Abstract
Purpose
Traditionally, 2-year follow-up data have been the established standard for reporting clinical outcomes following spinal deformity surgery. However, previous studies indicate that 2-year follow-up does not represent long-term outcomes. Currently, there is no clear data that demonstrate a difference in outcomes between the 1 and 2 years postoperative time-periods following posterior spinal fusions (PSF) for adolescent idiopathic scoliosis (AIS).
Methods
A multi-center, prospective database was queried for AIS patients treated with PSF. Clinical outcome scores, assessed by SRS-22, coronal and sagittal radiographic parameters were assessed at time periods: 6 months, 1 year, and 2 years post operatively. Complications and reoperation rates were also assessed. Statistical analysis compared outcomes variables across time-points to assess for significant differences.
Results
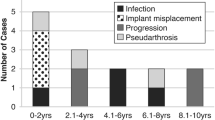
694 patients (82.6% female, mean age at surgery 14.9 ± 2.13 years) were identified. Between post-operative year 1 and 2, significant difference in SRS-22 domain scores were present for function domain (4.5 vs. 4.6; p < 0.001), mental health domain (4.3 vs. 4.2; p < 0.001), and total domain score (4.4 vs. 4.4; p = 0.03) but were below the minimal clinically important difference threshold. New complication development was significantly higher within the first year following surgery than the 1–2 year follow-up period (p < 0.001) with greater complication severity within the 0–1 year follow-up period (P = 0.03).
Conclusion
There are no clinically important changes in SRS-22 domain scores between 1 and 2 years following PSF for AIS, with higher complications in the first year following PSF. Two-year follow-up data provide little added clinical information while under-estimating the cumulative complication and reoperation rates at long-term follow-up.


Similar content being viewed by others
References
Weinstein SL, Ponseti IV (1983) Curve progression in idiopathic scoliosis. J Bone Joint Surg Am 65(4):447–455
Asher M, Min Lai S, Burton D, Manna B (2003) Scoliosis research society-22 patient questionnaire: responsiveness to change associated with surgical treatment. Spine (Phila Pa 1976) 28(1):70–73
Howard A, Donaldson S, Hedden D, Stephens D, Alman B, Wright J (2007) Improvement in quality of life following surgery for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 32(24):2715–2718
Pellegrino LN, Avanzi O (2014) Prospective evaluation of quality of life in adolescent idiopathic scoliosis before and after surgery. J Spinal Disord Tech 27(8):409–414
Smucny M, Lubicky JP, Sanders JO, Carreon LY, Diab M (2011) Patient self-assessment of appearance is improved more by all pedicle screw than by hybrid constructs in surgical treatment of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 36(3):248–254
Louer C Jr, Yaszay B, Cross M et al (2019) Ten-year outcomes of selective fusions for adolescent idiopathic scoliosis. J Bone Joint Surg Am 101(9):761–770
Newton PO, Ohashi M, Bastrom TP et al (2020) Prospective 10-year follow-up assessment of spinal fusions for thoracic AIS: radiographic and clinical outcomes. Spine Deform 8(1):57–66
Mac-Thiong JM, Remondino R, Joncas J, Parent S, Labelle H (2019) Long-term follow-up after surgical treatment of adolescent idiopathic scoliosis using high-density pedicle screw constructs: Is 5-year routine visit required? Eur Spine J 28(6):1296–1300
Ahmed SI, Bastrom TP, Yaszay B, Newton PO (2017) 5-Year reoperation risk and causes for revision after idiopathic scoliosis surgery. Spine (Phila Pa 1976) 42(13):999–1005
