Abstract
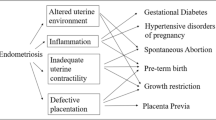
The aim of this review is to summarize the current literature regarding a link between endometriosis and adverse pregnancy outcomes. We also present an overview of common pathogenic mechanisms between endometriosis and obstetric complications. A computerized literature search was performed to identify relevant studies. The search covered the period between January 2008 and October 2018. Emerging evidence has revealed that endometriosis increased the risk of preterm birth, miscarriage, preterm premature rupture of membranes, placenta previa, preeclampsia, pregnancy-induced hypertension (PIH), gestational diabetes, gestational cholestasis, small for gestational age (SGA) babies, antepartum hemorrhage, postpartum hemorrhage, placental abruption, retained placenta, malpresentation, labor dystocia, cesarean delivery, stillbirth, neonatal death, and congenital malformations of the uterus, but the data are based on limited information. However, some studies have found that endometriosis did not affect pregnancy outcomes. Previous studies are heterogenous and the existing data are controversial. Limited evidence from a few studies also indicated that surgical excision of endometriosis may not reduce the risk of adverse pregnancy outcomes. Endometriosis and obstetric complications may share common pathophysiologic mechanisms, in which abnormal activation of inflammation, structural and functional alterations in the junctional zone, and perturbed uterine peristalsis may play important roles. In this review, we outlined evidence that women with endometriosis have a high risk of obstetric complications. We describe the common crucial features between endometriosis and obstetric complications.

Similar content being viewed by others
References
Petraglia F, Arcuri F, de Ziegler D, Chapron C. Inflammation: a link between endometriosis and preterm birth. Fertil Steril. 2012;98:36–40.
Scutiero G, Iannone P, Bernardi G, et al. Oxidative stress and endometriosis: a systematic review of the literature. Oxidative Med Cell Longev. 2017;2017:7265238.
Patel BG, Rudnicki M, Yu J, Shu Y, Taylor RN. Progesterone resistance in endometriosis: origins, consequences and interventions. Acta Obstet Gynecol Scand. 2017;96:623–32.
Parazzini F, Esposito G, Tozzi L, Noli S, Bianchi S. Epidemiology of endometriosis and its comorbidities. Eur J Obstet Gynecol Reprod Biol. 2017;209:3–7.
Teng SW, Horng HC, Ho CH, Yen MS, Chao HT. Wang PH; Taiwan Association of Gynecology Systematic Review Group. Women with endometriosis have higher comorbidities: analysis of domestic data in Taiwan. J Chin Med Assoc. 2016;79(11):577–82. https://doi.org/10.1016/j.jcma.2016.04.006.
Fernando S, Breheny S, Jaques AM, Halliday JL, Baker G, Healy D. Preterm birth, ovarian endometriomata, and assisted reproduction technologies. Fertil Steril. 2009;91:325–30.
Stephansson O, Kieler H, Granath F, Falconer H. Endometriosis, assisted reproduction technology, and risk of adverse pregnancy outcome. Hum Reprod. 2009;24:2341–7.
Conti N, Cevenini G, Vannuccini S, et al. Women with endometriosis at first pregnancy have an increased risk of adverse obstetric outcome. J Matern Fetal Neonatal Med. 2015;28:1795–58.
Lin H, Leng JH, Liu JT, Lang JH. Obstetric outcomes in Chinese women with endometriosis: a retrospective cohort study. Chin Med J (Engl). 2015;128:455–8.
Berlac JF, Hartwell D, Skovlund CW, Langhoff-Roos J, Lidegaard Ø. Endometriosis increases the risk of obstetrical and neonatal complications. Acta Obstet Gynecol Scand. 2017;96:751–60.
Fujii T, Wada-Hiraike O, Nagamatsu T, et al. Assisted reproductive technology pregnancy complications are significantly associated with endometriosis severity before conception: a retrospective cohort study. Reprod Biol Endocrinol. 2016;14:73.
