Abstract
Research and innovation in the area of robotics in healthcare has seen significant growth in recent years. Global trends indicate that patients are getting older and sicker, while demands in healthcare workers are increasing their chance of injury. Robotic technology has the potential to enable high levels of patient care, clinical productivity and safety for both patients and healthcare workers. This paper surveys the state-of-the-art in robotics in healthcare and well-being, with particular attention to the key barriers and enablers to the implementation of this technology in real-world settings. Desktop research was used to identify available and emerging robotic technology currently in use (or with potential use) in healthcare settings. Primary sources of information included: academic publications, international organisations, commercial websites and online news agencies. In this paper, applications of robots in healthcare were divided into five main areas: service, assistive, socially-assistive, teleoperated and interventional robots. The maturity and readiness of different products is still an open challenge, with service and interventional robots leading the way. Wide-spread adoption of robots is likely to happen as the cost of the technology reduces, and wide evidence of beneficial long-term impact is available. This manuscript identified the main drivers, challenges, opportunities and considerations for implementing robots in healthcare. We hope this manuscript will raise awareness about robotics in healthcare among a wider audience to maximise availability, quality, and acceptability this technology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Robots are physically embodied systems capable of sensing and responding to the world through physical interaction. They can vary in their aesthetic appearance, sensing capabilities and degree of autonomy [1]. They can handle materials that are hazardous to humans, can undertake repetitive activities with great precision, and are immune to psychological wear [1].
With more than 10% of the global gross domestic product (GDP) spent on healthcare [2], digital innovation is increasingly important to both reduce costs and improve outcomes. Robotics is one area of digital innovation that can have wide impact in healthcare.
The use of robotic technology in healthcare is not a new concept. Technological advances in the 1980s led to one of the first documented applications of robots in healthcare, used to define the trajectory of a brain biopsy [3]. Since then, technology has rapidly progressed impacting positively the capabilities of robots. Robotic systems today are used in well-defined tasks such as hospital logistics, productivity, and pharmacy automation [4, 5]. Moving forward, we foresee that emerging technology will improve robots’ abilities even further, allowing them to be more self-sufficient and work more closely with humans. In fact, the use and demand of robotics and automation in healthcare is increasing every day [5, 6].
Although there has been a significant progress in the field of robotics [4, 7,8,9,10,11,12,13], a general lack of exposure and understanding of robots in healthcare is a major barrier to developing positive attitudes among stakeholders, including clinicians [14, 15]. Society acceptance of robots varies widely depending on their application. To achieve greater acceptance, robots in healthcare should focus on providing support to patients and clinicians. Tasks that appear to replace people should be considered with caution [16]. While many experimental studies have demonstrated the potential positive impacts of robots in healthcare, the impacts on long-term adoption are not well known with large-scale studies in real-life settings still needed to show economic, societal and health impacts [5, 17].
Using information collected from a range of sources, this paper identifies the main stakeholders, settings and applications of robots in healthcare and wellbeing. The main objective is to provide a comprehensive review on the state-of-the-art, and chart the main opportunities to inform future developments, as well as the challenges and necessary considerations for implementation of robots in healthcare. This manuscript also aims at raising awareness about robotic technology in healthcare among a wider audience.
Since the overall sector of robotics in healthcare is still an emerging area, it is difficult to make a final conclusion about the future trajectory. Nonetheless, this paper extends previous work [5, 6, 18, 19] to illustrate the major themes and future directions for this field, and provides examples from current and past research and commercial implementations. The identification of drivers, challenges, applications and key recommendations to the implementation of robots in healthcare presented here can be used as guideline to the future development and implementation of robotic solutions in healthcare.
This paper is organised as follows. A brief introduction to the field of robotics is presented in Sect. 2, followed by the main drivers for robotics in healthcare (Sect. 3). Then, a review of the landscape grouped into five main areas of application—service, assistive, socially-assistive, teleoperated and interventional robots—is introduced in Sect. 4. A discussion around the future of robotics in healthcare, including the main challenges and recommendations for their implementation in a health context is presented in Sect. 5 followed by the conclusion in Sect. 6.
What is a Robot?
The term robot comes from the Czech word ‘robota’, meaning slave, servant, or forced labour. The modern use of the term was first encountered in the 1920s play Rossum Universal Robots where Karel Čapek used it to denote an artificial fictional automaton. The modern perception of robots, however, leans on developments in artificial intelligence (AI) and mechatronics. More specifically, robots are defined as mechanical (physically embodied) artificially intelligent agents with the ability to move in the physical environment to perform complex tasks. This means that devices without mechanical action are not generally regarded as robots. Based on this definition, robots can typically do three things either autonomously or semi-autonomously: sense their environment, carry out computations to make decisions, and perform coordinated mechatronic actions in the physical world. While the details of these three components vary from robot to robot, most robots constantly repeat this sensing-cognition-acting cycle.
Robots are often described in terms of two classes: industrial and service robots [20]. Industrial robots are used in manufacturing automation, while service robots are used for personal, domestic and professional settings. Healthcare robots are simply the application of service robots to support the provision of healthcare services including (but not limited to) diagnose and treat conditions, support the functioning of impaired individuals, rehabilitation, care and medical intervention of patients [4, 5, 7]. While industrial robots were developed primarily to automate dirty, dull, and dangerous tasks without human intervention [21]; service and healthcare robots are designed for entirely different environments and tasks, including those that involve direct interaction with human users in hospitals, rehabilitation clinics, and the family home [22].
Today, more than eight million robots are in use around the world [23]. While robots in healthcare are still in the early stages of development and experimentation [24], the field is expected to grow in the face of demographic change, shortages of healthcare personnel, and a need to improve quality of care at reduced costs.
Global Drivers of Robotics in Healthcare
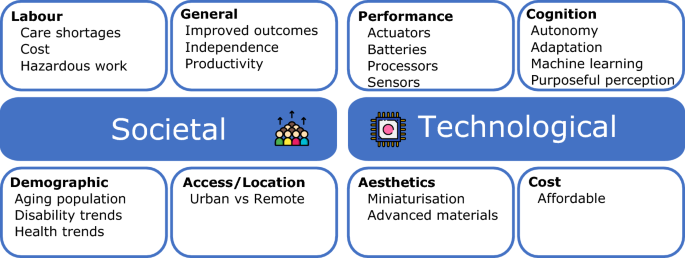
The application of robotics in healthcare depends heavily on societal need, acceptance and satisfaction. The primary reasons for implementing robotic technology in healthcare is normally a robot’s ability to deliver value to the health system through more effective and affordable healthcare, timely and continuous access to clinicians, and a system that supplements the efforts of caregivers by optimising care delivery and reducing human error and workplace injury [18, 25]. This section describes the key drivers of robotics in healthcare, focusing on two main areas: societal and technological drivers (Fig. 1).
Societal Drivers
Societal drivers lie in three main areas: broadening access to healthcare, reducing labour costs, and improving patient outcomes. Challenges related to these areas are expected to grow in the face of an ageing population, and increases in chronically-ill and disabled.
The world has a rapidly ageing population [26]. Due to the post World War II “baby boom”, the percentage of people above 65 is growing. Additionally, increased welfare and better medical procedures allow people to live longer. Associated with an ageing population is an increased prevalence of injuries, disorders and diseases [27]. Furthermore, across the age spectrum an estimated 90% of the world’s population experiences difficulties with physical, cognitive, mental or behavioural health [27]. These experiences may be temporary or permanent, acute or chronic, and may change throughout one’s lifespan. If left unchecked, trends in chronic disease risk factors—combined with a growing and ageing population—indicate a significant increase in the numbers of people living with life-long conditions including diabetes, obesity, and cancer [27, 28].
Direct challenges of a changing population include workforce shortages and limited availability of informal (family) care providers. Projections show that severe shortages should be expected, especially in the nursing professions [29, 30]. With the expanding demand, healthcare workers face increasingly hazardous work environments which exposes them to great risk of debilitating injury and disability [30]. Additionally, scarcity of nurses, doctors, and specialists means that some people will not receive the care they need, at least not in a timely manner. This is particularly concerning given the coronavirus (COVID-19) pandemic, which has been highly demanding on healthcare personnel worldwide. Increasing life-long independence from the medical system thus becomes a key societal driver. Enabling elderly and chronically-ill to stay at home longer and healthier will reduce the need for specialised healthcare, while improving independence and well-being in caregivers. Enabling informal caregivers and people with life-long conditions to go into workforce would also offset the expected reduction in available workforce.
Access to effective healthcare is also directly related to productivity, affordability and scarcity. While the need for medical procedures and treatments is limitless, the resources available to supply them are limited [31, 32]. Therefore, treatment is often restricted to urgent cases. Existing medical interventions can be improved through the use of robots to be less invasive, more cost-effective, and produce less side effects [13, 33, 34]. More effective methods of training for medical practitioners can also be introduced to reduce the number of medical errors [35,36,37,38]. There is also a constant drive to make it possible for procedures to be performed in less specialised places, and by less highly educated professionals [13, 39].
