Abstract
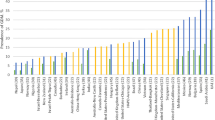
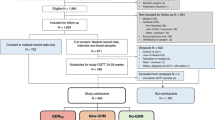
Over the years, several international guidelines have been developed by specialist organizations for the diagnosis of gestational diabetes mellitus (GDM). However, these guidelines vary and lack consensus on what level of glycemia defines GDM and worryingly, there is now evidence of over- or- under-diagnosis of women with GDM by current criteria. Towards this end, the National Priorities Research Program (NPRP) funded a program of research aimed at elucidating the problem with GDM diagnosis. It was determined, on completion of the project, that the solution required diagnosis of graded levels of dysglycemia in pregnancy and not just a diagnosis of presence or absence of GDM. A new diagnostic criterion (called the NPRP criterion) was created based on a single numerical summary of the three readings from the oral glucose tolerance test (GTT) that diagnosed women in pregnancy into four levels: normal, impaired, GDM and high risk GDM. This paper now examines existing GDM criteria vis-à-vis the NPRP criterion. It is noted that no significant change has happened over the years for existing criteria except for a gradual reduction in the threshold values of individual time-points or the number of time points, bringing us towards over-diagnosis of GDM in pregnancy. The new criterion unifies all readings from the GTT into one numerical value and, because it results in four levels of glycemia, represents a new way forwards for GDM diagnosis and can potentially reduce the rates of under diagnosis and over diagnosis of GDM.


Similar content being viewed by others
Data Availability
All data used in this paper are available from the corresponding author in de-identified format on reasonable request.
Abbreviations
- NDDG:
-
National Diabetes Data Group, 1979
- C&C:
-
Carpenter and Coustan, 1982
- ADIPS1998AU:
-
Australasian Diabetes in Pregnancy Society – Australia
- ADIPS1998NZ (NZ 2014):
-
Australasian Diabetes in Pregnancy Society – New Zealand
- WHO1998:
-
World Health Organization
- ADA2004:
-
American Diabetes Association
- ADA2006:
-
American Diabetes Association
- IADPSG:
-
International Association of Diabetes and Pregnancy Study Group (OR 1.75)
- ADA2011:
-
American Diabetes Association
- ADIPS2011:
-
Australasian Diabetes in Pregnancy Society
- ACOG:
-
American College of Obstetricians and Gynecologists, 2013
- WHO2013:
-
World Health Organization
- NICE:
-
National Institute for Health and Care Excellence, 2015
- CDA:
-
Canadian Diabetes Association, 2018
- NPRP:
-
National Priorities Research Program, 2022
References
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 2. Classification and Diagnosis of Diabetes: Standards of Care in Diabetes-2023. Diabetes Care. 2023;46(Suppl 1):S19–s40. https://doi.org/10.2337/dc23-S002.
Ratner RE, Christophi CA, Metzger BE, Dabelea D, Bennett PH, Pi-Sunyer X, et al. Prevention of diabetes in women with a history of gestational diabetes: effects of metformin and lifestyle interventions. J Clin Endocrinol Metab. 2008;93(12):4774–9.
Bhat M, Ramesha KN, Sarma SP, Sangeetha Menon SCV. Determinants of gestational diabetes mellitus: A case control study in a district tertiary care hospital in south India. Int J Diabetes Dev Ctries. 2010;30(2):91.
Cordero L, Treuer SH, Landon MB, Gabbe SG. Management of infants of diabetic mothers. Arch Pediatr Adolesc Med. 1998;152(3):249–54.
Fadl HE, Östlund IKM, Magnuson AFK, Hanson USB. Maternal and neonatal outcomes and time trends of gestational diabetes mellitus in Sweden from 1991 to 2003. Diabet Med. 2010;27(4):436–41.
Ju H, Rumbold AR, Willson KJ, Crowther CA. Borderline gestational diabetes mellitus and pregnancy outcomes. BMC Pregnancy Childbirth. 2008;8(1):1–7.