Vannuccini S, Lazzeri L, Orlandini C, Tosti C, Clifton VL, Petraglia F. Potential influence of in utero and early neonatal exposures on the later development of endometriosis. Fertil Steril. 2016;105:997–1002.
Aris A. A 12-year cohort study on adverse pregnancy outcomes in Eastern Townships of Canada: impact of endometriosis. Gynecol Endocrinol. 2014;30:34–7.
Chen I, Lalani S, Xie RH, Shen M, Singh SS, Wen SW. Association between surgically diagnosed endometriosis and adverse pregnancy outcomes. Fertil Steril. 2018;109:142–7.
Li H, Zhu HL, Chang XH, Li Y, Wang Y, Guan J, et al. Effects of previous laparoscopic surgical diagnosis of endometriosis on pregnancy outcomes. Chin Med J (Engl). 2017;130:428–33.
Mekaru K, Masamoto H, Sugiyama H, et al. Endometriosis and pregnancy outcome: are pregnancies complicated by endometriosis a high-risk group? Eur J Obstet Gynecol Reprod Biol. 2014;172:36–9.
Benaglia L, Bermejo A, Somigliana E, Scarduelli C, Ragni G, Fedele L, et al. Pregnancy outcome in women with endometriomas achieving pregnancy through IVF. Hum Reprod. 2012;27:1663–7.
Benaglia L, Candotti G, Papaleo E, Pagliardini L, Leonardi M, Reschini M, et al. Pregnancy outcome in women with endometriosis achieving pregnancy with IVF. Hum Reprod. 2016;31:2730–6.
Vercellini P, Parazzini F, Pietropaolo G, Cipriani S, Frattaruolo MP, Fedele L. Pregnancy outcome in women with peritoneal, ovarian and rectovaginal endometriosis: a retrospective cohort study. BJOG. 2012;119:1538–43.
Nirgianakis K, Gasparri ML, Radan AP, Villiger A, McKinnon B, Mosimann B, et al. Obstetric complications after laparoscopic excision of posterior deep infiltrating endometriosis: a case-control study. Fertil Steril. 2018;110:459–66.
Kohl Schwartz AS, Wölfler MM, Mitter V, et al. Endometriosis, especially mild disease: a risk factor for miscarriages. Fertil Steril. 2017;108:806–814.e2.
Juang CM, Chou P, Yen MS, Twu NF, Horng HC, Hsu WL. Adenomyosis and risk of preterm delivery. BJOG. 2007;114:165–9.
Tamura H, Kishi H, Kitade M, Asai-Sato M, Tanaka A, Murakami T, et al. Complications and outcomes of pregnant women with adenomyosis in Japan. Reprod Med Biol. 2017;16:330–6.
Bayram C, Osmanağaoğlu MA, Aran T, Güven S, Bozkaya H. The effect of chronic pelvic pain scoring on pre-term delivery rate. J Obstet Gynaecol. 2013;33:32–7.
Harada T, Taniguchi F, Onishi K, et al. Obstetrical complications in women with endometriosis: a cohort study in Japan. PLoS One. 2016;11:e0168476.
Brosens I, Brosens JJ, Fusi L, Al-Sabbagh M, Kuroda K, Benagiano G. Risks of adverse pregnancy outcome in endometriosis. Fertil Steril. 2012;98:30–5.
Glavind MT, Forman A, Arendt LH, Nielsen K, Henriksen TB. Endometriosis and pregnancy complications: a Danish cohort study. Fertil Steril. 2017;107:160–6.
Mannini L, Sorbi F, Noci I, Ghizzoni V, Perelli F, di Tommaso M, et al. New adverse obstetrics outcomes associated with endometriosis: a retrospective cohort study. Arch Gynecol Obstet. 2017;295:141–51.
Exacoustos C, Lauriola I, Lazzeri L, De Felice G, Zupi E. Complications during pregnancy and delivery in women with untreated rectovaginal deep infiltrating endometriosis. Fertil Steril. 2016;106:1129–1135.e1.