Access to healthcare is also related to location. People living in regional and remote locations are especially affected by a lack of specialised healthcare, with health outcomes consistently below average [40]. Distance and unstructured environments are significant obstacles to providing on-site quality care. Autonomous, semi-autonomous, and teleoperated robots can provide an alternative to health service delivery for people outside populated areas [13, 39, 41, 42]. Similar obstacles exist as a result of self-isolation restrictions implemented in response to COVID-19, that can be alleviated with the use robots [7, 43, 44].
Finally, there are several categories of socio-cultural factors that drive developments in healthcare. The first category relates to rising expectations about health as a result of socio-cultural changes influenced by media and education. These expectations relate not only to the health services themselves but also to the way they are delivered to empower patients. The second category includes safety. With changing practices as a results of social distancing restrictions (due to COVID-19), patient and clinician safety are in the forefront. The third and last factor is connectivity. There are over 5 billion internet users around the world, with about half of them accessing the internet over mobile devices. This connectivity is influencing the way we look after our health. Changes in regulation around the world reflect a significant emergence of patient-centric technologies, including mobile applications and associated devices to support the provision of healthcare services [45,46,47]. These types of regulations are expected to be widen as new technology is developed.
Technological Drivers
Technology drivers for robotics in healthcare are similar to those for other technologies: falling prices, increasing performance of sensors, faster processors, larger storage devices, increasing miniaturisation of electronic and mechanical devices, advances in batteries and communications hardware, advances in machine cognition (i.e., AI), persistent autonomy and advanced materials.
Additionally, the use of robots in healthcare involves physical interaction between caregivers, patients, and technology. The reciprocal nature of human-robot interactions means that a robot needs to be able to perceive and understand its environment to be able to provide useful feedback to humans, whether that person is a caregiver or a patient. Recent developments in sensing and machine learning (i.e., deep-learning) have demonstrated that progress in robotic perception is evolving in a way that new applications and real-world tasks can become a reality. Examples include object detection, scene understanding, and activity recognition that allow robots to navigate and interact with people in safe and effective ways [48, 49]. Data from several sources can be combined to create more purposeful perception systems than those available from a single source of data [50, 51].
Developments in AI are also improving the abilities of robots to interact with people in natural and intuitive ways, providing more personalised, adaptive and long-term support to individuals [52, 53]. Several recent developments in how people interface with robots have enabled robot orthoses and exoskeletons to offer neural integration, and increasingly more intuitive control of the limb [54].
Additionally, a range of advances in actuation, power, and control have enabled clinicians to have improved dexterity and visualisation inside the body [55]. There is also recent progress in the field of micro robots, where miniaturisation and increasing intelligence have led to new functionalities and areas of application [55]. As such, it is expected that ongoing technological developments will not only improve current applications of robots in healthcare, but will also open more areas of opportunity.
Landscape of Robotics in Healthcare
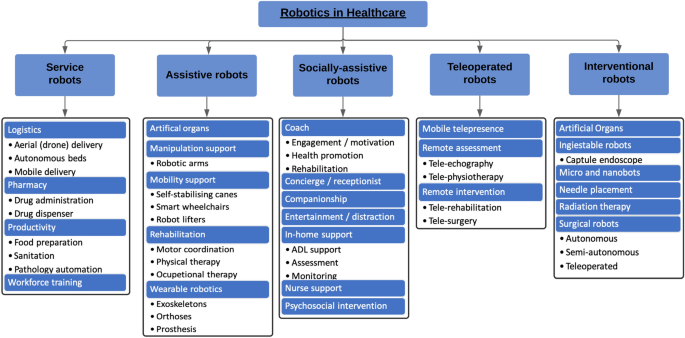
The domain of healthcare robotics is diverse. Robots can provide both physical and cognitive support. They can take part in a range of activities and settings from prevention and assessment to medical intervention, and from short-term rehabilitation to long-term care support. Within these activities, robots can support clinical staff, administration and hospital services [56]. In this vein, this manuscript identifies five major areas of application for robots in healthcare (Fig. 2). This section provides an overview of these areas, including examples of commercial products in use, areas where significant development is taking place, main challenges, and potential future applications.
Service Robots
Clinicians spend significant amounts of time on tasks that keep them away from patients including dirty, dull, distant, dangerous or repetitive jobs, such as moving materials or people from one place to another, and waiting for patients, materials, and medications [19, 57]. The overburden of these tasks can create a climate for error, frustration and burnout. Service robots in healthcare can assist clinicians with these tasks. These robots have limited requirements to function in close proximity to hospital personnel or patients. As such, most systems pose little risk to patients.
One of the best tasks for robots in this space is logistics and transportation (Table 1), where robots can be exceptionally accurate at given the right conditions. For example, mobile robots can fetch and deliver linen, pathology samples, medication, and food [58,59,60]. These systems can automate the delivery of goods/supplies for pharmacies, nursing stations, kitchens, or laboratories; enabling operation with little disturbance to staff and patients. Another task that robots can do effectively is moving patients using autonomous motorised hospital beds. While autonomous beds are not yet widely available, it is believed that these systems could improve efficiency and reduce musculoskeletal injuries in clinicians [61, 62]. There is also potential for aerial vehicles (i.e., drones) to be used in short- and long-distance delivery of consumables, medications and pathology samples [41, 42].
There are some challenges associated with logistic systems. Mobile deliveries need available paths (or hallways) within the premises that must be taken into consideration during the installation or architectural design of new institutions. Aerial vehicles, on the other hand, are exposed to harsh forces of the weather such as wind and rain—not to mention restrictions from international aviation authorities [73]. In spite of these challenges, it is expected that robots will automate many delivery-based services in the near future, and at a reasonable cost.
There is also increasing interest in the use of robots to support workforce training and education to improve patient safety and quality of care. Robotic patient simulators are life-sized anthropomorphic robots that can simulate the acts of breathing, bleeding, speaking, expelling fluids, and responding to medications in similar ways to real patients. These types of robots allow clinicians to simultaneously practice both procedural and communication skills. Examples of workforce training robots include a system to simulate prostate exams [35] and robots that simulate the behaviour of patients’ limbs [36, 74]. Other researchers have focused on developing robot-based simulations of a patient’s facial expressions for medical diagnosis training [37], a patient’s act of gazing or turning away during injections [75], and a patient’s oral cavity for dental training [76] or airway management training [38].
The problem of handling an ever increasing number of analyses in pathology is common to all laboratories and disciplines. Pathology automation robots aim to optimise processes within the laboratory, streamline operations, improve efficiency, reduce manual handling and free up staff for more productive tasks. Laboratory automation has been commercially available for many years and, similar to industrial robots, it allows for tasks to be completed without user intervention. Total laboratory automation is an effective mean to eliminate batch processing delays and achieve a consistent and reliable laboratory service [77].
A different type of service robots that has already been proven to be effective are pharmacy dispensing robots [63, 64]. Dispensing machines provide computer-controlled dispensing and tracking of medications. They decrease the potential for administration errors, and save nursing and pharmacists’ time by eliminating the need for manual narcotic counts and inventory management. These robots have shown significant increases in pharmacy storage capacity, and a decrease in dispensing errors and time required to pick items for dispensing [59].
Another relevant application of service robots includes sanitation robots, such as a climbing robot to clean hospital walls using disinfecting liquids [59], and a mobile platforms with arrays of ultraviolet (UV) lamps used to disinfect patient rooms and operating theatres [70, 71]. Sanitation robots attracted significant attention during the COVID-19 pandemic, to kill the COVID-19 virus within hospitals [4].
Assistive Robots
Assistive robots support people with a physical disability to complete necessary activities of daily living (ADL) independently including personal hygiene, eating and leisure. The type of support provided by assistive robots includes manipulation, mobility and rehabilitation.
Robots for manipulation support patients with functionalities of the arm and hand. Robotic arms fitted with grippers are commonly designed to perform specific activities such as eating, brushing teeth, washing, picking up objects and opening doors [78,79,80]. Handy 1, for example, was one of the first low-cost robots used for multitask manipulation support for activities such as feeding and washing [81]. More recent examples include Obi [82] and the Neater Eater [83]. Both platforms are commercial feeding support robots designed to help people with upper limb disability [78].
Robots for mobility support are intended to help people with mobility impairments navigate from one place to another. The wheelchair is one of the most important mobility support tools. However, many people are not able to use a traditional wheelchairs due to, for example, blindness, limited muscle power in the arms, or limited eye-hand coordination. Smart wheeled platforms (including smart wheelchairs) provide needed opportunities to those individuals. A smart wheeled platform is a powered mobile device to which computers, sensors, and assistive technology are attached to. A good example is the iBOT wheelchair from DEKA (now in partnership with Toyota). Unlike most wheelchairs, iBOT can go up and down stairs and allows the user to rise from a sitting to a standing position [84, 85]. Alternative approaches focus on wheelchairs with automated navigation support for those users with difficulties manoeuvering powered wheelchairs [84, 86].
