HAs to identify gaps that hinder rapid drug development and propose recommendations to close them.
Materials and Methods
To evaluate MAA requirements and CT approval regulations, LATAM countries and those Caribbean islands with regulations, described in the Introduction section, were chosen. Reference HAs selected were FDA, EMA, Health Canada, Swissmedic, Therapeutic Goods Administration (TGA) in Australia, and the Pharmaceuticals and Medical Devices Agency (PMDA) in Japan.
Reference HAs and LATAM regulations were reviewed by examining the contents published on their corresponding websites. A comprehensive search was done in each country through an initial review followed by an in-depth one when contents of interest were not found initially.
Relevant items (key concepts) to address the gaps, selected by analyzing the reference HA regulations, corresponded to different steps in drug development and belonged to two main categories: (1) MAA and (2) CT authorization. Key concepts for each category and their descriptions considered for the purpose of this evaluation are detailed in Table 1.
In addition, we reviewed the implementation of two International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) guidelines belonging to the efficacy category: E6-Good Clinical Practice (R2) (ICH E6 [R2]) and E8-General Considerations for Clinical Trials (R1) (ICH E8 [R1]).
Information regarding key concepts from LATAM and reference HAs was searched as of August 2022 and organized into tables. Next, gaps and relevant differences with respect to reference HAs were identified. Finally, actions were proposed to improve marketing approval and CT development requirements in LATAM countries.
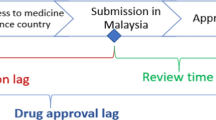
Figure 1 shows a diagram with our data analysis procedure.
Results
The findings on the regulations for each process (MAA and CT authorization) are presented separately below.
MAA Procedures
Overall, while most of the key concepts selected to assess the MAA requirements were found in reference HAs, especially FDA and EMA (Table 2), LATAM regulations frequently lacked the corresponding items. This absence is remarkable for the MAA procedures that intend to achieve faster patient access to drugs (except reliance pathways).
Unless otherwise stated, the reviewed regulations apply to chemical and biological products.
Standard MAA requirements are described more exhaustively in reference HAs than LATAM regulations, where the extent of contents can vary significantly among countries. Four of twenty-five countries assessed in LATAM have no local regulation, so they adopt international indications such as the “ICH guideline M4 (R4) on common technical document (CTD) for the registration of pharmaceuticals for human use—organization of CTD Module 2. Common Technical Document Summaries”. The requirement of phase I-III study development to obtain drug approval is specified in Chile, Brazil, Ecuador, and Venezuela regulations and in countries adopting Central American Technical Regulations (RTCA for its acronym in Spanish), which are Costa Rica, El Salvador, Guatemala, Honduras, Nicaragua, and Panama.
For innovative biotechnological products, Guatemala considers an exemption of phase III studies in exceptional cases of early development of clinically relevant drugs if previously authorized by a WHO-classified reference HA. This is referred to that biotechnological product first marketing-authorized in the first origin country, supported by the complete quality, safety, efficacy, and immunogenicity documentation, being the reference product. No specification for the required phases was found in 8 of 25 LATAM countries. However, when searching information regarding CT conducting before drug commercialization, these regulations only mention the traditional phase I–III development, apart from Cuba, where the possibility of having overlapped phases (i.e., a phase II/III CT) is considered.
In many cases, a separate section is found for biological drugs, globally defined as those of which obtaining and/or production involves living organisms, as well as their fluids or tissues.
An abbreviated procedure for new drug application that is a generic/bioequivalent drug of authorized one is implemented in all reference HAs. However, in LATAM regulations, this process is only included in Chile (with a specific mention for biotechnological products), Colombia and countries adopting RTCA, besides, Guatemala has its own regulation.
In general, procedures for faster patient access to new drugs can be grouped into four classes: programs for priority drugs, expedited review, conditional approval, and reliance pathways.
Programs for priority drugs are focused on drugs aimed to cover unmet needs in serious or life-threatening diseases and directed to provide faster development and evaluation for earlier availability to patients. They are named differently by each HA. These programs are only implemented in FDA (Fast-track), EMA (Priority medicines [PRIME]), and PMDA (Strategy of SAKIGAKE). They are not present in the rest of the reference HAs or LATAM regulations.