Yamaguchi A, Kyozuka H, Fujimori K, et al. Risk of preterm birth, low birthweight, and small-for-gestational-age infants in pregnancies with adenomyosis: a cohort study of the Japan Environment and Children’s Study. Acta Obstet Gynecol Scand. 2019;98:359–64.
Kim SG, Seo HG, Kim YS. Primiparous singleton women with endometriosis have an increased risk of preterm birth: meta-analyses. Obstet Gynecol Sci. 2017;60:283–8.
Lalani S, Choudhry AJ, Firth B, Bacal V, Walker M, Wen SW, et al. Endometriosis and adverse maternal, fetal and neonatal outcomes, a systematic review and meta-analysis. Hum Reprod. 2018;33:1854–65.
Bruun MR, Arendt LH, Forman A, Ramlau-Hansen CH. Endometriosis and adenomyosis are associated with increased risk of preterm delivery and a small-for-gestational-age child: a systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2018;97:1073–90.
Zullo F, Spagnolo E, Saccone G, et al. Endometriosis and obstetrics complications: a systematic review and meta-analysis. Fertil Steril. 2017;108:667–672.e5.
Vigano P, Corti L, Berlanda N. Beyond infertility: obstetrical and postpartum complications associated with endometriosis and adenomyosis. Fertil Steril. 2015;104:802–12.
Falconer H. Pregnancy outcomes in women with endometriosis. Semin Reprod Med. 2013;31:178–82.
Ozkan S, Ceylan Y, Ozkan OV, Yildirim S. Review of a challenging clinical issue: intrahepatic cholestasis of pregnancy. World J Gastroenterol. 2015;21:7134–41.
Pérez-López FR, Villagrasa-Boli P, Muñoz-Olarte M, Morera-Grau Á, Cruz-Andrés P, Hernandez AV, et al. Association between endometriosis and preterm birth in women with spontaneous conception or using assisted reproductive technology: a systematic review and meta-analysis of cohort studies. Reprod Sci. 2018;25:311–9.
Leone Roberti Maggiore U, Inversetti A, Schimberni M, Viganò P, Giorgione V, Candiani M. Obstetrical complications of endometriosis, particularly deep endometriosis. Fertil Steril. 2017;108:895–912.
Leyendecker G, Kunz G, Kissler S, Wildt L. Adenomyosis and reproduction. Best Pract Res Clin Obstet Gynaecol. 2006;20:523–46.
Cozzolino M, Basile F, Pontrelli G. Effects of adenomyosis on obstetric outcomes: a literature review. Minerva Ginecol. 2019;71:146–54.
Lier MCI, Brosens IA, Mijatovic V, Habiba M, Benagiano G. Decidual bleeding as a cause of spontaneous hemoperitoneum in pregnancy and risk of preterm birth. Gynecol Obstet Investig. 2017;82:313–21.
Kishi Y, Suginami H, Kuramori R, et al. Four subtypes of adenomyosis assessed by magnetic resonance imaging and their specification. Am J Obstet Gynecol. 2012;207:114.e1–7.
Lier M, Malik RF, van Waesberghe J, Maas JW, van Rumpt-van de Geest D, Coppus SF, et al. Spontaneous haemoperitoneum in pregnancy and endometriosis: a case series. BJOG. 2017;124:306–12.
Cozzolino M, Corioni S, Maggio L, Sorbi F, Guaschino S, Fambrini M. Endometriosis-related hemoperitoneum in pregnancy: a diagnosis to keep in mind. Ochsner J. 2015;15:262–4.
Jiang L, Yan Y, Liu Z, Wang Y. Inflammation and endometriosis. Front Biosci (Landmark Ed). 2016;21:941–8.
Cappelletti M, Della Bella S, Ferrazzi E, Mavilio D, Divanovic S. Inflammation and preterm birth. J Leukoc Biol. 2016;99(1):67–78. https://doi.org/10.1189/jlb.3MR0615-272RR.