Similar to wheelchairs are smart walkers, which can support individuals with limited standing, walking or balancing ability, or who suffer from additional limitations (e.g., blindness). The Lean Empowering Assistant by Robot Care Systems [87], for example, is a roboticised walker with active guidance, navigation and motion. Other example includes the Smart-Cane and Smart-Walker, which can detect obstacles and build a map of their surroundings in order to localize the user inside the map, and subsequently guide them to different waypoints [88].
In some cases, both mobility and manipulation support are needed. Wheelchair-mounted robot arms can provide improved means of manipulating objects. Examples include PerMMA [89, 90] and JACO [91]. In these systems, the user’s motion intention is commonly extracted through either manual manipulation (e.g., joysticks and buttons) or sensors implanted in the user’s body [92].
Another technology that provides both mobility and manipulation support is wearable robots such as prostheses, orthoses, and exoskeletons [9, 93,94,95]. A prosthesis is a device that supplants a person’s missing limb. Robotic prosthetics aim to fully emulate a missing limb through replication of its joints and limb segments, and seamless integration that provides intuitive control of the limb as well as touch feedback to the wearer [93, 94].
Orthoses and exoskeletons, on the other hand, help people with intact limbs with limited movement or control. Orthoses protect, support, or improve the function of body parts such as ankles, knees and the spine. Robotic orthoses are typically designed in the form of an exoskeleton which envelopes the body part in question. They allow free motion of limbs while providing the required support. Most recent robotic exoskeletons are still expensive and have limited battery (power) to be used as orthoses, and are only used within rehabilitation clinics. Comprehensive reviews of upper and lower limb rehabilitation exoskeletons are available in [9, 95].
In rehabilitation, robots are normally intended to help with functional restoration to both the lower and upper body. The main objective is to increase training intensity and assessment of progress compared to using a human therapist. Common conditions that are treated with rehabilitation robots include spinal cord injury, sports injury, stroke, musculoskeletal pain syndromes, fibromyalgia and traumatic brain injury [25]. Rehabilitation robots can also be used to support muscle sustaining therapies. Examples of commercial robots for upper-limb rehabilitation include MIT-Manus, ArmeoSpring and ReoGo [92], while Lokomat is the most well-known lower-limb rehabilitation system [33, 92, 96]. Additional examples of mobility support and rehabilitation robots are available in [5].
Advances are also being made towards robots that assist in lifting patients in a semi-automated way. Robear [97] and RIBA [98], for example, are specifically designed to help lift and move a bedridden patient from a bed to a wheelchair and back. Other types of assistive robots that support staff and patients include the RobotBathtub, which is used to bathe a person while they lie down; and the Quirubot, a robotic scrub nurse [80].
Socially-Assistive Robots
Socially-assistive robots (SARs) provide assistance to humans through social interaction, rather than physical intervention. To be effective, SARs must understand and interact with their environment, exhibit social behaviour, sustain engagement and achieve specific assistive goals. They should do this in a way that is safe, ethical and effective.
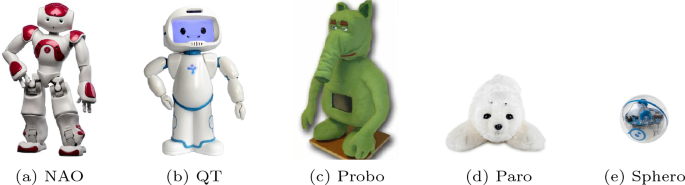
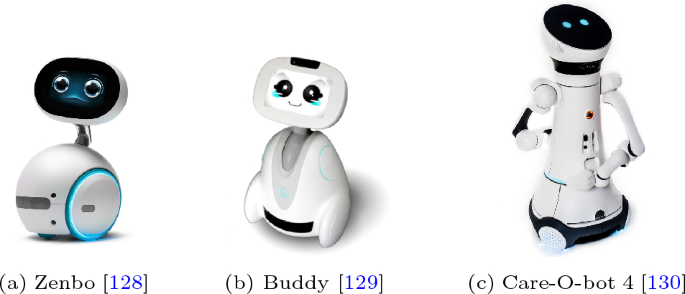
The robot’s physical embodiment and behaviour are at the heart of SARs’ effectiveness, as they leverage the inherently human tendency to engage with life-like (but not necessarily human-like) social behaviour. Based on their appearance, SARs can be divided into three main categories: anthropomorphic, zoomorphic and non-biomimetic robots (Fig. 3). Anthropomorphic robots are those designed with a human-like resemblance, such as a head, eyes, torso, arms or legs. These robots can provide complex behaviour patterns, such as those available in interpersonal interactions, and evoke social behaviours and perceptions in the people they interact with, while appearing less intimidating and more predictable than humans. Zoomorphic robots are non-threatening animal-like robots that allow for the expression of limited social cues that are appropriate to their physical form. The interactive behaviour of these robots are often simpler to those available in anthropomorphic robots. Finally, non-biomimetic robots are those designed without considering their resemblance to any biological species. Non-biomimetic robots are commonly used to engage children in free-play [99], or as catalysts for interaction with adults or children [100].
SARs have the potential to enhance the quality of life for large populations of users, including the elderly [101], individuals with cognitive impairments [102], and children with socio-developmental disorders [17, 103]. A popular application is the use of robots to provide comfort or companionship, with some solutions breaking out of academia into the market as commercially available products. Paro the robotic seal (Fig. 3d), for example, was the first long-standing SAR certified by the U.S. Food and Drug Administration (FDA) as a neurological therapeutic device shown to decrease stress, anxiety, and medication in elderly patients [101, 104]. More recently, the Mabu robot was deployed as an in-home personal companion for patients with chronic health issues [105]. Companion robots like Mabu (by Catalia Health [106]), Paro, and My Special Aflac Duck (by Aflac and Sproutel [107]) can assist with emotional support, medication adherence, health monitoring and to encourage exercise [11, 108].
SARs are also used to support psychosocial interventions (e.g., social, cognitive and behavioural therapy). One of the most common applications in this area is the diagnosis and treatment of autism spectrum disorder (ASD) and cognitive impairments; see [8, 109] and [110] for comprehensive reviews. SARs hold great potential in this area, with many recent studies reporting that autonomous and remotely-operated robots can promote, among other skills, facial expression recognition [111], joint attention [112], imitative free-form play [113], verbalisation [103], and turn taking [114]. The advantage of robots in support of therapy and education lies in their controllable behaviour and ability to repeat actions. Other examples of SARs used in psychosocial interventions include ageing, where robots can reduce anxiety and increase social interaction with peers [11, 115, 116], and cognitive rehabilitation intervention for adults with intellectual disability [102].
SARs have shown to increase engagement and motivation. They have been used to coach young children on nutrition and healthy food choices [117], to help children with type 1 diabetes learn about their illness [118], and to reduced paediatric distress in oncology patients by teaching children about their condition and providing them with techniques to manage their distress [119]. New strategies that provide interesting and motivating interventions are often incorporated to improve participation and performance. In this vein, SARs have successfully served as motivators with weight management and self-monitoring strategies [120], as tools to motivate physical exercise in older adults [121], and as support tool to physical therapy intervention for children with cerebral palsy [122]. It has been observed that the motivation generated by the interaction with a SAR facilitates the persistence in exercise (e.g., walking) and the fulfilment of objectives [122,123,124].
SARs are also entering patients’ homes to assist with everyday needs and nursing support (e.g., medication reminders and health monitoring) to people with chronic conditions, the elderly and individuals with cognitive impairments [11, 108, 125, 126]. Fischinger et al. [127], for example, presented the development and evaluation of ‘Hobbit’ a care robot to promote ageing in place and postpone the need to move to a care facility. Hobbit is designed especially for fall detection and prevention. While most personal assistance robots are only available as research platforms, there is growing interest to build-up on the momentum of AI assistants and develop SARs to assist within the home environment. Commercial examples include Zenbo, Buddy and Care-O-bot 4 (Fig. 4).
While these robots have the ability to support people with a range of relatively simple activities, a stand-alone platform that can successfully support people with most ADL is a long way from reaching the consumer market, particularly due to the high degree of manual dexterity, sensing and learning capabilities required. An overview of personal home robots is available in [131].
Robots are normally limited by their onboard functionality and hardware. However, they have the ability to leverage information from other technologies in their environment to perform more complex tasks and requests [108]. For example, a smart environment can be used to locate a patient when the robot is called for support, enhancing navigation skills [132]. A similar approach can be used to find misplaced items for the elderly [133].
SARs are also being trialled for use as concierges or receptionists answering questions, checking appointments, assigning patients to medical staff and delivering information and public health education [134,135,136]. Research is also available in which SARs are used as guides (multilingual way finders) greeting and helping people navigate from one spot to another within a hospital [137], and as entertainers or distractors to reduce stress during hospital stays [138,139,140,141]. SARs are also being developed to follow doctors or nurses during medical rounds, carry armamentarium, and record electronic health data [142].