Regarding expedited review, which implies procedures that shorten the time for evaluation of the MAA for innovative drugs of interest for public health, it receives distinct designations across regulations. All reference HAs have implemented this process with different features (priority review in FDA, TGA, Health Canada, and Japan, accelerated assessment in EMA, and fast-track procedure in Swissmedic). In LATAM regulations, they are considered in some countries, as shown in Table 2. Brazilian normative establishes that for the registration of a new drug aimed to prevent or treat serious diseases being life-threatening or heavily debilitating, if it fulfills an unmet medical need, phase-III CTs are not necessarily to be ended, or even only ended phase-II CTs are required if phase-III CTs are not applicable (also for biologicals). There is an expedited procedure in Chile, since 2020, for chemical drugs, and is planned to be widened to biological products under certain circumstances. In the case of Colombia, authorities prolonged for 6 months the urgency approval procedure for COVID-19 drugs.
Conditional approval is granted for drugs treating serious or life-threatening diseases that provide meaningful therapeutic benefit over existing treatments, for which promising data from phase I–II CTs or from surrogate endpoints are obtained. It implies an engagement by the marketing authorization holder to comply with a post-marketing plan to develop confirmatory studies and evaluation of safety issues to obtain the “full approval”. This procedure is found under different denominations among regulations. All reference HAs have included this procedure. In LATAM countries, this procedure was found in Venezuela (for extendable 6-month periods) and Honduras (6-month permission for imported drugs) only.
Regulatory reliance is not implemented by reference HAs, except Swissmedic. However, some LATAM countries consider diverse reliance pathways (see Table 2). Those presenting an official procedure are Argentina, Chile, Colombia, Costa Rica, Dominican Republic, Ecuador, El Salvador, Guatemala, Honduras, Mexico, Nicaragua, Panama, Peru, and Uruguay. A collaborative reliance (Joint Mechanism for the Evaluation of drug product files in Central America), not yet for biologicals, among countries was recently implemented in Costa Rica, El Salvador, Guatemala, Honduras, Nicaragua, and Panama (the two last ones are not actively involved). Colombia and Peru mention the reliance on adoption in their regulation; however, there have been very few examples in practice. In the case of Ecuador, the current process does not represent a better timeline for regulatory evaluation. The National Health Surveillance Agency (ANVISA for its acronym in Portuguese) in Brazil is still evaluating the comments from an industry survey before implementing a formal procedure. In addition, reliance is also applied by the Caribbean Regulatory System (CRS), being currently adopted by Guyana and Trinidad and Tobago only.
CT Authorization Application
Generally, most of the key concepts selected to assess CT approval regulations were found in reference HAs, especially FDA and EMA (Table 3), however LATAM regulations frequently lacked the corresponding concepts, being striking for complex, innovative CT designs (Table 3).
With respect to CT approval requirements, the definition of CT and investigational phases are described in reference regulations. Most LATAM ones include CT (or synonymous term) definition. This was not found in countries with low performance of CTs (Aruba, Curacao, Guyana, Jamaica, Sint Maarten, and Trinidad and Tobago). In the case of Honduras, although there is CT normative, no definition of such activity is included in its regulations.
In the countries that describe the type of CT and its phases, they refer to the standard phases (I, II, III, and IV). Some regulations containing CT definition do not include the description of the phases, such as Dominican Republic, El Salvador, and Panama. Generally, in both LATAM and reference regulations, phases I, II, III, and IV are described following the traditional concepts of drug development. However, when defining CT in Cuba, they consider the possibility of overlapped phases (i.e., a phase II/III CT). In the case of phase III, it is usually defined as the phase providing the needed confirmatory information for the studied indication, and even mention of its support for marketing authorization is clearly stated in some regulations.
Requirements for CT application (standard procedure) are described in reference and almost all LATAM regulations, as shown in Table 3. In the case of Health Canada, although not yet approved, a proposal to make the procedure more flexible is in progress. Overall, there is no explicit prohibition to carry out CTs with innovative designs. However, in some LATAM countries (Argentina, Chile, Colombia, Dominican Republic, Ecuador, El Salvador, Honduras, and Mexico) some type of specification about traditional phases (I–IV) are described, so it could be understood that only standard CT designs are considered under those regulations. In Cuba, as explained above, CTs with overlapped phases are possible.