Perucci LO, Corrêa MD, Dusse LM, Gomes KB, Sousa LP. Resolution of inflammation pathways in preeclampsia-a narrative review. Immunol Res. 2017;65(4):774–89. https://doi.org/10.1007/s12026-017-8921-3.
Lindner U, Tutdibi E, Binot S, Monz D, Hilgendorff A, Gortner L. Levels of cytokines in umbilical cord blood in small for gestational age preterm infants. Klin Padiatr. 2013;225(2):70–4. https://doi.org/10.1055/s-0033-1334879.
Tarín JJ, García-Pérez MA, Hamatani T, Cano A. Infertility etiologies are genetically and clinically linked with other diseases in single meta-diseases. Reprod Biol Endocrinol. 2015;13:31.
Mu F, Rich-Edwards J, Rimm EB, Spiegelman D, Missmer SA. Endometriosis and risk of coronary heart disease. Circ Cardiovasc Qual Outcomes. 2016;9(3):257–64. https://doi.org/10.1161/CIRCOUTCOMES.115.002224.
Caserta D, Mallozzi M, Pulcinelli FM, Mossa B, Moscarini M. Endometriosis allergic or autoimmune disease: pathogenetic aspects--a case control study. Clin Exp Obstet Gynecol. 2016;43(3):354–7.
Sundqvist J, Falconer H, Seddighzadeh M, Vodolazkaia A, Fassbender A, Kyama C, et al. Endometriosis and autoimmune disease: association of susceptibility to moderate/severe endometriosis with CCL21 and HLA-DRB1. Fertil Steril. 2011;95(1):437–40. https://doi.org/10.1016/j.fertnstert.2010.07.1060.
Pope CJ, Sharma V, Sharma S, Mazmanian D. A systematic review of the association between psychiatric disturbances and endometriosis. J Obstet Gynaecol Can. 2015 Nov;37(11):1006–15.
Patel S. Disruption of aromatase homeostasis as the cause of a multiplicity of ailments: a comprehensive review. J Steroid Biochem Mol Biol. 2017;168:19–25. https://doi.org/10.1016/j.jsbmb.2017.01.009.
Vannuccini S, Petraglia F. Recent advances in understanding and managing adenomyosis. F1000Res. 2019;8:F1000 Faculty Rev-283. https://doi.org/10.12688/f1000research.17242.1 eCollection 2019.
Kunz G, Beil D, Huppert P, Leyendecker G. Structural abnormalities of the uterine wall in women with endometriosis and infertility visualized by vaginal sonography and magnetic resonance imaging. Hum Reprod. 2000 Jan;15(1):76–82.
Brosens JJ, Barker FG, de Souza NM. Myometrial zonal differentiation and uterine junctional zone hyperplasia in the non-pregnant uterus. Hum Reprod Update. 1998 Sep-Oct;4(5):496–502.
Leyendecker G, Kunz G, Herbertz M, Beil D, Huppert P, Mall G, et al. Uterine peristaltic activity and the development of endometriosis. Ann N Y Acad Sci. 2004;1034:338–55.
Leone Roberti Maggiore U, Ferrero S, Mangili G, Bergamini A, Inversetti A, Giorgione V, et al. A systematic review on endometriosis during pregnancy: diagnosis, misdiagnosis. Hum Reprod Update. 2016;22(1):70–103. https://doi.org/10.1093/humupd/dmv045.
Brosens I, Pijnenborg R, Benagiano G. Defective myometrial spiral artery remodelling as a cause of major obstetrical syndromes in endometriosis and adenomyosis. Placenta. 2013;34(2):100–5. https://doi.org/10.1016/j.placenta.2012.11.017.
Brosens I, Derwig I, Brosens J, Fusi L, Benagiano G, Pijnenborg R. The enigmatic uterine junctional zone: the missing link between reproductive disorders and major obstetrical disorders? Hum Reprod. 2010;25(3):569–74. https://doi.org/10.1093/humrep/dep474.