Metzger BE, Contreras M, Sacks DA, Watson W, Dooley SL, Foderaro M, et al. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008;358(19):1991–2002.
Shand AW, Bell JC, McElduff A, Morris J, Roberts CL. Outcomes of pregnancies in women with pre-gestational diabetes mellitus and gestational diabetes mellitus; a population-based study in New South Wales, Australia, 1998–2002. Diabet Med. 2008;25(6):708–15.
Farrar D. Hyperglycemia in pregnancy: prevalence, impact, and management challenges. Int J Women’s Health. 2016;8:519.
Plows JF, Stanley JL, Baker PN, Reynolds CM, Vickers MH. The pathophysiology of gestational diabetes mellitus. Int J Mol Sci. 2018;19(11). https://doi.org/10.3390/ijms19113342.
Landon MB, Spong CY, Thom E, Carpenter MW, Ramin SM, Casey B, et al. A multicenter, randomized trial of treatment for mild gestational diabetes. N Engl J Med. 2009;361(14):1339–48. https://doi.org/10.1056/NEJMoa0902430.
Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med. 2005;352(24):2477–86. https://doi.org/10.1056/NEJMoa042973.
ACOG. ACOG Committee opinion number 315, September 2005. Obesity in pregnancy. Obstetrics and Gynecology. 2005;106(3):671–5.
ACOG. Gestational diabetes mellitus. Practice Bulletin No. 137. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2013;122(2):406–16.
Bashir M, Baagar K, Naem E, Elkhatib F, Alshaybani N, Konje JC, et al. Pregnancy outcomes of early detected gestational diabetes: a retrospective comparison cohort study, Qatar. BMJ Open. 2019;9(2):e023612.
Hillier TA, Pedula KL, Ogasawara KK, Vesco KK, Oshiro C, Van Marter JL. Impact of earlier gestational diabetes screening for pregnant people with obesity on maternal and perinatal outcomes. J Perinat Med. 2022;50(8):1036–44.
Hughes RCE, Rowan J, Williman J. Prediabetes in pregnancy, can early intervention improve outcomes? A feasibility study for a parallel randomised clinical trial. BMJ Open. 2018;8(3):e018493.
Simmons D, Nema J, Parton C, Vizza L, Robertson A, Rajagopal R, et al. The treatment of booking gestational diabetes mellitus (TOBOGM) pilot randomised controlled trial. BMC Pregnancy Childbirth. 2018;18:1–8.
Vinter CA, Tanvig MH, Christensen MH, Ovesen PG, Jørgensen JS, Andersen MS, et al. Lifestyle intervention in Danish obese pregnant women with early gestational diabetes mellitus according to WHO 2013 criteria does not change pregnancy outcomes: results from the LiP (Lifestyle in Pregnancy) study. Diabetes Care. 2018;41(10):2079–85.
Enakpene CA, Della Torre M, DiGiovanni L, Wojtowycz M, Hasan A, Sutherland M, et al. Randomization of early diabetes screening among obese pregnant women (REDSOAP study). Am J Obstet Gynecol. 2022;226(1):S42.
Rodriguez A, Delgado A, Pressman K, Louis J. Early gestational diabetes screening in women at risk for gestational diabetes: a randomized controlled trial. Am J Obstet Gynecol. 2022;226(1):S41.
Harper LM, Jauk V, Longo S, Biggio JR, Szychowski JM, Tita AT. Early gestational diabetes screening in obese women: a randomized controlled trial. Am J Obstet Gynecol. 2020;222(5):495.e1–8. https://doi.org/10.1016/j.ajog.2019.12.021.
Osmundson SS, Norton ME, El-Sayed YY, Carter S, Faig JC, Kitzmiller JL. Early screening and treatment of women with prediabetes: a randomized controlled trial. Am J Perinatol. 2016;33(02):172–9.
Roeder HA, Moore TR, Wolfson MT, Gamst AC, Ramos GA. Treating hyperglycemia in early pregnancy: a randomized controlled trial. Am J Obstet Gynecol MFM. 2019;1(1):33–41.