As an alternative procedure to accelerate CT approval, the reliance pathway based on previous authorization by other HA is considered in Argentina and Guatemala, although is not included by reference HAs.
During COVID-19 pandemic, flexible procedures to facilitate CT conduct were set by most reference HAs and some LATAM countries (see Table 3).
Regulations for the innovative cell therapy CTs were found in most of reference regulations, but only in Argentina for LATAM countries, being less exhaustive, specially vs. FDA, EMA, or Health Canada, although the main principles are considered equally.
All reference HAs have set scientific advice meetings with sponsors, in some steps of the drug development, to contribute to the earlier access of the patient to new drugs and to foster more effective drug development by improving scientific resource utilization and enhancing patients’ participation. In the EMA, early advice is offered via the Innovation Task Force meeting. This type of meeting is only considered in Argentina, Brazil, and Mexico for LATAM countries.
With respect to complex innovative trial designs, master protocols (umbrella, basket, and complex trials with features of both) are described in a guidance for industry in FDA, being a part of the category of complex CTs. EMA and Swissmedic consider master protocols by relying on the recommendation paper of the Clinical Trial Facilitation and Coordination Group (CTFG). Health Canada consulted stakeholders in 2021 about the modernization of CTs, where this concept was treated (including its implementation for pediatric studies), but the results of the consult have not been implemented yet. TGA also considers these concepts in its regulations. No corresponding information was found for PMDA. None of LATAM countries have implemented normative for master protocols.
Adaptive designs are considered by most reference HAs (see Table 3). Only in Guatemala and Bolivia the term “sequential clinical trial” is found, where the final sample size depends on the intermediate results of the trial. No other related information is found in the rest of the LATAM regulations.
Enrichment designs are described in FDA regulations. The EMA and Swissmedic rely on the CTFG recommendation paper and the Q&A on complex clinical trials from EMA. Other reference HAs and LATAM countries do not include this strategy.
Aspects about decentralized CTs that use digital health technologies for remote data acquisition are present in almost all reference HAs, as shown in Table 3. However, this concept is not found in LATAM regulations.
Regarding the adoption of ICH E6 (R2) and ICH E8 (R1) (Table 3), reference HAs, all ICH members except TGA (observer), have implemented, or are in the process of implementing, these guidelines. For LATAM countries, Brazil and Mexico are members, but these guidelines are only implemented in Brazil. Argentina, Colombia, and Cuba are observers. The rest of LATAM countries have not formally joined the ICH.
Discussion
MAA and CT authorization regulations are aspects that must be changed to facilitate quicker and safe access of patients to new drugs.
Our review provides an overview of the current procedures for MAA and CT approval that are discussed below:
MAA Procedures
Overall, patient access to new drugs is not as rapid as required to address unmet medical needs. The standard drug approval procedures currently established by many HAs, imply numerous and, sometimes, complex steps [15].
In this research work, first, we reviewed the requirements for MAA. All LATAM countries consider regulations regarding this concept, although some of them do not have specific local rules; therefore, they adopt international ICH guideline M4.
The need for phase I–III development, as a traditional requirement, is stated in some regulations (Chile, Brazil, Ecuador, and Venezuela), including those countries adopting RTCA where conclusive data of such CTs are required; Guatemala has an exemption of phase III studies for exceptional drugs of clinical relevance previously authorized by a WHO-classified reference HA. For the rest of countries having local regulations, no such specification appears but considering CTA requirements, some type of specification about traditional phases before drug registration is described. Therefore, it could be understood that they only consider traditional CT designs, apart from Cuba, where a flexible feature is found when defining the term “clinical trial” with the possibility of phase-combined studies.
