Abstract
Purpose
To evaluate the utility of 5-Item Modified Frailty Index (mFI-5) as compared to chronological age in predicting outcomes of spinal osteotomy in Adult Spinal Deformity (ASD) patients.
Methods
Using Current Procedural and Terminology (CPT) codes, the American College of Surgeons National Surgery Quality Improvement Program (ACS-NSQIP) database was queried for adult patients undergoing spinal osteotomy from 2015 to 2019. Multivariate regression analysis was performed to evaluate the effect of baseline frailty status, measured by mFI-5 score, and chronological age on postoperative outcomes. Receiver-operating characteristic (ROC) curve analysis was performed to analyze the discriminative performance of age versus mFI-5.
Results
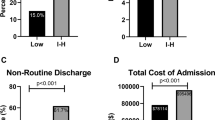
A total of 1,789 spinal osteotomy patients (median age 62 years) were included in the analysis. Among the patients assessed, 38.5% (n = 689) were pre-frail, 14.6% frail (n = 262), and 2.2% (n = 39) severely frail using the mFI-5. Based on the multivariate analysis, increasing frailty tier was associated with worsening outcomes, and higher odds ratios (OR) for poor outcomes were found for increasing frailty tiers as compared to age. Severe frailty was associated with the worst outcomes, e.g., unplanned readmission (OR 9.618, [95% CI 4.054–22.818], p < 0.001) and major complications (OR 5.172, [95% CI 2.271–11.783], p < 0.001). In the ROC curve analysis, mFI-5 score (AUC 0.838) demonstrated superior discriminative performance than age (AUC 0.601) for mortality.
Conclusions
The mFI5 frailty score was found to be a better predictor than age of worse postoperative outcomes in ASD patients. Incorporating frailty in preoperative risk stratification is recommended in ASD surgery.


Similar content being viewed by others
Data availability
All relevant data are included in the manuscript draft, tables, and figures. The raw data are available upon reasonable request from the corresponding author.
Code availability
Not applicable.
References
Glassman SD, Bridwell K, Dimar JR et al (2005) The impact of positive sagittal balance in adult spinal deformity. Spine 30:2024–2029
Soroceanu A, Burton DC, Diebo BG et al (2015) Impact of obesity on complications, infection, and patient-reported outcomes in adult spinal deformity surgery. J Neurosurg Spine 23:656–664
Smith C, Lamba N, Ou Z et al (2019) The prevalence of complications associated with lumbar and thoracic spinal deformity surgery in the elderly population: a meta-analysis. J Spine Surg 5:223–235
Safaee MM, Ames CP, Smith JS (2020) Epidemiology and socioeconomic trends in adult spinal deformity care. Neurosurgery 87:25–32
Indrakanti SS, Weber MH, Takemoto SK et al (2012) Value-based care in the management of spinal disorders: a systematic review of cost-utility analysis. Clin Orthop Relat Res 470:1106–1123
Chan V, Wilson JRF, Ravinsky R et al (2021) Frailty adversely affects outcomes of patients undergoing spine surgery: a systematic review. Spine J 21:988–1000
Kazim SF, Bowers CA, Lloyd RA et al (2021) Letter: frailty and outcomes of traumatic spinal cord injury. Neurosurgery. https://doi.org/10.1093/neuros/nyab210
Pazniokas J, Gandhi C, Theriault B et al (2021) The immense heterogeneity of frailty in neurosurgery: a systematic literature review. Neurosurg Rev 44:189–201
Puffer RC, Planchard R, Mallory GW et al (2016) Patient-specific factors affecting hospital costs in lumbar spine surgery. J Neurosurg Spine 24:1–6
Azizkhanian I, Alcantara R, Ballinger Z et al (2021) Spine surgery complexity score predicts outcomes in 671 consecutive spine surgery patients. Surg Neurol Int 12:206
Mitnitski AB, Mogilner AJ, Rockwood K (2001) Accumulation of deficits as a proxy measure of aging. ScientificWorldJournal 1:323–336
Wilson JRF (2021) The effect of age and frailty on clinical outcomes after surgery for degenerative cervical myelopathy. University of Toronto (Canada), Toronto
Hoogendijk EO, Afilalo J, Ensrud KE et al (2019) Frailty: implications for clinical practice and public health. Lancet 394:1365–1375
Wilkes JG, Evans JL, Prato BS et al (2019) Frailty cost: economic impact of frailty in the elective surgical patient. J Am Coll Surg 228:861–870
Hajek A, Bock J-O, Saum K-U et al (2017) Frailty and healthcare costs—longitudinal results of a prospective cohort study. Age Ageing 47:233–241
Chimukangara M, Helm MC, Frelich MJ et al (2017) A 5-item frailty index based on NSQIP data correlates with outcomes following paraesophageal hernia repair. Surg Endosc 31:2509–2519
Subramaniam S, Aalberg JJ, Soriano RP et al (2018) New 5-factor modified frailty index using american college of surgeons NSQIP data. J Am Coll Surg 226:173–81.e8
Traven SA, Reeves RA, Sekar MG et al (2019) New 5-factor modified frailty index predicts morbidity and mortality in primary hip and knee arthroplasty. J Arthroplasty 34:140–144
