Abstract
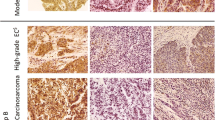
The objective of this study was to investigate proliferation, apoptosis, and antiapoptotic molecule expression in endometrial cells of reproductive-aged women with and without type II diabetes mellitus (T2D). In this case-control study, a total of 80 endometrial tissue specimens from reproductive-aged women (35 in the proliferative phase and 45 in the secretory phase) were examined. The age and body mass index (BMI) were matched between the groups. Formalin-fixed and paraffin-embedded endometrial tissue samples were used for immunohistochemistry analysis. The presence of proliferation was evaluated with Ki-67 expression, antiapoptotic function of cells was evaluated with Bcl-2 expression, and apoptosis was evaluated with terminal deoxynucleotidyl transferase (TUNEL) immunoreactivity in both the glandular epithelium and stroma of endometrial tissue samples from women with and without T2D. Ki-67 expression in the glandular epithelium and Bcl-2 expression in both the glandular epithelium and stroma were significantly higher in endometrial tissue samples of women in the T2D group than the control group (p = 0.0008, p = 0.0022, and p = 0.0261, respectively). TUNEL immunoreactivity was significantly lower in the glandular epithelium of women in the T2D group than the control group (p = 0.0001). Glandular Ki-67 expression correlated positively with BMI, use of insulin, and hemoglobin A1c level (p = 0.0034, p = 0.0154, and p = 0.0011, respectively). Glandular Bcl-2 expression correlated positively with BMI and duration of T2D (p = 0.0090 and p = 0.0109, respectively). Stromal Bcl-2 expression correlated positively with duration of T2D (p = 0.0069). TUNEL immunoreactivity in the glandular epithelium correlated negatively with duration of T2D (p = 0.0340) and positively with the use of oral antidiabetic agents (p = 0.0226). Compared to age and BMI-matched controls, women with T2D experienced increased cell proliferation and decreased apoptosis in the glandular epithelium and increased antiapoptotic function in both the glandular epithelium and stromal cells. High BMI values in women with diabetes seemed to contribute to increased cell proliferation and increased antiapoptotic function in the glandular epithelium but not the stromal cells.




Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- ASCVD:
-
atherosclerotic cardiovascular diseases
- Ki-67:
-
MKI67
- Bcl-2:
-
B cell leukemia/lymphoma 2
- T2D:
-
type II diabetes mellitus
- BMI:
-
body mass index
- TUNEL:
-
terminal dUTP nick-end labeling
- ADA:
-
American Diabetes Association
- HbA1c:
-
hemoglobin A1c
- EC:
-
endometrial cancer
- DM:
-
diabetes mellitus
- SD:
-
standard deviation
- FFA:
-
plasma free fatty acid
- EP:
-
early proliferative
- LP:
-
late proliferative
- ES:
-
early secretory
- MS:
-
mid secretory
- LS:
-
late secretory
- IGFBP1:
-
insulin-like growth factor binding protein 1
- ROS:
-
reactive oxygen species
References
Brooks RA, Fleming GF, Lastra RR, Lee NK, Moroney JW, Son CH, et al. Current recommendations and recent progress in endometrial cancer. CA Cancer J Clin. 2019;69:258–79. https://doi.org/10.3322/caac.21561.
Constantine GD, Kessler G, Graham S, Goldstein SR. Increased incidence of endometrial cancer following the Women’s Health Initiative: an assessment of risk factors. J Women's Health. 2019;28:237–43. https://doi.org/10.1089/jwh.2018.6956.
Felix AS, Weissfeld JL, Stone RA, Bowser R, Chivukula M, Edwards RP, et al. Factors associated with type I and type II endometrial cancer. Cancer Causes Control. 2010;21:1851–6. https://doi.org/10.1007/s10552-010-9612-8.