Finally, SARs played an important role to prevent the spread of coronavirus during the COVID-19 pandemic [143]. In this vein, SARs performed three main activities: (1) liaison, where robots acted as a links between humans to minimize human-human contact (e.g., patient registration, book appointments, and print prescriptions); (2) safeguard, including all functions related to ensuring risk-free environments (e.g., safety advice and enforce protective measurements); and (3) well-being support, where robots acted as coaches to preserve physical and psychological well-being (e.g., companionship and entertainment). A comprehensive review of the implementation of SARs during the COVID-19 pandemic is available in [143].
Despite showing great promise, there has been skepticism against the use of SARs in healthcare. It has been hypothesised that clinicians perceive robots as expensive and limited tools which provide no real advancement to current protocols [144]. A significant reason behind this is that the benefits of SARs have been demonstrated particularly in short-term studies with small groups of participants, with very few following clinically-valid randomised controlled trials (RCTs) to evaluate their efficacy [109, 139, 145]. While current clinical evidence is insufficient, research suggests that SARs constitute a promising opportunity to support health management needs particularly in children, elderly and individuals with cognitive impairment.
Teleoperated Robots
Teleoperated robotics, or telerobotics, is considered to be a part of telehealth. The ultimate goal is to provide specialised healthcare services over long distances. Telerobotics can virtually bring specialists to areas where medical facilities and experts are not available [13]. Telerobotics (and telehealth) has become particularly pertinent since the COVID-19 pandemic began, primarily due to the rising demand for contactless healthcare. Telerobotics allows for procedures such as surgeries, treatments, and diagnoses to be conducted remotely.
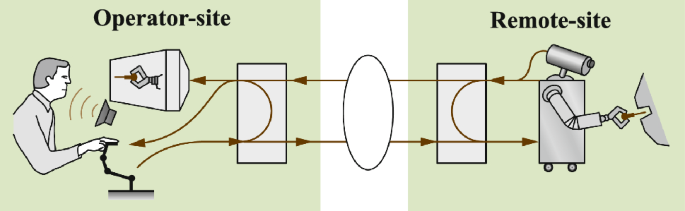
In a teleoperated robot (or telerobot), a human operator controls the movements of robots remotely, via wired and/or wireless communication networks. Most teleoperated robots are semi-autonomous, task-oriented and have a limited range of functions. While the physical separation may be very small (e.g., within the same room), telerobotic systems are—at least conceptually—split into two different sites. In this manuscript, the term telerobotics is used to describe the provision of remote services where there is a significant distance between the two sites (i.e., they are not within the same building).
In telerobotics, the local site encompasses the human operator (typically a clinician) and all elements needed to control the system, while the remote site contains the robot and the environment to be manipulated (Fig. 5). The local and remote systems are called “master” and “slave” respectively. The slave robot is commonly programmed to follow the motions of the master.
Overview of a telerobotic system. Adapted from Niemeyer et al. [39]
Teleoperated robots can provide access to treatment for people outside populated areas and in disaster scenarios. Remote surgery (or telesurgery), for example, is the ability for a doctor to perform surgery on a patient from a remote site [146]. The promise of telesurgery is to allow the expertise of specialised surgeons to be available for patients worldwide, without the need for either of them to travel beyond their local hospital.
The first successful telesurgery, named “Operation Lindbergh”, took place in 2000 using a dedicated multiservice transmission network provided by France Telecom, and a surgery robot called Zeus [147]. In Operation Lindbergh, a laparoscopic intervention was performed on a patient located in Strasbourg, France while the operating surgeon was located in New York, USA. Since then, different systems have been successfully trialled around the world. Recent examples include the RAVEN robot for laparoscopic surgery research and the RIME robot for transpedicular fixation surgery [13]. None of these systems are available for commercial use.
The two main factors impacting progress in telerobotic surgery are data transmission speed and communication latency. Effective stable connections that offer minimum latency delays are expensive, and their availability is limited particularly in remote and rural areas. With previous studies indicating that latency delays are associated with more errors [148], additional trials to improve data transmission and evaluate the efficacy and safety of this systems are needed.
Making a diagnosis usually requires the attendance of a doctor. New developments in telerobotics make remote assessment of patients possible. The MELODY system (by AdEchoTech), for example, is a tele-echography robot that facilitates ultrasonography over a distance [149]. The doctor who is performing the examination is assisted by a paramedic at the patient’s site who positions the robot over the patient, but is the expert who remotely manipulates the ultrasound probe. Telerobots can also support clinicians with other tasks, such as the remote evaluation and rehabilitation of upper-limb function [150, 151].
A subfield of telerobotics is “telepresence”, which refers to systems that include immersive interfaces that help the operator feel present in the remote site using feedback from vision, audio, touch and even smell and taste. There is also potential to increase the level of interaction between telepresence robots and the patients/environment via sensors and manipulators. Examples of telepresence robots used in healthcare include the RP-VITA robot (by iRobot and InTouch Health), an FDA-approved telepresence robot to allow clinicians to check in patients remotely [152, 153]; ROBIN, a telepresence robot integrated into a sensor-rich environment to support independent living [154]; and RoboConsultant, a telepresence robot to facilitate intraoperative consultation by expert surgeons located in remote sites [155].
Most telepresence robots to date are essentially a video chat session on a mobile platform. The physicality and interactive abilities of robots, however, can yield a stronger feeling of presence for both patient and caregiver. A number of studies have shown that mobile telepresence robots can help reduce the length of stay after minor invasive surgery [156] and at intensive care units [157], as well as reduce response times in emergency situations [157, 158]. In other studies, patients agreed that mobile telepresence robots should be part of regular hospital care, and stated that they would rather be seen remotely by their own physician than by a different physician [159, 160].
Telepresence robots can also provide unique opportunities to people who are homebound or hospitalised due to either a medical condition or a disability. Friedman and Cabral [161], for example, evaluated the use of a mobile telepresence robot operated by people with developmental disability in exploring a public exhibit. Their study revealed positive trends toward the use of mobile telepresence robots to improve wellbeing, physical and social self-efficacy. Similar studies were conducted to improve the hospital experience of paediatric patients [162] and people with motor disabilities [163]. Telepresence was one of the most widespread functions of robots during the COVID-19 crisis [143].
Telerobotics remains an exciting area of robotics. In many ways, it forms a platform which can use the advances in technology while leveraging the skills and capabilities of clinicians. Teleoperated robots can serve as a pathway for a gradual introduction of autonomous robots into healthcare.
Interventional Robots
The main goal of interventional robots is to assist medical practitioners in executing efficient and safe diagnostic or therapeutic procedures. The usual motivation is to increase precision rather than efficiency. As such, a range of advances have been made that enable clinicians to have improved dexterity and visualisation inside the body, and reduce the degree of movement during operations [33].
Technological advances in the 1980s led minimally invasive procedures to become an established approach across several surgical techniques. Minimally invasive surgery (MIS) uses smaller incisions or openings than conventional surgery. While this provides several advantages over traditional open surgery (e.g., quicker recovery times), the surgeon is limited by a lack of sensory feedback and a very restricted range of motion [92]. Surgical robots for MIS were developed to address these challenges with the first surgical robot introduced in 1985, a Puma 560 industrial robot modified to be used to define the trajectory of a brain biopsy [3].
The introduction of surgical robots gave rise to new innovation to support MIS, including the laparoscopic assistant robotic system (LARS) created at the IBM Watson Research Center [164] and the robot assisted microsurgery (RAMS) workstation developed at the NASA’s Jet Propulsion Laboratory [165]. Among the most significant innovation of these robots was the introduction of a workstation to allow the surgeon to control a robotic arm using a small joystick. Eventually, the idea of controlling robotic arms to perform laparoscopic surgery from a teleoperated workstation resulted in the Computer Motion’s Zeus robot [166]. Zeus was withdrawn from the market in 2003 and replaced by the da Vinci robot from Intuitive Surgical Inc [167].
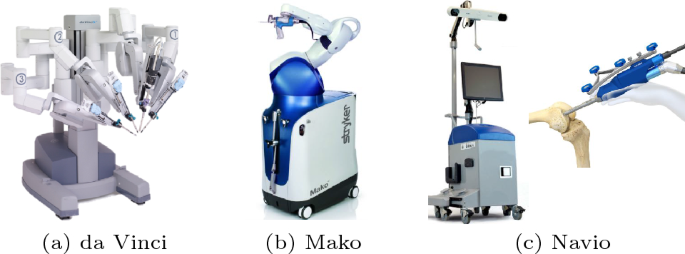
The da Vinci system consists of a surgeon’s console and a patient-side cart (Fig. 6a) with three to four robotic arms teleoperated by the surgeon to allow him to manipulate a full range of instruments (e.g., clamping, dissecting, suturing, etc.). Da Vinci is used in a wide variety of surgical procedures, including urological and cardiac procedures with more than 4500 systems sold worldwide [34]. Since its introduction, a number of commercial surgical robots have been developed, examples are summarised in Table 2. Additionally, a summary of clinical, experimental and commercial systems is available in [13, 34].