The review of the procedures to speed MAA and provide faster patient access showed that there are programs for priority drugs that are promising to cover unmet medical needs. These programs shorten the drug development and the marketing approval for an indication and are included in three of the reference regulations (FDA, EMA, and PDMA). In the case of the FDA, once a drug receives “fast track” designation, early and frequent communication with the drug company is encouraged throughout the entire drug development and review process, and often leading to earlier drug approval and access by patients [19]. These types of programs, not considered by LATAM and the rest of the reference regulations, are difficult to implement, although they would be very effective as it reduces the time for drug development from early phases. Secondly, expedited review, which reduces the time for evaluating a MAA, such as the “priority review” program in FDA that leads to review in 6 months vs. 10 months for a standard review [20], is included in some LATAM regulations. Brazilian normative also considers that phase III studies do not necessarily need to be ended, or even only ended phase II studies are required when phase III CTs are not applicable, for the registration of a new drug aimed to prevent or treat serious diseases that are life-threatening or heavily debilitating if it fulfills an unmet medical need. A third way to accelerate access to new drugs is through conditional approval, which grants early authorization for drugs considered especially needed but requires further data obtained during post-marketing use to get the definitive approval. This is not usually accepted by LATAM HAs (with two exceptions: Venezuela and Honduras), in contrast to all reference regulations. Overall, these types of expedited procedures reduce the timelines for drug development when implemented by HAs. For example, the median development time for drugs in at least 1 expedited program was 7.1 years (interquartile range [IQR], 5.1–10.1) compared with 8.0 years for non-expedited drugs (IQR, 6.5–10.0; P = 0.04) [20].
In LATAM regulations, however, it is more common to find some type of reliance procedure to speed up the drug approval process. This mechanism is implemented through several ways across countries. Reliance in a formal manner, implying an immediate authorization if the drug is already approved by recognized HAs, is adopted by Argentina, Brazil (in progress), Chile, Costa Rica, Guyana, and Trinidad and Tobago. This pathway has the advantage of being quicker than other reliance modalities, such as the abbreviated procedure (Mexico and Panama), recognition of clinical studies (Costa Rica and Uruguay), recognition of chemical products and vaccines approved by PAHO (Guatemala), recognition of foreign registrations (El Salvador), homologation (Ecuador, Guyana, and Trinidad and Tobago), simplified procedure (Dominican Republic), accelerated procedure (only for biologics, in Chile, El Salvador, and Peru), or collaborative reliance (Costa Rica, El Salvador, Guatemala, Honduras, Nicaragua, and Panama). Countries implementing these types of reliance procedures could be more receptive to adopting a formal one, thereby facilitating quicker drug MAA approval. On the other hand, those countries that mention the reliance procedure in their regulations, but their implementation is not done (Colombia and Peru) or do not even shorten timelines (Ecuador) should modify their specifications to make this procedure real and effective. WHO supports the use of the reliance pathway with recommendations that HAs adopt these types of approaches that take into account decisions from reference agencies and evaluate only specific issues of local responsibility [21].
Currently, there are examples of drugs getting marketing approval by using innovative trial designs. Adaptive designs (including adaptations in formulation selection, new primary efficacy endpoint, dose selection, or sample size adjustment) and master protocols (basket, umbrella, and platform) have been used as part of the evidence dossier to get marketing approval from FDA and EMA [5, 10]. The different authorizations were granted for diseases including hematological malignancies and solid tumors (melanoma, breast cancer, urothelial carcinoma, among others), and included adult and pediatric populations. Some of them were accelerated or conditional approvals following a phase II trial [10, 22].
An example of an initiative that considers innovative CT designs and early alignment among stakeholders, including the FDA and the EMA, is ACCELERATE [23]. ACCELERATE aimed to accelerate the authorization of innovative treatments for children and adolescents with cancer so they can benefit rapidly and reduce the burden of further sequelae.
Although this review did not include the regulations about real-world evidence (RWE) use as a support in pre-marketing for decision-making, it is worth mentioning that this new approach, incorporated into regulatory processes by FDA and the EMA and by other regulatory bodies in an earlier stage [10], has not been found in LATAM regulations.
CT Authorization Application
Traditional CTs, although being considered the paradigm of drug research, show issues that hamper the agile arrival of needed drugs to the market [1, 2].