Dominguez JF, Shah S, Ampie L et al (2021) Spinal epidural abscess patients have higher modified frailty indexes than back pain patients on emergency room presentation: a single-center retrospective case-control study. World Neurosurg 152:e610–e616
Phen HM, Jones C, Kravets VG et al (2021) Impact of frailty and malnutrition on outcomes after surgical fixation of lower extremity fractures in young patients. J Orthop Trauma 35:e126–e133
Ali R, Schwalb JM, Nerenz DR et al (2016) Use of the modified frailty index to predict 30-day morbidity and mortality from spine surgery. J Neurosurg Spine 25:537–541
Dicpinigaitis AJ, Kazim SF, Schmidt MH et al (2021) Association of baseline frailty status and age with postoperative morbidity and mortality following intracranial meningioma resection. J Neurooncol 155:45–52
McIntyre M, Gandhi C, Dragonette J et al (2020) Increasing frailty predicts worse outcomes and increased complications after angiogram-negative subarachnoid hemorrhages. World Neurosurg 134:e181–e188
Dicpinigaitis AJ, Kalakoti P, Schmidt M et al (2021) Associations of baseline frailty status and age with outcomes in patients undergoing vestibular schwannoma resection. JAMA Otolaryngol Head Neck Surg 147:608–614
Huffman KM, Cohen ME, Ko CY et al (2015) A comprehensive evaluation of statistical reliability in ACS NSQIP profiling models. Ann Surg 261:1108–1113
Shiloach M, Frencher SK Jr, Steeger JE et al (2010) Toward robust information: data quality and inter-rater reliability in the American college of surgeons national surgical quality improvement program. J Am Coll Surg 210:6–16
Weaver DJ, Malik AT, Jain N et al (2019) The modified 5-item frailty index: a concise and useful tool for assessing the impact of frailty on postoperative morbidity following elective posterior lumbar fusions. World Neurosurg. https://doi.org/10.1016/j.wneu.2018.12.168
McIntyre MK, Gandhi C, Dragonette J et al (2020) A comparison of frailty indices in predicting length of inpatient stay and discharge destination following angiogram-negative subarachnoid hemorrhage. Br J Neurosurg 35:1–6
Kim MG, Gandhi C, Azizkhanian I et al (2020) Frailty and spontaneous intracerebral hemorrhage: does the modified frailty index predict mortality? Clin Neurol Neurosurg 194:105816
Panayi AC, Haug V, Kauke-Navarro M et al (2021) The modified 5-item frailty index is a predictor of perioperative risk in head and neck microvascular reconstruction: an analysis of 3795 cases. Am J Otolaryngol 42:103121
Kesserwan M, Bergin B, Trivedi A et al (2021) Assessment of frailty in predicting surgical outcomes in patients with chronic subdural hematomas: retrospective chart review. World Neurosurg 146:e168–e174
Christopher E, Poon MTC, Glancz LJ et al (2019) Outcomes following surgery in subgroups of comatose and very elderly patients with chronic subdural hematoma. Neurosurg Rev 42:427–431
Passias PG, Brown AE, Bortz C et al (2021) A risk−benefit analysis of increasing surgical invasiveness relative to frailty status in adult spinal deformity surgery. Spine 46:1087–1096
Yagi M, Hosogane N, Fujita N et al (2019) Predictive model for major complications 2 years after corrective spine surgery for adult spinal deformity. Eur Spine J 28:180–187
Özyemişci TÖ (2020) Rehabilitation in adult spinal deformity. Turk J Phys Med Rehabil 66:231–243
Mohamed B, Ramachandran R, Rabai F et al (2021) Frailty assessment and prehabilitation before complex spine surgery in patients with degenerative spine disease. J Neurosurg Anesthesiol. https://doi.org/10.1097/ana.0000000000000787. (Publish Ahead of Print)
Funding
The authors did not receive any specific Grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Contributed to conception/design of work: OHT, JV, SFK, RT, KR, MC, DA-C, KLC, SV, JFD, RGM, MHS, CAB. Analysis/interpretation of data: OHT, JV, SFK, RT, KR, MC, DA-C, KLC, SV, MHS, CAB. Drafted the work: OHT, JV, SFK, RT, KR, MC, DA-C, KLC, SV, CAB. Critically revised the work: SFK, JFD, RGM, MHS, CAB. Oversaw the project: CAB, MHS. Approved version to be published: OHT, JV, SFK, RT, KR, MC, DA-C, KLC, SV, JFD, RGM, MHS, CAB. Agrees to be accountable for all aspects of the work: OHT, JV, SFK, RT, KR, MC, DA-C, KLC, SV, JFD, RGM, MHS, CAB.
Corresponding author
Ethics declarations
Conflict of interest
The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Ethical approval
The present study was performed under the data user agreement (DUA) of the ACS with the University of New Mexico (UNM) and was approved by the Institutional Review Board of UNM School of Medicine (Study ID 21-315).
Consent to participate
Given the deidentified nature of the information in NSQIP database, patient consent was neither sought nor required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tarawneh, O.H., Vellek, J., Kazim, S.F. et al. The 5-item modified frailty index predicts spinal osteotomy outcomes better than age in adult spinal deformity patients: an ACS − NSQIP analysis. Spine Deform 11, 1189–1197 (2023). https://doi.org/10.1007/s43390-023-00712-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-023-00712-y