Most robots for MIS are teleoperated over a short distance. However, semi-autonomous systems also exist. The Mako robot (Fig. 6b), for example, is a semi-autonomous orthopaedic surgery robot used for knee replacement [178]. Mako uses preoperative CT scans to build a model of the patient’s knee to plan the surgery. The system generates virtual constraints to guide the surgeon in the milling operations and avoid burring the bone outside the predefined areas [179]. A different example of a semi-autonomous robot used in orthopaedic surgery is Navio [175], from Smith & Nephew (Fig. 6c). Navio is a telerobot designed to assist surgeons with knee replacement surgery without requiring a CT scan to plan the surgery. Instead, during the procedure, Navio builds a 3D model of the patient’s knee. This information helps the surgeon determine the correct size and position of the implant.
The successful introduction of robots in orthopaedic surgery is possible thanks to the rigid nature of bones and consistent imaging registration. However, this success does not translate into MIS involving soft tissue manipulation, where robots have not delivered on its early promise, with studies divided on their overall benefits [180, 181].
From one generation to the next surgical robots improve dexterity and precision, reduce invasiveness and tissue damage [34]. The concept of minimal invasiveness has resulted in the evolution of new types of flexible and steerable robots that require only one opening (single-port surgery) or no artificial opening of the skin (e.g., umbilical incision) [182, 183]. Recent advances in miniaturisation methodologies have also contributed to the use of robots in ear, nose, and throat microsurgical procedures, which typically require submillimetric accuracy [34].
Although flexible robots are promising, new advances in miniaturised robotics are paving the way toward the next generation of interventional robots. In this vein, wireless capsule endoscopes were introduced for gastrointestinal diagnosis. Once swallowed, capsule endoscopes move through the gastrointestinal tract to perform diagnosis using visual and biopsy information [184]. These devices are only a few centimetres in size.
In recent years, micro- and nano-robots have been developed for diagnostic and therapeutic purposes. Micro- and nano-robots have the potential to crash kidney stones with little harm and side effects [185], detect a cancer cell and deliver targeted medication [185, 186], destroy microbiological pathogens, or even reverse the effect of genetic diseases by replacing entire chromosomes [187, 188]. Although there are many studies investigating the use of micro- and nano-robots for different biomedical applications, there are still many significant challenges for implementing this technology in real-life applications [188].
Needle placement for percutaneous procedures have also become common in interventional robotics. The process involves the use of patients’ images to plan needle trajectories [189]. Robot-assisted needle placement procedures are used for drainage, tumour destruction, aspirations, local drug delivery, biopsies and automated suturing [13, 189,190,191]. Other applications of interventional robotics include oral surgery [192], ophthalmologic interventions [193], radiation therapy [191] and catheterisation [194]. Furthermore, during the COVID-19 pandemic, autonomous and teleoperated oropharyngeal swab robots were introduced to help medical staff to perform COVID-19 swab sampling without close contact with patients [195, 196]. Additional information on interventional robotics is available in the many available reviews [13, 34, 92, 184, 189, 191, 194, 197].
Despite a number of achievements demonstrated by interventional robots, only a handful of them have reached a commercialisation stage, and even fewer have been adopted in practice. For a device to be commercially feasible, it must be accepted by third-party payers including the public and private health systems. An issue that limits the adoption of interventional robots is the high cost associated with the acquisition and maintenance of such systems. This is largely attributed to the high development costs related to strict safety and reliability requirements. Future developments in the field will require addressing both clinical and technological challenges, at an accessible cost.
Discussion
Over the last two decades we have seen a wide range of robotic technology and platforms developed to support healthcare and wellbeing. Robots can be used in rehabilitation, psychosocial interventions, physical therapy, convalescence and in support of those with impaired functioning. They have a role in augmenting virtual consultations and workplace training, and can be used to acquire medical and behavioural data to gain quantitative insights into both physical and social behaviour.
An important aspect for robots in healthcare is the connection between technology and people. When robots are deployed within the healthcare system, they need to complement or enhance service provision. To achieve this, it is important that end-users of robots are involved in the research, development and deployment of systems.
The Future of Robotics in Healthcare
In this paper applications of robots in healthcare were divided into five main areas: service, assistive, socially assistive, teleoperated and interventional robots. It is expected that new products and services related to these areas will continue to enter healthcare, and create new opportunities. Within the next five years, we should expect robots to increase their capabilities to autonomously support the clinical workforce in well-defined tasks that require little human intervention/interaction including logistics, pharmacy administration/dispersion and productivity. We should also expect new implementations in aerial delivery of consumables, medications and pathology samples.
Interaction with humans will be more intuitive and enjoyable. SARs will autonomously maintain short-term interactions with staff and patients in well-defined tasks, including workforce training, entertainment and distraction. Ongoing developments in AI will also allow robots in front-of-house and in-home support roles, providing health education, reminders, coaching, helping patients navigate from one spot to another or serving as data collection devices (i.e., interviews).
As a response to COVID-19, teleoperated systems are also expected to attract more attention with mobile telepresence taking a significant role in clinical consultations. Mobile telepresence robots will acquire semi-autonomous functions in navigation and patient-robot interaction, allowing clinicians to use higher-level commands during the teleoperation. Similarly, advances in sensing and navigation will enable mobility aids and smart mobility beds. These systems might allow the operator to issue only high-level commands for complex navigation tasks.
Within the next 5–10 years, robots will be able to extract significant data from wearable and distributed sensors (e.g., heart rate, movement, sleep, etc.) within a controlled environment (e.g., clinics, ageing facilities), to complement the data collected by the robots themselves. Integration of the multi-modal data will be essential for modelling user behaviour and intent. Algorithms developed in that time will allow robots to learn and adapt dynamically to changing environments and users. At the same time, autonomous SARs will be able to maintain longer, repeated interactions in a broader set of domains, including companionship, coaching, social and cognitive support. They will adapt their behaviours to changes over time, including small fluctuations in mood, slow decline or improvement, and sudden unexpected changes in a patient’s health or behaviour.
During this time, robotic dexterous manipulation for everyday objects should be expanded to handle more general objects and tasks. Manipulation capabilities will enable the next level of socially-assistive and telepresence robots required to assess and treat patients. General purpose autonomous physical support is not foreseen within the next 10 years, due to the cost and complexity of the technology.
In surgery, more intuitive interfaces that better estimate the surgeons intent, rather than simply executing the user’s commands should be expected in about 10 years. We should also see significant developments in algorithms to provide appropriate feedback to allow surgeons to feel forces, textures, and other physical properties of a patient. At the same time, wearable robotic systems should be able to provide physical feedback to a human operator.
Finally in the next 10–15 years, we should expect significant developments in micro- and nano-robots, allowing this technology to assist in microsurgeries or the localised delivery of medications.
Introducing new technologies in healthcare is disruptive. For robots to be successful, management and hospital staff must understand not only how the new technology is going to benefit the organisation, but also how it’s going to benefit them and the patients they care for. The following section describes some of the main challenges to be expected when implementing a robots in healthcare.
Key Barriers to the Implementation of Robots in Healthcare
Negative attitudes and concerns from the public, patients and healthcare staff can be a significant barrier to implementation. Specifically, healthcare staff might be opposed to the introduction of robots due to lack of familiarity with technology, perceived threats to professional roles (e.g., job losses), absence of an apparent personal benefit, or lack of trust in the technology [5, 15].
Moreover, there is the question of acceptability by patients, families and informal caregivers. A trusting relationship between the healthcare staff and patients is often perceived to require human input [15]. Robotic applications designed to work in specific settings with limited interaction with people (e.g., service robots) are often received positively, and are perceived as being less difficult to implement than those that were designed to operate in human-dense surroundings [15]. Robotic applications designed to support healthcare staff and do not replace them receive higher levels of acceptance [16].
The next barriers are related to cost. Commercially available robots are few and expensive, limiting their usability to organisation with significant purchasing power. As the technology matures, it is expected that an increase in demand may cause a decline in direct costs. Financial challenges, however, should also include considerations beyond capital expenditure, including ongoing costs, potential risks associated with the new technology, and potential impacts in associated areas within the organisation.
For robots to reach their full potential they must be integrated into an organisation’s current workflow, systems and physical spaces. Ageing infrastructure, as well as space limitation in wards, theatres, corridors, and laboratories can significantly increase the cost and time involved in retrofitting new robots.
The absence of adequate regulation and the difficulty of the legal system keeping up with the rapid pace of technological developments presents significant implementation challenges. Without responsible corporate policies and protocols, many robot capabilities can become a threat to both healthcare staff and patients. However, as noted by Dr Kathrin Cresswell [15], “while regulation is important, it should be designed in a way that promotes routine use without stifling innovation.”
The next barrier is related to the longitudinal use of robots. While real-world applications require repeated interactions over extended periods of time, many of the current studies in human-robot interaction (HRI) in healthcare contexts are focused on short-term interactions between humans and robots. Additional research in the longitudinal impact of robots in healthcare are required to improve efficacy, trust and acceptability by the different stakeholders.
Technical challenges are not to be ignored. Advances in battery performance, sensing capabilities, processing power, learning capabilities (i.e., AI), and data communication are key for ongoing innovation. In addition, strong digital foundations are required to manage advanced robotic innovation. Limited technical skills in hospital staff might be an issue to uptake, particularly if significant technical support is needed during or after implementation.