Comparing LATAM and reference regulations, a relevant difference is observed with respect to innovative CT design descriptions (master protocols, adaptive designs, enrichment strategies, or decentralized CTs). Most reference regulations include these new approaches that allow faster patient access to new drugs [10, 24, 25] but most LATAM countries have not considered them in their rules or guidances for CT approval procedures. This means that, although innovative CT designs are not explicitly forbidden, usual CT designs and traditional phases (I-III) should still be followed before marketing approval is obtained in these countries. Currently, in the case that innovative designs could be considered during the development of any drug, their implementation is difficult or even not possible due to the lack of regulation. During the COVID pandemic, unusual methods to carry out CTs had to be implemented [26, 27], showing that more flexible procedures were safe and effective. Thus, it was demonstrated that it is possible to change standard designs without losing reliability in the clinical investigation. In fact, many reference HAs and some in LATAM countries (Brazil, Colombia, Cuba, Ecuador, Mexico, Panama, and Peru) developed rules for performing CTs during this period. Some of these measures, such as reducing the burden of administrative procedures, designing decentralized trials, or using electronic informed consent, would be aligned with modernization purposes.
Other measures to facilitate the development of a drug, as well as the performance of innovative CTs [5], would be carrying out scientific advice meetings between HAs and sponsors. These meetings happen at several points of the drug development lifecycle and are useful to align the objectives to reach for both parties from early stages. These meetings are described in reference regulations but only in very few LATAM countries (Argentina, Brazil, and Mexico).
Additional reference points are the revisions of applicable international guidelines to ensure the quality and data integrity of CTs. The ICH E8 (CTs performance guidelines) is modified by ICH E8 (R1) [28], which includes details about quality for CTs, stakeholder engagement, CT design, and proportionate trial management. The ICH E6 (R2) (Good Clinical Practice guidelines) [29] will be updated by ICH E6 (R3), which is still in progress, taking into consideration features such as overarching principles, interventional CTs, and non-traditional interventional CTs. Reference HAs are ICH members, except TGA, so they implement these guidelines. However, most LATAM countries have not formally joined the ICH [30], so implementation of guidelines is not mandatory. This lack of compromise hinders adoption of all new concepts described in these guidelines.
Overall Discussion and Conclusions
Some HAs are already implementing changes to regulations or publishing guidance to consider new drug development designs and alternative registration procedures, although they are progressing at a different speed [31,32,33]. Even in the case of reference HAs (FDA, EMA, TGA, Health Canada, PMDA, and Swissmedic), the stages for implementation and acceptance of these novelties are not homogeneous. For LATAM countries, this situation is still more delayed. Therefore, we considered that an analysis of LATAM regulations and their comparison to reference HAs was necessary to determine measures to identify gaps and propose measures to close them. In this review and analysis, we have found a lack of acceptance of alternative registration pathways and innovative CT designs which motivates the call to LATAM stakeholders to follow the steps that reference HAs have already started and to adopt more simple and flexible procedures. One reason that hampers the implementation of these new procedures is the lack of a regular update of the drug registration and clinical research requirements in LATAM countries. More frequent reviews and updates of the regulations will facilitate the necessary changes for adopting new CT designs and more agile marketing approvals for a new drug or indication. In addition, implementing measures such as enhancing the adoption of the reliance pathway or accepting non-traditional CT phases as sufficient for registration would facilitate alignment with the current setting and modernization. In this sense, FDA is the most advanced agency of the reference HAs, so the key point could be to strengthen its role as a reference agency in these countries. In this way, by simplifying requirements and modernizing the drug development model, new drugs that aim to cover unmet medical needs will be able to reach patients earlier in LATAM countries.
In summary, regulations in LATAM countries must be changed and adapted to the newest regulatory standards to account for novelties and efficiently provide innovative drugs to patients. The path to be followed is adopting regulations from reference HAs, especially the FDA and EMA, as well as international guidelines (ICH). The key points to develop are included in Table 4.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Almufleh A, Joseph J. The time is now: role of pragmatic clinical trials in guiding response to global pandemics. Trials. 2021;22(1):229.
Harvin JA, Zarzaur BL, Nirula R, et al. Alternative clinical trial designs. Trauma Surg Acute Care Open. 2020;5(1):e000420.