Greene MF. Early versus Second-Trimester Screening and Treatment for Diabetes in Pregnancy. N Engl J Med. 2023;388(23):2193–4. https://doi.org/10.1056/NEJMe2304543.
Simmons D, Immanuel J, Hague WM, Teede H, Nolan CJ, Peek MJ, et al. Treatment of Gestational Diabetes Mellitus Diagnosed Early in Pregnancy. N Engl J Med. 2023;388(23):2132–44. https://doi.org/10.1056/NEJMoa2214956.
Chaves C, Cunha FM, Martinho M, Garrido S, Silva-Vieira M, Estevinho C, et al. First trimester fasting glucose and glycated haemoglobin cut-offs associated with abnormal glucose homeostasis in the post-partum reclassification in women with hyperglycaemia in pregnancy. Arch Gynecol Obstet. 2022;305(2):475–82. https://doi.org/10.1007/s00404-021-06107-6.
Riskin-Mashiah S, Damti A, Younes G, Auslander R. Normal fasting plasma glucose levels during pregnancy: a hospital-based study. J Perinat Med 2011;39(2):209–11. https://doi.org/10.1515/jpm.2010.142.
Bilous RW, Jacklin PB, Maresh MJ, Sacks DA. Resolving the Gestational Diabetes Diagnosis Conundrum: The Need for a Randomized Controlled Trial of Treatment. Diabetes Care. 2021;44(4):858–64.
Hartling L, Dryden DM, Guthrie A, Muise M, Vandermeer B, Aktary WM, et al. Screening and diagnosing gestational diabetes mellitus. Evid Rep Technol Assess. 2012;210:1.
Metzger BE, Gabbe SG, Persson B, Buchanan TA, Catalano PA, Damm P, et al. International Association of Diabetes and Pregnancy Study Groups Consensus Panel International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33(3):676–82.
Carpenter MW, Coustan DR. Criteria for screening tests for gestational diabetes. Am J Obstet Gynecol. 1982;144(7):768–73.
Bashir M, Ibrahim I, Eltaher F, Beer S, Baagar K, Aboulfotouh M, et al. Screening pregnant women in a high-risk population with WHO-2013 or NICE diagnostic criteria does not affect the prevalence of gestational diabetes. Sci Rep. 2021;11(1):1–7.
WHO. Definition, diagnosis and classification of diabetes mellitus and its complications: report of a WHO consultation. Part 1, Diagnosis and classification of diabetes mellitus. World Health Organization; 1999.
WHO. Diagnostic criteria and classification of hyperglycaemia first detected in pregnancy. World Health Organization; 2013.
ADA. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2006;29(Suppl 1):S43–8.
ADA. Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2011;34(Supplement 1):S62. https://doi.org/10.2337/dc11-S062.
ADA. Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2004;27(suppl 1):s5. https://doi.org/10.2337/diacare.27.2007.S5.
NICE. Diabetes in pregnancy: management from preconception to the postnatal period (NG3). 2015. https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwjGrPmE0b7uAhXUSH0KHd6kAqEQFjABegQIAhAC&url=https%3A%2F%2Fwww.nice.org.uk%2Fguidance%2Fng3%2Fresources%2Fdiabetes-in-pregnancy-management-from-preconception-to-the-postnatal-period-pdf-51038446021&usg=AOvVaw0cD1ULLOvNxGDpNWM9nnRm. Accessed 2020.
NDDG. Classification and diagnosis of diabetes mellitus and other categories of glucose intolerance. Diabetes. 1979;28(12):1039–57.
Hoffman L, Nolan C, Wilson JD, Oats JJN, Simmons D. Gestational diabetes mellitus - management guidelines: The Australasian Diabetes in Pregnancy Society. Med J Aust. 1998;169(2):93–7. https://doi.org/10.5694/j.1326-5377.1998.tb140192.x.
Thompson D, Berger H, Feig D, Gagnon R, Kader T, Keely E, et al. Diabetes and pregnancy. Can J Diabetes. 2013;37(Suppl 1):S168–83. https://doi.org/10.1016/j.jcjd.2013.01.044.