Saraswat L, Ayansina DT, Cooper KG, Bhattacharya S, Miligkos D, Horne AW, et al. Pregnancy outcomes in women with endometriosis: a national record linkage study. BJOG. 2017;124(3):444–52. https://doi.org/10.1111/1471-0528.13920.
Kim YM, Chaiworapongsa T, Gomez R, Bujold E, Yoon BH, Rotmensch S, et al. Failure of physiologic transformation of the spiral arteries in the placental bed in preterm premature rupture of membranes. Am J Obstet Gynecol. 2002;187(5):1137–42.
O’Callaghan D. Endometriosis--an update. Aust Fam Physician. 2006;35(11):864–7.
Brien ME, Baker B, Duval C, Gaudreault V, Jones RL, Girard S. Alarmins at the maternal-fetal interface: involvement of inflammation in placental dysfunction and pregnancy complications 1. Can J Physiol Pharmacol. 2019;97(3):206–12. https://doi.org/10.1139/cjpp-2018-0363.
Kobayashi H. Imprinting genes associated with endometriosis. EXCLI J. 2014;13:252–64.
Chen P, Wang DB, Liang YM. Evaluation of estrogen in endometriosis patients: regulation of GATA-3 in endometrial cells and effects on Th2 cytokines. J Obstet Gynaecol Res. 2016;42:669–77.
Cordeiro A, Neto AP, Carvalho F, Ramalho C, Dória S. Relevance of genomic imprinting in intrauterine human growth expression of CDKN1C, H19, IGF2, KCNQ1 and PHLDA2 imprinted genes. J Assist Reprod Genet. 2014;31(10):1361–8. https://doi.org/10.1007/s10815-014-0278-0.
Zadora J, Singh M, Herse F, Przybyl L, Haase N, Golic M, et al. Disturbed placental imprinting in preeclampsia leads to altered expression of DLX5, a human-specific early trophoblast marker. Circulation. 2017;136(19):1824–39. https://doi.org/10.1161/CIRCULATIONAHA.117.028110.
Burris HH, Baccarelli AA, Motta V, Byun HM, Just AC, Mercado-Garcia A, et al. Association between length of gestation and cervical DNA methylation of PTGER2 and LINE 1-HS. Epigenetics. 2014;9(8):1083–91. https://doi.org/10.4161/epi.29170.
Meis PJ, Michielutte R, Peters TJ, et al. Factors associated with preterm birth in Cardiff, Wales. II. Indicated and spontaneous preterm birth. Am J Obstet Gynecol. 1995;173:597–602.
Oprescu ND, Ionescu CA, Drăgan I, Fetecău AC, Said-Moldoveanu AL, Chirculescu R, et al. Adnexal masses in pregnancy: perinatal impact. Romanian J Morphol Embryol. 2018;59:153–8.
Boujenah J, Salakos E, Pinto M, Shore J, Sifer C, Poncelet C, et al. Endometriosis and uterine malformations: infertility may increase severity of endometriosis. Acta Obstet Gynecol Scand. 2017;96:702–6.
Funding
This work was supported by JSPS KAKENHI Grant Numbers JP16K11150, 18 K09269, and 18 K09234.
Author information
Authors and Affiliations
Contributions
NK, KO, and CY performed the literature search and collected data regarding the data supporting the common epidemiology and shared pathophysiology using the Web database. HK and CY made substantial contribution to the conception of the study. HK contributed to the study design and interpretation of included research studies. The final version of the manuscript has been read and approved by all authors.
Corresponding author
Ethics declarations
Ethical Approval
Not applicable.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
One-sentence summary
Endometriosis may increase the risk of obstetric complications, possibly through common pathophysiologic mechanisms such as inflammation.
Electronic Supplementary Material
ESM 1
(DTD 43 kb)
Rights and permissions
About this article
Cite this article
Kobayashi, H., Kawahara, N., Ogawa, K. et al. A Relationship Between Endometriosis and Obstetric Complications. Reprod. Sci. 27, 771–778 (2020). https://doi.org/10.1007/s43032-019-00118-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-019-00118-0