Sharma A, Harrington RA, McClellan MB, et al. Using digital health technology to better generate evidence and deliver evidence-based care. J Am Coll Cardiol. 2018;71(23):2680–90.
Spreafico A, Hansen AR, Abdul Razak AR, et al. The future of clinical trial design in oncology. Cancer Discov. 2021;11(4):822–37.
European Federation of Pharmaceutical Industries and Associations. EFPIA Clinical Research Expert Group. Innovation in clinical trial design: a review of the clinical trial design landscape. 2020. https://www.efpia.eu/media/547507/efpia-position-paper-innovation-in-clinical-trial-design-white-paper.pdf
Dragalin V. Adaptive designs: terminology and classification. Drug Inf J. 2006;40:425–35.
Hirakawa A, Asano J, Sato H, et al. Master protocol trials in oncology: review and new trial designs. Contemp Clin Trials Commun. 2018;12:1–8.
Fountzilas E, Tsimberidou AM, Vo HH, et al. Clinical trial design in the era of precision medicine. Genome Med. 2022;14(1):101.
Mahlich J, Bartol A, Dheban S. Can adaptive clinical trials help to solve the productivity crisis of the pharmaceutical industry? A scenario analysis. Health Econ Rev. 2021;11(1):4.
Varnai P, Davé A, Farla K, et al. The evidence REVEAL study: exploring the use of real-world evidence and complex clinical trial design by the European pharmaceutical industry. Clin Pharmacol Ther. 2021;110(5):1180–9.
Clinical Trial Facilitation Coordinationg Group—Heads medicines agencies CTs recommendation paper on the initiation and conduct of complex clinical trials. 2019. https://www.hma.eu/fileadmin/dateien/Human_Medicines/01-About_HMA/Working_Groups/CTFG/2019_02_CTFG_Recommendation_paper_on_Complex_Clinical_Trials.pdf.
Health Canada. Clinical trials modernization: consultation paper 2021. https://www.canada.ca/en/health-canada/programs/consultation-clinical-trials-regulatory-modernization-initiative/document.html#a1.
Cruz Rivera S, Torlinska B, Marston E, et al. Advancing UK regulatory science strategy in the context of global regulation: a stakeholder survey. Ther Innov Regul Sci. 2021;55(4):646–55.
Bujar M, McAuslane N, Liberti L. The qualitative value of facilitated regulatory pathways in Europe, USA, and Japan: benefits, barriers to utilization, and suggested solutions. Pharmaceut Med. 2021;35(2):113–22.
Cox EM, Edmund AV, Kratz E, et al. Regulatory affairs 101: introduction to expedited regulatory pathways. Clin Transl Sci. 2020;13(3):451–61.
Swissmedic. Statement from global medicines regulators on the value of regulatory reliance 2021. https://www.swissmedic.ch/swissmedic/en/home/news/mitteilungen/icmra-konzept-regulatorischen-reliance.html#context-sidebar.
Durán CE, Cañás M, Urtasun MA, et al. Regulatory reliance to approve new medicinal products in Latin American and Caribbean countries. Rev Panam Salud Publica. 2021;45:e10.
Padua A, Partika L, Bonamici D, et al. Registration pathways to accelerate regulatory assessment of innovative medicines in Latin America. J Public Health Policy. 2020;41(4):481–95.
U.S. Food & Drug Administration. Fast track. 2018. https://www.fda.gov/patients/fast-track-breakthrough-therapy-accelerated-approval-priority-review/fast-track.
Hwang TJ, Darrow JJ, Kesselheim AS. The FDA’s expedited programs and clinical development times for novel therapeutics, 2012–2016. JAMA. 2017;318:2137–8.
World Health Organization WHO. Good reliance practices in regulatory 5 decision-making for medical products: 6 high-level principles and considerations. 2020. https://www.who.int/docs/default-source/medicines/norms-and-standards/current-projects/qas20-851-rev-1-good-reliance-practices.pdf?sfvrsn=ad1c54df_2.
US Food and Drug Administration. FDA approves pembrolizumab for advanced cervical cancer with disease progression during or after chemotherapy. 2018. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-pembrolizumab-advanced-cervical-cancer-disease-progression-during-or-after-chemotherapy#:~:text=On%20June%2012%2C%202018%2C%20the,by%20an%20FDA%2Dapproved%20test.