Guissé NF, Stone JD, Keil LG et al (2021) Modified Clavien-Dindo-sink classification system for adolescent idiopathic scoliosis. Spine Deform. https://doi.org/10.1007/s43390-021-00394-4
Carreon LY, Sanders JO, Diab M, Sucato DJ, Sturm PF, Glassman SD (2010) The minimum clinically important difference in Scoliosis Research Society-22 Appearance, Activity, And Pain domains after surgical correction of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 35(23):2079–2083
Kelly MP, Lenke LG, Sponseller PD et al (2019) The minimum detectable measurement difference for the Scoliosis Research Society-22r in adolescent idiopathic scoliosis: a comparison with the minimum clinically important difference. Spine J 19(8):1319–1323
Hwang SW, Samdani AF, Marks M et al (2013) Five-year clinical and radiographic outcomes using pedicle screw only constructs in the treatment of adolescent idiopathic scoliosis. Eur Spine J 22(6):1292–1299
Yilmaz G, Borkhuu B, Dhawale AA et al (2012) Comparative analysis of hook, hybrid, and pedicle screw instrumentation in the posterior treatment of adolescent idiopathic scoliosis. J Pediatr Orthop 32(5):490–499
Bastrom TP, Bartley CE, Newton PO (2019) Patient-Reported SRS-24 Outcomes Scores After Surgery for Adolescent Idiopathic Scoliosis Have Improved Since the New Millennium. Spine Deform 7(6):917–922
Hamzaoglu A, Karadereler S, Kahraman S et al (2021) Clinical, radiological and HRQoL outcomes after selective thoracic fusion with minimum 15-year follow-up. Spine Deform 9(5):1323–1331
Hughes J, Yaszay B, Bastrom TP et al (2021) Long-term patient perception following surgery for adolescent idiopathic scoliosis if dissatisfied at 2-year follow-up. Spine (Phila Pa 1976) 46(8):507–511
Sanders JO, Carreon LY, Sucato DJ, Sturm PF, Diab M (2010) Preoperative and perioperative factors effect on adolescent idiopathic scoliosis surgical outcomes. Spine (Phila Pa 1976) 35(20):1867–1871
Mignemi M, Tran D, Ramo B, Richards BS (2018) Repeat surgical interventions following “Definitive” instrumentation and fusion for idiopathic scoliosis: 25-year update. Spine Deform 6(4):409–416
Roye BD, Matsumoto H, Fano AN et al (2021) Distal adding-on in adolescent idiopathic scoliosis results in diminished health-related quality of life at 10 years following posterior spinal fusion. Spine Deform. https://doi.org/10.1007/s43390-021-00432-1
Weinstein SL, Dolan LA, Spratt KF, Peterson KK, Spoonamore MJ, Ponseti IV (2003) Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA 289(5):559–567
Hwang SW, Pendleton C, Samdani AF et al (2020) Preoperative SRS pain score is the primary predictor of postoperative pain after surgery for adolescent idiopathic scoliosis: an observational retrospective study of pain outcomes from a registry of 1744 patients with a mean follow-up of 3.4 years. Eur Spine J 29(4):754–760
Helenius L, Diarbakerli E, Grauers A et al (2019) Back pain and quality of life after surgical treatment for adolescent idiopathic scoliosis at 5-year follow-up: comparison with healthy controls and patients with untreated idiopathic scoliosis. J Bone Joint Surg Am 101(16):1460–1466
Bastrom TP, Marks MC, Yaszay B, Newton PO (2013) Prevalence of postoperative pain in adolescent idiopathic scoliosis and the association with preoperative pain. Spine (Phila Pa 1976) 38(21):1848–1852
Cook S, Asher M, Lai SM, Shobe J (2000) Reoperation after primary posterior instrumentation and fusion for idiopathic scoliosis Toward defining late operative site pain of unknown cause. Spine (Phila Pa 1976) 25(4):463–468
Ramo BA, Richards BS (2012) Repeat surgical interventions following “definitive” instrumentation and fusion for idiopathic scoliosis: five-year update on a previously published cohort. Spine (Phila Pa 1976) 37(14):1211–1217