Key Recommendations to the Implementation of Robots in Healthcare
The application of robots in healthcare has large potential benefits. The main recommendation is therefore to further develop this area through evidence-based research and implementation programmes. More specifically, the key areas of consideration when implementing robots in healthcare are:
Innovation
The field of robotics in healthcare is still in its infancy, with only a few products commercially available. Future innovation should incorporate not only basic research, but also practical applications that ensure effective translation of research into practice. Comprehensive analysis of needs and user acceptance should be explored as part of new projects. Ideally, projects that investigate short-term practical applications as well as long-term opportunities should be considered.
Usability
Robots that are difficult to use have a high likelihood of being abandoned. There are two main ways to address this issue. One approach is to reduce robot complexity and create robots that are easier to use and maintain. The other is to improve user interfaces through inclusive design principles (e.g., co-design) that allow for user-friendly interfaces. Either way, all new systems should undergo user testing evaluations before their implementation.
Acceptability
The appearance, behavior, and functionality of robots plays a major role in their adoption and sustained use. Roboticists are usually concerned about a robot’s functional capabilities. However, there is great value in also considering a robot’s appearance and behavior to improve technology adoption. While humanoid robots are often preferred in order to provide a similar interactive experience to that currently available through clinicians, human-like robots often fall short of human expectations, resulting in disappointment and mistrust [18].
Acceptance and trust towards robots in healthcare will improve through exposure, communication, education and appropriate management of expectations. As success stories of robots become more visible, robots are likely to become more acceptable in healthcare. Acceptance from both hospital staff and patients in needed for widespread adoption. At the moment, acceptability of robots in healthcare varies widely. The prospect that robots may take over healthcare jobs is of particular concern [16, 198]. Augmenting human capabilities and empowering professionals instead of replacing them is generally more accepted. Nevertheless, greater reliance on robots is likely to have impacts in the short, medium, and long term and that must be managed responsibly.
Privacy, Reliability and Safety
Robots in healthcare work in close proximity to people who may be vulnerable to harm due to disability, injury, or illness. When robots and people are proximately located, safety and reliability are incredibly important. While there is significant work looking at safe physical human-robot interaction (e.g., collision avoidance), there is little work available in cognitive or emotional safety. That is, ensuring that the appearance of the robot is well-aligned with its functions to avoid deception, or considerations around how the robot manages users’ data to maintain privacy and dignity.
Training and Education
End-users (either staff or patients) need to be brought onboard with the technology, how it works and what are its limitations. If users do not know how to use these robots, or what their limitations are, then the implementation will not be effective. Interdisciplinary programs that bridge medical and engineering training at the university level might be beneficial.
Clinical Efficacy
For robots to be clinically effective they should benefit patients, clinicians or both. This question should be answered thorough evidence-based studies. These studies should evaluate technology reliability, reproducibility of experiments, safety, usability, acceptability and generalisation of outcomes. As systems become increasingly intelligent and autonomous, it might be necessary to develop methods for measuring and evaluating adaptive technologies that change along with robots. Longitudinal evaluations of implementation (translation from research to practice), adoption, and optimisation should be considered.
Depending on the application, robots might need to undergo regulatory approvals (e.g., FDA). Particular attention needs to be given to an organisation’s current workflow, and how robots will be integrated without significant disruption.
Cost
When a robot is being acquired, it is important to consider its costs beyond the purchase and maintenance, including the impacts in infrastructure, clinical workflow and other unintended consequences. That is, we should ensure the selected robot can be installed in available spaces, meets clinical needs without increasing workflow, appropriate plans for implementation and ongoing support are in place, and the safety, reliability and efficacy of the robot are properly evaluated. We should also make sure the organisation and relevant stakeholders are ready for the new technology, with training put in place to minimise the impacts in staff. Finally, we need to ensure the new system is compatible with other products and technologies, and adaptable to ongoing changes within the organisation.
Change Management
There are risks in introducing a new system before it is fully functional, as resistance to an innovation often grows out of mistakes or overlooked issues in an implementation plan. Integration of new technology requires planning, testing, guidance and appropriate change management practices. Ideally, the least disruptive application should be the first one to be implemented.
Deployment
Integration of robots with existing practices is challenging. This process requires clear objectives, detailed plans, and an adequate management of expectations. Success metrics should be determined in advance and evaluated continually. Quality improvement should be supported on an ongoing basis. More importantly, deployment of robots should be considered only after the clinical effectiveness is demonstrated. This process will reduce potential risks for mistrust, frustration and disappointment.
Additionally, key stakeholders should be included and engaged from the onset. In most cases, a clinical champion is recommended to manage expectations. Public engagement campaigns and public dissemination of successful case studies of robots in healthcare could help promote a positive attitude towards robots among staff and patients.
Finally, given that internet connectivity is vital to many of these devices, the provision of a fast and functional internet service is of significant importance.
Conclusions
The application of robotics in healthcare is a relatively new and exciting area driven by the expectation that robots will be able to help address key challenges and introduce efficiencies over the next decades. To date, only a few robots are commercially available and used in large-scale. The most prominent healthcare robots currently in use are service and surgery robots, with many other applications under development. How these robots will be integrated into the healthcare system remains unknown, but there is no doubt that robots will be a major enabler to the delivery of healthcare.
Integrating new robotic systems into healthcare is complex. With the correct strategy, however, large successful technology disruption can be very successful. Prior to the implementation and commercialisation of robots in healthcare, prototype experimental systems have to be refined to be safe, reliable, and appealing to users. The robot’s appearance and behaviour need to be adequate, and fit within the proposed application. Concrete measures of system performance and cost effectiveness need to be considered. Feasibility, impact, and economic evaluations need to be undertaken to confirm usability and acceptability. Robots that support hospital staff to enhance service delivery rather than to exclude or replace them are more likely to be accepted. Ultimately, wide-spread adoption of robots is not likely until there is evidence of beneficial long-term impacts.
The main objective of this paper was to chart key opportunities and considerations for implementing robots in healthcare. The identification of the main drivers, challenges and opportunities for robots in healthcare can be used to inform strategic directions to maximise quality, acceptability, safety and availability of the technology. Finally, this document should not be seen a comprehensive review to the field, but as a stepping stone to stimulate wider discussions surrounding robots in healthcare.
Data availability
Not applicable.
Code availability
Not applicable.
References
Siciliano B, Khatib O. Springer handbook of robotics. In: Siciliano B, Khatib O, editors. 2nd ed. Switzerland: Springer International Publishing; 2016.
World Health Organization (WHO). Global spending on health: a world in transition 2019. Global Report. 2019. p. 49.
Kwoh YS, Hou J, Jonckheere EA, Hayati S. A robot with improved absolute positioning accuracy for CT guided stereotactic brain surgery. IEEE Trans Biomed Eng. 1988;35(2):153–60.
Kaiser MS, Mamun SA, Mahmud M, Tania MH. Healthcare robots to Combat COVID-19. Lecture notes on data engineering and communications technologies. 60th ed. Singapore: Springer; 2021. p. 14.
Kyrarini M, Lygerakis F, Rajavenkatanarayanan A, Sevastopoulos C, Nambiappan HR, Chaitanya KK, et al. A Survey of Robots in Healthcare. Technologies. 2021;9:8.
Müller C. International Federation of Robotics Press Conference; 2019.
Khan ZH, Siddique A, Lee CW. Robotics utilization for healthcare digitization in global COVID-19 management. Int J Environ Res Public Health. 2020;17:11.
Dickstein-Fischer LA, Crone-Todd DE, Chapman IM, Fathima AT, Fischer GS. Socially assistive robots: current status and future prospects for autism interventions. Innov Entrep Health. 2018;5:15–25. https://doi.org/10.2147/ieh.s138753.
Shi D, Zhang W, Zhang W, Ding X. A review on lower limb rehabilitation exoskeleton robots. Chin J Mech Eng (English Edition). 2019;32(74):11. https://doi.org/10.1186/s10033-019-0389-8.
Conti D, Nuovo AD. Social robots for older users: a possibility to support assessment and social interventions. In: CEUR workshop proceedings. 2019. p. 1–8.
Abdi J, Al-Hindawi A, Ng T, Vizcaychipi MP. Scoping review on the use of socially assistive robot technology in elderly care. BMJ Open. 2018;8: e018815. https://doi.org/10.1136/bmjopen-2017-018815.
Mois G, Beer JM. Robotics to support aging in place. In: Living with robots, emerging issues on the psychological and social implications of robotics. Elsevier Inc.; 2020. p. 49–74.
Avgousti S, Christoforou EG, Panayides AS, Voskarides S, Novales C, Nouaille L, et al. Medical telerobotic systems: current status and future trends. BioMed Eng Online. 2016;15:1–44. https://doi.org/10.1186/s12938-016-0217-7.
Whelan S, Murphy K, Barrett E, Krusche C, Santorelli A, Casey D. Factors affecting the acceptability of social robots by older adults including people with dementia or cognitive impairment: a literature review. Int J Soc Robot. 2018;10:643–68. https://doi.org/10.1007/s12369-018-0471-x.