Pearson ADJ, Weiner SL, Adamson PC, et al. ACCELERATE—five years accelerating cancer drug development for children and adolescents. Eur J Cancer. 2022;166:145–64.
Krendyukov A, Singhvi S, Zabransky M. Value of adaptive trials and surrogate endpoints for clinical decision-making in rare cancers. Front Oncol. 2021;11:636561.
Nelson RM, Conklin LS, Komocsar WJ, et al. The role of master protocols in pediatric drug development. Ther Innov Regul Sci. 2022;56(6):895–902.
Karzai F, Madan RA, Dahut WL. The world of clinical trial development post COVID-19: lessons learned from a global pandemic. Clin Cancer Res. 2020;26(16):4198–200.
Vanderbeek AM, Bliss JM, Yin Z, et al. Implementation of platform trials in the COVID-19 pandemic: a rapid review. Contemp Clin Trials. 2022;112:106625.
ICH. General considerations for clinical studies E8(R1). 2021. https://database.ich.org/sites/default/files/ICH_E8-R1_Guideline_Step4_2021_1006.pdf.
ICH. Integrated addentum to ICH E6(R1): Guideline for good clinical practice E6(R2). 2016. https://database.ich.org/sites/default/files/E6_R2_Addendum.pdf.
ICH. Members & observers. 2022. https://www.ich.org/page/members-observers.
Hwang TJ, Kesselheim AS, Tibau A, et al. Clinical benefit and expedited approval of cancer drugs in the United States, European Union, Switzerland, Japan, Canada, and Australia. JCO Oncol Pract. 2022;18(9):e1522–32.
Burns L, Roux NL, Kalesnik-Orszulak R, et al. Real-world evidence for regulatory decision-making: guidance from around the world. Clin Ther. 2022;44(3):420–37.
Epps C, Bax R, Croker A, et al. Global regulatory and public health initiatives to advance pediatric drug development for rare diseases. Ther Innov Regul Sci. 2022;56(6):964–75.
EFPIA. The path to improved access to medicines through alternative registration pathways. 2017. 1–5. www.efpia.eu/media/288557/position-paper-reliance-and-expedited-pathways-in-emerging-markets_final_pdf.pdf.
European Medicines Agency. How scientific advice works. 2022. https://www.ema.europa.eu/en/human-regulatory/research-development/scientific-advice-protocol-assistance/how-scientific-advice-works#:~:text=During%20scientific%20advice%2C%20experts%20respond,identifies%20questions%20and%20possible%20solutions.
National Institute for Health and Care Research. Delivering complex and innovative trials. 2022. https://www.nihr.ac.uk/partners-and-industry/industry/run-your-study-in-the-nhs/complex-innovative-trials.htm.
Bogin V. Master protocols: new directions in drug discovery. Contemp Clin Trials Commun. 2020;18:100568.
Funding
The research for and writing of this article were conducted and funded by Roche. Urimara Argotti-Rodríguez (UA-R), Lada Leyens (LL), and Virginia Cozzi (VC) are employed by Roche. Roche provided support for the contribution of Carlos Lisbona (CL), Pilar López (PL), Sergio Alonso (SA), and Angel Nevado (AN).
Author information
Authors and Affiliations
Contributions
Substantial contributions to the conception, acquisition, analysis, and interpretation of data for the work: UA-R, LL, VC, CL, PL, SA, and AN. Drafting the work and revising it critically for important intellectual content: UA-R, LL, VC, CL, PL, SA, and AN. Final approval of the version to be published: UA-R, LL, and VC. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: UA-R, LL, VC, and CL.
Corresponding author
Ethics declarations
Conflict of interest
UA-R, LL, and VC are employees and stockholders of Roche.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Argotti, U., Leyens, L., Lisbona, C. et al. Comparison of the Latin America Regulation Landscape and International Reference Health Authorities to Hasten Drug Registration and Clinical Research Applications. Ther Innov Regul Sci 57, 1287–1297 (2023). https://doi.org/10.1007/s43441-023-00565-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43441-023-00565-7