Lindemann K, Vatten LJ, Ellstrøm-Engh M, Eskild A. Body mass, diabetes and smoking, and endometrial cancer risk: a follow-up study. Br J Cancer. 2008;98:1582–5. https://doi.org/10.1038/sj.bjc.6604313.
Morice P, Leary A, Creutzberg C, Abu-Rustum N, Darai E. Endometrial cancer. Lancet. 2016;387:1094–108. https://doi.org/10.1016/S0140-6736(15)00130-0.
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019;157. https://doi.org/10.1016/j.diabres.2019.107843.
Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol. 2018;14:88–98. https://doi.org/10.1038/nrendo.2017.151.
Anderson KE, Anderson E, Mink PJ, Hong CP, Kushi LH, Sellers TA, et al. Diabetes and endometrial cancer in the Iowa Women’s Health Study. Cancer Epidemiol Prev Biomark. 2001;10:611–6.
AlHilli M, Bakkum-Gamez JN, Mariani A, Shridhar V, Cliby BA, McGree M, et al. The impact of diabetes and metformin on clinical outcomes is negligible in risk-adjusted endometrial cancer cohorts. Gynecol Oncol. 2015;137:156–7. https://doi.org/10.1016/j.ygyno.2015.01.391.
Saed L, Varse F, Baradaran HR, Moradi Y, Khateri S, Friberg E, et al. The effect of diabetes on the risk of endometrial cancer: an updated a systematic review and meta-analysis. BMC Cancer. 2019;19:527. https://doi.org/10.1186/s12885-019-5748-4.
Friberg E, Orsini N, Mantzoros CS, Wolk A. Diabetes mellitus and risk of endometrial cancer: a meta-analysis. Diabetologia. 2007;50:1365–74. https://doi.org/10.1007/s00125-007-0681-5.
Luo J, Beresford S, Chen C, Chlebowski R, Garcia L, Kuller L, et al. Association between diabetes, diabetes treatment and risk of developing endometrial cancer. Br J Cancer. 2014;111:1432–9. https://doi.org/10.1038/bjc.2014.407.
Gunter MJ, Hoover DR, Yu H, Wassertheil-Smoller S, Manson JE, Li J, et al. A prospective evaluation of insulin and insulin-like growth factor-I as risk factors for endometrial cancer. Cancer Epidemiol Biomarkers Prev. 2008;17:921–9. https://doi.org/10.1158/1055-9965.EPI-07-2686.
Kim JJ, Chapman-Davis E. Role of progesterone in endometrial cancer. Semin Reprod Med. 2010;28:81–90. https://doi.org/10.1055/s-0029-1242998.
Mu N, Zhu Y, Wang Y, Zhang H, Xue F. Insulin resistance: a significant risk factor of endometrial cancer. Gynecol Oncol. 2012;125:751–7. https://doi.org/10.1016/j.ygyno.2012.03.032.
Wang Y, Zhu Y, Zhang L, Tian W, Hua S, Zhao J, et al. Insulin promotes proliferation, survival, and invasion in endometrial carcinoma by activating the MEK/ERK pathway. Cancer Lett. 2012;322:223–31. https://doi.org/10.1016/j.canlet.2012.03.026.
Han J, Zhang L, Guo H, Wysham WZ, Roque DR, Willson AK, et al. Glucose promotes cell proliferation, glucose uptake and invasion in endometrial cancer cells via AMPK/mTOR/S6 and MAPK signaling. Gynecol Oncol. 2015;138:668–75. https://doi.org/10.1016/j.ygyno.2015.06.036.
Benchahong S, Chanthasenanont A, Pongrojpaw D, Pattaraarchachai J, Bhamarapravatana K, Suwannarurk K. Efficacy of intrauterine lidocaine instillation in reducing pain during endometrial biopsy by Novak. Pain Res Treat. 2018;2018:1–7. https://doi.org/10.1155/2018/9368298.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2017;71:1269–324.