Dolic Z, Castro R, Moarcas A. Robots in healthcare: a solution or a problem? European Parliament Policy Department for Economic, Scientific and Quality of Life Policies Directorate-General for Internal Policies. 2019.
Aizcorbe JI. A review on human robot collaboration and its application in the health care sector. University of Applied Sciences (Hochschule Niederrhein); 2020.
Silvera-Tawil D, Roberts-Yates C. Socially-assistive robots to enhance learning for secondary students with intellectual disabilities and autism. In: IEEE International symposium on robot and human interactive communication. 2018. p. 838–843.
Cresswell K, Cunningham-Burley S, Sheikh A. Health care robotics: qualitative exploration of key challenges and future directions. J Med Internet Res. 2018;20(7):1–11. https://doi.org/10.2196/10410.
Riek LD. Healthcare robotics. Commun ACM. 2017;60(11):68–78. https://doi.org/10.1145/3127874. arXiv:1704.03931.
Bekey G, Ambrose R, Kumar V, Sanderson A, Wilcox B, Zheng Y. International assessment of research and development in robotics. National Science Foundation; 2006. http://www.wtec.org/robotics/report/screen-robotics-final-report.pdf.
Hägele M, Nilsson K, Pires JN, Bischoff R. Industrial robotics. In: Siciliano B, Khatib O, editors. Springer handbook of robotics. Berlin: Springer International Publishing; 2016. p. 1385–422.
Sprenger M, Mettler T. Service robots. Bus Inf Syst Eng. 2015;57(4):271–4. https://doi.org/10.1007/s12599-015-0389-x.
Guizzo E. World robot population reaches 8.6 million. https://spectrum.ieee.org/automaton/robotics/industrial-robots/world-robot-population-chart.
Keay S. A robotics roadmap for Australia 2018. Australian Centre for Robotic Vision; 2018.
Butter M, Rensma A, van Boxsel J, Kalisingh S, Schoone M, Leis M, et al. Robotics for healthcare. European Commission, DG Information Society; 2008.
World Population Ageing. United Nations: Department of Economic and Social Affairs; 2019.
Vos T. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(9995):743–800. https://doi.org/10.1016/S0140-6736(15)60692-4.
Australian Institute of Health and Welfare. Australia’s health 2018; 2018. https://www.aihw.gov.au/reports/australias-health/australias-health-2018-in-brief/contents/how-healthy-are-we.
Health Workforce Australia. Australia’s future health workforce—Nurses detailed report. 2014. https://www.health.gov.au/resources/publications/nurses-australias-future-health-workforce-reports.
Lee JY, Song YA, Jung JY, Kim HJ, Kim BR, Do HK, et al. Nurses’ needs for care robots in integrated nursing care services. J Adv Nurs. 2018;74(9):2094–105. https://doi.org/10.1111/jan.13711.
Scheunemann LP, White DB. The ethics and reality of rationing in medicine. Chest. 2011;140(6):1625–32. https://doi.org/10.1378/chest.11-0622.
Keliddar I, Mosadeghrad AM, Jafari-Sirizi M. Rationing in health systems: a critical review. Med J Islam Repub Iran. 2017;31(1):271–277. https://doi.org/10.14196/MJIRI.31.47.
National Science Foundation. A roadmap for US robotics: from internet to robotics. National Science Foundation, University of California San Diego, Oregon State University, Georgia Institute of Technology; 2016.
Troccaz J, Dagnino G, Yang GZ. Frontiers of medical robotics: From concept to systems to clinical translation. Annu Rev Biomed Eng. 2019;21(1):193–218. https://doi.org/10.1146/annurev-bioeng-060418-052502.
Gerling GJ, Rigsbee S, Childress RM, Martin ML. The design and evaluation of a computerized and physical simulator for training clinical prostate exams. IEEE Trans Syst Man Cybern Part A Syst Hum. 2009;39(2):388–403. https://doi.org/10.1109/TSMCA.2008.2009769.
Huang Z, Lin C, Kanai-Pak M, Maeda J, Kitajima Y, Nakamura M, et al. Impact of using a robot patient for nursing skill training in patient transfer. IEEE Trans Learn Technol. 2017;10(3):355–66. https://doi.org/10.1109/TLT.2016.2599537.
Hashimoto T, Morita K, Kato N, Kobayashi H, Nakane H. Depression patient robot for diagnostic training in psychiatric education. In: IEEE/ASME international conference on advanced intelligent mechatronics. IEEE; 2011. p. 134–139.
Noh Y, Ebihara K, Segawa M, Sato K, Wang C, Ishii H, et al. Development of the airway management training system WKA-4: for improved high-fidelity reproduction of real patient conditions, and improved tongue and mandible mechanisms. In: IEEE international conference on robotics and automation. IEEE; 2011. p. 1726–1731.
Niemeyer G, Preusche C, Stramigioli S, Lee D. Telerobotics. In: Siciliano B, Khatib O, editors. Springer handbook of robotics. Berlin: Springer; 2016. p. 1085–108.
Australian Department of Health. National strategic framework for rural and remote health, rural health standing committee; 2016. https://www1.health.gov.au/internet/main/publishing.nsf/Content/national-strategic-framework-rural-remote-health.
Amukele T, Ness PM, Tobian AAR, Boyd J, Street J. Drone transportation of blood products. Transfus Pract. 2017;57(3):582–8. https://doi.org/10.1111/trf.13900.
Sherwood D. This Chilean community is using drones to deliver medicine to the elderly. https://www.weforum.org/agenda/2020/04/drone-chile-covid19/.
Hussain K, Wang X, Omar Z, Elnour M, Ming Y. Robotics and artificial intelligence applications in manage and control of COVID-19 pandemic. In: International conference on computer, control and robotics; 2021. p. 66–69.
Wang XV, Wang L. A literature survey of the robotic technologies during the COVID-19 pandemic. J Manuf Syst. 2021. https://doi.org/10.1016/j.jmsy.2021.02.005.
Therapeutic Goods Administration. Regulation of software as a medical device. https://www.tga.gov.au/regulation-software-medical-device.
Alexander FG, Petrie JR, Bergenstal RM, Holl RW, Peters AL, Heinemann L. Diabetes digital app technology: benefits, challenges, and recommendations. A consensus report by the European Association for the Study of Diabetes (EASD) and the American Diabetes Association (ADA) Diabetes Technology Working Group. Diabetes Care. 2020;43(1):250–60. https://doi.org/10.2337/dci19-0062.
Sheppard MK. mHealth apps: disruptive innovation, regulation, and trust—a need for balance. Med Law Rev. 2020;28(3):549–72. https://doi.org/10.1093/medlaw/fwaa019.
Myagmarbayar N, Yuki Y, Imamoglu N, Gonzalez J, Otake M, Yu W. Human body contour data based activity recognition. In: Annual international conference of the IEEE engineering in medicine and biology society. 2013. p. 5634–5637.
Rodriguez Lera FJ, Martín Rico F, Guerrero Higueras AM, Olivera VM. A context-awareness model for activity recognition in robot-assisted scenarios. Expert Syst. 2020;37(2): e12481. https://doi.org/10.1111/exsy.12481.
Alam F, Mehmood R, Katib I, Albogami NN, Albeshri A. Data fusion and IoT for smart ubiquitous environments. IEEE Access. 2017;5:9533–54.
Nweke HF, Teh YW, Mujtaba G, Al-garadi MA. Data fusion and multiple classifier systems for human activity detection and health monitoring: review and open research directions. Inf Fusion. 2019;46:147–70. https://doi.org/10.1016/j.inffus.2018.06.002.
Martins GS, Santos L, Dias J. User-adaptive interaction in social robots: a survey focusing on non-physical Interaction. Int J Soc Robot. 2019;11:185–205. https://doi.org/10.1007/s12369-018-0485-4.
Haring KS, Silvera-Tawil D, Watanabe K, Velonaki M. The influence of robot appearance and interactive ability in HRI: a cross-cultural study. In: Social robotics. Lecture notes in computer science. Springer; 2016. p. 392–401.
Tucker MR, Olivier J, Pagel A, Bleuler H, Bouri M, Lambercy O, et al. Control strategies for active lower extremity prosthetics and orthotics: A review. J NeuroEng Rehabil. 2015. https://doi.org/10.1186/1743-0003-12-1.
Nelson BJ, Kaliakatsos IK, Abbott JJ. Microrobots for minimally invasive medicine. Annu Rev Biomed Eng. 2010. https://doi.org/10.1146/annurev-bioeng-010510-103409.
World robotics 2015 survey—Executive summary. International Federation of Robotics; 2015.
Philbrick V. Leading the lean healthcare journey: driving culture change to increase value. AORN J. 2012;96(4):456–7. https://doi.org/10.1016/j.aorn.2012.07.006.
Bloss R. Mobile hospital robots cure numerous logistic needs. Ind Robot. 2011;38(6):567–71. https://doi.org/10.1108/01439911111179075.