Samdani AF, Belin EJ, Bennett JT et al (2013) Unplanned return to the operating room in patients with adolescent idiopathic scoliosis: are we doing better with pedicle screws? Spine (Phila Pa 1976) 38(21):1842–1847
Lykissas MG, Jain VV, Nathan ST et al (2013) Mid- to long-term outcomes in adolescent idiopathic scoliosis after instrumented posterior spinal fusion: a meta-analysis. Spine (Phila Pa 1976) 38(2):E113-119
Acknowledgements
Harms Study Group Investigators: Aaron Buckland, MD: New York University. Amer Samdani, MD; Joshua Pahys, MD; and Steven Hwang, MD: Shriners Hospitals for Children—Philadelphia. Amit Jain, MD; and Paul Sponseller, MD: Johns Hopkins Hospital. Baron Lonner, MD: Mount Sinai Hospital. Benjamin Roye, MD; Larry Lenke, MD; Michael Vitale, MD; and Ron Lehman, MD: Columbia University. Burt Yaszay, MD; Peter Newton, MD; and Vidyadhar Upasani, MD: Rady Children's Hospital. Chris Reilly, MD; and Firoz Miyanji, MD: BC Children's Hospital. Daniel Hedequist, MD; and Michael Glotzbecker, MD: Boston Children's Hospital. Daniel Sucato, MD: Texas Scottish Rite Hospital. David Clements, MD: Cooper Bone & Joint Institute New Jersey. Harry Shufflebarger, MD; Stephen George, MD; and Tom Errico, MD: Nicklaus Children's Hospital. Jack Flynn, MD; and Patrick Cahill, MD: Children's Hospital of Philadelphia. Jahangir Asghar, MD: Cantor Spine Institute. Jean Marc Mac-Thiong, MD; and Stefan Parent, MD: CHU Sainte-Justine. Juergen Harms, MD: ETHIANUM Klinik, Heidelberg, Germany. Keith Bachmann, MD; and Mark Abel, MD: University of Virginia. Michael Kelly, MD; and Munish Gupta, MD: Washington University. Michelle Marks, PT, MA: Setting Scoliosis Straight Foundation. Nicholas Fletcher, MD: Emory University. Peter Gabos, MD; and Suken Shah, MD: Nemours/Alfred I. duPont Hospital for Children. Peter Sturm, MD: Cincinnati Children's Hospital. Randal Betz, MD: Institute for Spine & Scoliosis.
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Consortia
Contributions
KAS: study design, data analysis, data interpretation, manuscript drafting, manuscript approval, accountable. KO: study design, data analysis, manuscript approval, accountable. TPB: study design, data analysis, manuscript editing, manuscript approval, accountable. PON: study design, data interpretation, manuscript editing, manuscript approval, accountable. NDF: study design, data analysis, manuscript editing, manuscript approval, accountable.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Shaw is a committee member for NASS and AAOS; Dr. Orland reports nothing to disclose; Ms. Bastrom reports nothing to disclose; Dr. Newton is a consultant for Depuy, Globus Medical, Mirus, Pacira, Stryker, receives IP royalties from Depuy and Stryker, is a paid speaker for Medtronic, receives publishing royalties from Thieme, receives research support from Depuy, EOS Imaging, Medtronic, Nuvasive, Stryker, and Zimmer Biomet, is a committee member for Harms Study Group, International Pediatric Orthopedic Think Tank, Setting Scoliosis Straight Foundation; Dr. Fletcher is a consultant for Medtronic, a paid speaker for Zimmer, Nuvasive, Orthopediatrics, and Medtronic, is a board member for SRS and POSNA and serves on the editorial board for JPOSNA. All authors read and approved the final manuscript.
Ethical approval
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shaw, K.A., Orland, K., Bastrom, T.P. et al. 1- vs. 2-year follow-up after posterior spinal fusion for AIS: what additional information is gained?. Spine Deform 10, 1359–1366 (2022). https://doi.org/10.1007/s43390-022-00555-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-022-00555-z