Doosup S, Chandrashekar B, Kullatham K. Impact of the discordance between the American College of Cardiology/American Heart Association and American Diabetes Association recommendations on hypertension in patients with diabetes mellitus in the United States. Hypertension. 2018;72:256–9. https://doi.org/10.1161/HYPERTENSIONAHA.118.11422.
Al-Rubeaan K, Siddiqui K, Al-Ghonaim MA, Youssef AM, Al-Sharqawi AH, AlNaqeb D. Assessment of the diagnostic value of different biomarkers in relation to various stages of diabetic nephropathy in type 2 diabetic patients. Sci Rep. 2017;7:2684. https://doi.org/10.1038/s41598-017-02421-9.
Feldman EL, Callaghan BC, Pop-Busui R, Zochodne DW, Wright DE, Bennett DL, et al. Diabetic neuropathy. Nat Rev Dis Primer. 2019;5:1–18. https://doi.org/10.1038/s41572-019-0092-1.
Association AD. Classification and diagnosis of diabetes: standards of medical care in diabetes—2018. Diabetes Care. 2018;41:S13–27. https://doi.org/10.2337/dc18-S002.
Murray MJ, Meyer WR, Zaino RJ, Lessey BA, Novotny DB, Ireland K, et al. A critical analysis of the accuracy, reproducibility, and clinical utility of histologic endometrial dating in fertile women. Fertil Steril. 2004;81:1333–43. https://doi.org/10.1016/j.fertnstert.2003.11.030.
Usta A, Turan G, Altun E, Hocaoglu M, Bulbul CB, Adali E. The usefulness of CD34, PCNA immunoreactivity, and histopathological findings for prediction of pain persistence after the removal of endometrioma. Reprod Sci. 2019;26:269–77. https://doi.org/10.1177/1933719118768697.
Mishra K, Wadhwa N, Guleria K, Agarwal S. ER, PR and Ki-67 expression status in granulomatous and chronic non-specific endometritis. J Obstet Gynaecol Res. 2008;34:371–8. https://doi.org/10.1111/j.1447-0756.2007.00700.x.
Samani SM, Bojnordi TE, Zarghampour M, Merat S, Fouladi DF. Expression of p53, Bcl-2 and Bax in endometrial carcinoma, endometrial hyperplasia and normal endometrium: a histopathological study. J Obstet Gynaecol. 2018;38:999–1004. https://doi.org/10.1080/01443615.2018.1437717.
Herod JJO, Eliopoulos AG, Warwick J, Niedobitek G, Young LS, Kerr DJ. The prognostic significance of Bcl-2 and p53 expression in ovarian carcinoma. Cancer Res. 1996;56:2178–84.
Friedenreich CM, Biel RK, Lau DCW, Csizmadi I, Courneya KS, Magliocco AM, et al. Case-control study of the metabolic syndrome and metabolic risk factors for endometrial cancer. Cancer Epidemiol Biomarkers Prev. 2011;20:2384–95. https://doi.org/10.1158/1055-9965.EPI-11-0715.
Bellou V, Belbasis L, Tzoulaki I, Evangelou E. Risk factors for type 2 diabetes mellitus: an exposure-wide umbrella review of meta-analyses. PLoS One. 2018;13:e0194127. https://doi.org/10.1371/journal.pone.0194127.
Park Y, Colditz GA. Diabetes and adiposity: a heavy load for cancer. Lancet Diabetes Endocrinol. 2018;6:82–3. https://doi.org/10.1016/S2213-8587(17)30396-0.
Lois K, Kumar S. Obesity and diabetes. Endocrinol Nutr Organo Soc Espanola Endocrinol Nutr. 2009;56(Suppl 4):38–42.
Shaw E, Farris M, McNeil J, Friedenreich C. Obesity and endometrial cancer. Recent Results Cancer Res Fortschritte Krebsforsch Progres Dans Rech Sur Cancer. 2016;208:107–36. https://doi.org/10.1007/978-3-319-42542-9_7.