O’Sullivan JB, Mahan CM. Criteria for the oral glucose tolerance test in pregnancy. Diabetes. 1964;13:278–85.
Doi SAR, Bashir M, Sheehan MT, Onitilo AA, Chivese T, Ibrahim IM, et al. Unifying the diagnosis of gestational diabetes mellitus: Introducing the NPRP criteria. Prim Care Diabetes. 2022;16(1):96–101.
Badran S, Doi S, Hammouda A, Musa O, Habib A. Validation of Doi’s weighted average glucose as a measure of post-load glucose excursion for clinical use. Biomol Biomed 2023;23(5):914–19. https://doi.org/10.17305/bb.2022.8807.
Soonthornpun K, Soonthornpun S, Thamprasit A, Aksonteing J. Differences in postload plasma glucose levels between 100-g and 75-g oral glucose tolerance tests in normal pregnant women: a potential role of early insulin secretion. J Med Assoc Thail. 2008;91(3):277–81.
Soonthornpun S, Soonthornpun K, Aksonteing J, Thamprasit A. A comparison between a 75-g and 100-g oral glucose tolerance test in pregnant women. Int J Gynaecol Obstet. 2003;81(2):169–73.
Gupta Y, Kalra B, Baruah MP, Singla R, Kalra S. Updated guidelines on screening for gestational diabetes. Int J Women’s Health. 2015;7:539–50. https://doi.org/10.2147/IJWH.S82046.
Shirazian N, Mahboubi M, Roya E, Yousefi-Nooraie R, Fazel-Sarjuei Z, Sedighpour N, et al. Comparison of different diagnostic criteria for gestational diabetes mellitus based on the 75-g oral glucose tolerance test: a cohort study. Endocr Pract. 2008;14(3):312–7.
Hillier TA, Pedula KL, Ogasawara KK, Vesco KK, Oshiro CES, Lubarsky SL, et al. A Pragmatic, Randomized Clinical Trial of Gestational Diabetes Screening. N Engl J Med. 2021;384(10):895–904. https://doi.org/10.1056/NEJMoa2026028.
Crowther CA, Samuel D, McCowan LME, Edlin R, Tran T, McKinlay CJ. Lower versus higher glycemic criteria for diagnosis of gestational diabetes. N Engl J Med. 2022;387(7):587–98.
McIntyre HD, Jensen DM, Jensen RC, Kyhl HB, Jensen TK, Glintborg D, et al. Gestational diabetes mellitus: does one size fit all? A challenge to uniform worldwide diagnostic thresholds. Diabetes Care. 2018;41(7):1339–42.
Meek CL, Lewis HB, Patient C, Murphy HR, Simmons D. Diagnosis of gestational diabetes mellitus: falling through the net. Diabetologia. 2015;58(9):2003–12.
Casey B. Gestational Diabetes—On Broadening the Diagnosis. N Engl J Med. 2021;384(10):965–6.
Dall TM, Yang W, Halder P, Pang B, Massoudi M, Wintfeld N, et al. The economic burden of elevated blood glucose levels in 2012: diagnosed and undiagnosed diabetes, gestational diabetes mellitus, and prediabetes. Diabetes Care. 2014;37(12):3172–9.
Keag OE, Norman JE, Stock SJ. Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: Systematic review and meta-analysis. PLoS Med. 2018;15(1):e1002494.
Xu T, Dainelli L, Yu K, Ma L, Zolezzi IS, Detzel P, et al. The short-term health and economic burden of gestational diabetes mellitus in China: a modelling study. BMJ Open. 2017;7(12):e018893.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
The multidisciplinary team of authors consisting of endocrinologists and epidemiologists all contributed to this article and critically revised and approved the final manuscript for submission. The corresponding author is the guarantor of the data reported herein.
Corresponding author
Ethics declarations
Conflict of Interest
Authors declare no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Musa, O.A.H., Syed, A., Khatib, M.A. et al. Time to Move Beyond a Binary Criterion for Gestational Diabetes?. Reprod. Sci. (2024). https://doi.org/10.1007/s43032-024-01514-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43032-024-01514-x