Nestler JE, Powers LP, Matt DW, Steingold KA, Plymate SR, Rittmaster RS, et al. A direct effect of hyperinsulinemia on serum sex hormone-binding globulin levels in obese women with the polycystic ovary syndrome. J Clin Endocrinol Metab. 1991;72:83–9. https://doi.org/10.1210/jcem-72-1-83.
Weiderpass E, Brismar K, Bellocco R, Vainio H, Kaaks R. Serum levels of insulin-like growth factor-I, IGF-binding protein 1 and 3, and insulin and endometrial cancer risk. Br J Cancer. 2003;89:1697–704. https://doi.org/10.1038/sj.bjc.6601312.
Lukanova A, Zeleniuch-Jacquotte A, Lundin E, Micheli A, Arslan AA, Rinaldi S, et al. Prediagnostic levels of C-peptide, IGF-I, IGFBP -1, -2 and -3 and risk of endometrial cancer. Int J Cancer. 2004;108:262–8. https://doi.org/10.1002/ijc.11544.
Nagamani M, Stuart CA. Specific binding and growth-promoting activity of insulin in endometrial cancer cells in culture. Am J Obstet Gynecol. 1998;179:6–12. https://doi.org/10.1016/S0002-9378(98)70244-3.
Clement NS, Oliver TR, Shiwani H, Sanner JR, Mulvaney CA, Atiomo W. Metformin for endometrial hyperplasia. Cochrane Database Syst Rev. 2017. https://doi.org/10.1002/14651858.CD012214.pub2.
Asmat U, Abad K, Ismail K. Diabetes mellitus and oxidative stress—a concise review. Saudi Pharm J. 2016;24:547–53. https://doi.org/10.1016/j.jsps.2015.03.013.
Rahimi-Madiseh M, Malekpour-Tehrani A, Bahmani M, Rafieian-Kopaei M. The research and development on the antioxidants in prevention of diabetic complications. Asian Pac J Trop Med. 2016;9:825–31. https://doi.org/10.1016/j.apjtm.2016.07.001.
Brownlee M. The pathobiology of diabetic complications: a unifying mechanism. Diabetes. 2005;54:1615–25. https://doi.org/10.2337/diabetes.54.6.1615.
Cho K-H, Wolkenhauer O. Analysis and modelling of signal transduction pathways in systems biology. Biochem Soc Trans. 2003;31:1503–9. https://doi.org/10.1042/bst0311503.
Acknowledgments
The author would like to thank the subjects that participated in this study.
Funding
The study was supported by the Scientific Investigations Foundation of Balikesir University (project number: BAP.2020/010).
Author information
Authors and Affiliations
Contributions
CSU: Protocol/project development, data collection, data management, manuscript writing/editing. GT: interpretation, data management, manuscript writing/editing. CBB: data collection, data management, manuscript writing. KK: data collection, data management. MH: data management, manuscript writing/editing. AU: protocol/project development, manuscript writing/editing. EA: protocol/project development, manuscript writing/editing.
Corresponding author
Ethics declarations
Competing Interest
The authors declare that they have no competing interests.
Ethics Approval and Consent to Participate
The authors have no connection to any companies or products mentioned in this article. The Ethics Committee at Balikesir University School of Medicine approved this study (date: 10.04.2019/ registration number: 2019/65) and all participating patients provided written informed consent before starting the study. All participants were aware during the informed consent process that the results of this study may be published.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sancakli Usta, C., Turan, G., Hocaoglu, M. et al. Differential Expressions of Ki-67, Bcl-2, and Apoptosis Index in Endometrial Cells of Women With and Without Type II Diabetes Mellitus and Their Correlation with Clinicopathological Variables. Reprod. Sci. 28, 1447–1456 (2021). https://doi.org/10.1007/s43032-020-00423-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-020-00423-z