Özkil AG, Fan Z, Dwids S, Aanaæs H, Kristensen JK, Christensen KH. Service robots for hospitals: a case study of transportation tasks in a hospital. In: IEEE international conference on automation and logistics. 2009. p. 289–294.
Doost A. Robot assists hospitals in the fight against COVID-19. https://fox40.com/news/coronavirus/robot-assists-hospitals-in-the-fight-against-covid-19/.
Wang C, Savkin AV, Clout R, Nguyen HT. An intelligent robotic hospital bed for safe transportation of critical neurosurgery patients along crowded hospital corridors. IEEE Trans Neural Syst Rehabil Eng. 2015;23(5):744–54. https://doi.org/10.1109/TNSRE.2014.2347377.
Wang C, Matveev AS, Savkin AV, Clout R, Nguyen HT. A semi-autonomous motorized mobile hospital bed for safe transportation of head injury patients in dynamic hospital environments without bed switching. Robotica. 2016;34(8):1880–97. https://doi.org/10.1017/S0263574714002641.
Willach. Australia’s leading dispensary automation technology at your fingertips! https://willach.com.au/.
Omnicell. Robomat Robotic Dispensing System. www.omnicell.com/products/robomat-robotic-dispensing-system.
Diligent Robotics. Moxi. https://diligentrobots.com/moxi.
Aethon. TUG: Change Healthcare. https://aethon.com/mobile-robots-for-healthcare/.
Keenon. Start at one touch: Delivery RobotT1. www.keenonrobot.com/en/Product/pro2.html.
Aim Lab. PathFinder 350A. www.aimlab.com/pathology-automation/?doing_wp_cron=1573019037.7309820652008056640625.
Beckman Coulter. AutoMate 2500. www.beckmancoulter.com/en/products/automation/automate-2500-family-sample-processing-systems.
UVD Robots. The only disinfection system clinically proven to disinfect effectively while ’on the move’. www.uvd-robots.com/robots.
Akara Robotics. Cleaning reimagined. www.akara.ai/.
Invento Robotics. C-Astra for disinfection. https://mitrarobot.com/covid/#profile.
Australian Civil Aviation Safety Authority. Drones. www.casa.gov.au/drones.
Wang C, Noh Y, Ebihara K, Terunaga C, Tokumoto M, Okuyama I, et al. Development of an arm robot for neurologic examination training. In: IEEE international conference on intelligent robots and systems. 2012. p. 1090–1095.
Kitagawa Y, Ishikura T, Song W, Mae Y, Minami M, Tanaka K. Human-like patient robot with chaotic emotion for injection training. In: ICCAS-SICE joint conference. 2009. p. 6.
Takanobu H, Omata A, Takahashi F, Yokota K, Suzuki K, Miura H, et al. Dental patient robot as a mechanical human simulator. In: IEEE international conference on mechatronics. 2007. p. 5.
Holland LL, Smith LL, Blick KE. Total laboratory automation can help eliminate the laboratory as a factor in emergency department length of stay. Am J Clin Pathol. 2006;125(5):765–70. https://doi.org/10.1309/3J5P9VJRUP4U5RU5.
Popovic MB. Feeding systems, assistive robotic arms, robotic nurses, robotic massage. In: Biomechatronics. Elsevier; 2019. p. 419–430.
Andreopoulos A, Tsotsos JK. Active vision for door localization and door opening using Playbot: a computer controlled wheelchair for people with mobility impairments. In: IEEE Canadian conference on computer and robot vision; 2008. p. 10.
Maalouf N, Sidaoui A, Elhajj IH, Asmar D. Robotics in nursing: a scoping review. J Nurs Scholarsh. 2018;50(6):590–600. https://doi.org/10.1111/jnu.12424.
Topping M. An overview of the development of Handy 1, a rehabilitation robot to assist the severely disabled. J Intell Robot Syst Theory Appl. 2002;34:253–63. https://doi.org/10.1023/A:1016355418817.
Desin Robotics. Obi, the first dining robot of its kind. https://meetobi.com/.
Neater Solutions. Neater Eater. https://neater.co.uk/.
Leaman J, La HM. A comprehensive review of smart wheelchairs: past, present, and future. IEEE Trans Hum-Mach Syst. 2017;47(4):486–489. https://doi.org/10.1109/THMS.2017.2706727. arXiv:1704.04697.
Heater B. Toyota and Dean Kamen are bringing back the iBOT motorized, stair-climbing wheelchair. https://techcrunch.com/2016/05/23/ibot-wheelchair/.
Ji Y, Hwang J, Kim EY. An intelligent wheelchair using situation awareness and obstacle detection. Proc Soc Behav Sci. 2013;97:620–8. https://doi.org/10.1016/j.sbspro.2013.10.281.
Robotikworld. LEA (The Lean Empowering Assistant). http://www.robotikworld.com/lea/.
Spenko M, Yu H, Dubowsky S. Robotic personal aids for mobility and monitoring for the elderly. IEEE Trans Neural Syst Rehabil Eng. 2006;14(3):344–51. https://doi.org/10.1109/TNSRE.2006.881534.
Bilyea A, Seth N, Nesathurai S, Abdullah HAA. Robotic assistants in personal care: a scoping review. Med Eng Phys. 2017;49:1–6. https://doi.org/10.1016/j.medengphy.2017.06.038.
Ktistakis IP, Bourbakis NG. A survey on robotic wheelchairs mounted with robotic arms. In: IEEE national aerospace electronics conference. 2016. p. 258–262. https://doi.org/10.1109/NAECON.2015.7443079.
Kinova. Kinova Jaco Assistive Robotic Arm. https://www.kinovarobotics.com/en/assistive-technologies/column-a1/kinova-assistive-robotic-arm.
Kim J, Gu GM, Heo P. Robotics for healthcare. In: Jo H, Jun HW, Shin J, Lee SH, editors. Biomedical engineering: frontier research and converging technologies, Biosystems & Biorobotics, vol. 9. Springer; 2016. p. 1–511.
Witteveen HJB, Droog EA, Rietman JS, Veltink PH. Vibro- and electrotactile user feedback on hand opening for myoelectric forearm prostheses. IEEE Trans Biomed Eng. 2012;59(8):2219–26. https://doi.org/10.1109/TBME.2012.2200678.
Sharbafi M, Naseri A, Seyfarth A, Grimmer M. Neural control in prostheses and exoskeletons. In: Dallali H, Demircan E, Rastgaar M, editors. Powered prostheses. Amsterdam: Elsevier Inc.; 2020. p. 153–78.
Rehmat N, Zuo J, Meng W, Liu Q, Xie SQ, Liang H. Upper limb rehabilitation using robotic exoskeleton systems: a systematic review. Int J Intell Robot Appl. 2018;2(3):283–95. https://doi.org/10.1007/s41315-018-0064-8.
Hocoma. Hocoma: Advanced Technologies for Movement Rehabilitation. https://www.hocoma.com/.
Szondy D. Robear robot care bear designed to serve Japan’s aging population. https://newatlas.com/robear-riken/36219/.
Böhlen M, Karppi T. The making of Robot Care. Transformations. 2017;29:22.
Michaud F, Theberge-Turmel C. Mobile robotic toys and autism. In: Dautenhahn K, Bond A, Cañamero L, Edmonds B, editors. Socially intelligent agents: creating relationships with computers and robots, Multiagent systems, artificial societies, and simulated organizations. vol. 3. Boston: Springer; 2002. p. 125–132.
Feil-Seifer D, Matarić MJ. Toward socially assistive robotics for augmenting interventions for children with Autism Spectrum Disorders. In: Kumar OKV, Pappas GJ, editors. Experimental, Springer Tracts in Advanced Robotics, vol. 54. Springer; 2009. p. 15.
Genocchi B, Lenk K, Hyttinen J. An overview of assistive robotics and technologies for elderly care. In: MEDICON. Springer International Publishing; 2019. p. 971–976.
Shukla J, Cristiano J, Oliver J, Puig D. Robot assisted interventions for individuals with intellectual disabilities: impact on users and caregivers. Int J Soc Robot. 2019;11(4):631–49. https://doi.org/10.1007/s12369-019-00527-w.
Silvera-Tawil D, Bradford D, Roberts-Yates C. Talk to me: the role of human-robot interaction in improving verbal communication skills in students with autism or intellectual disability. In: IEEE international symposium on robot and human interactive communication. 2018. p. 1–6.
Petersen S, Houston S, Qin H, Tague C, Studley J. The utilization of robotic pets in dementia care. J Alzheimer’s Dis. 2017;55(2):569–74. https://doi.org/10.3233/JAD-160703.
Ras BR. Mabu helps patients with chronic health issues manage their treatment. https://www.goodnet.org/articles/this-small-robot-helps-take-care-patients.
Catalia Health. Mobu: Leading Remote Care Management. http://www.cataliahealth.com/.
Aflac. My Special Aflac Duck. https://www.aflacchildhoodcancer.org/.
Abou Allaban A, Wang M, Padır T. A systematic review of robotics research in support of in-home care for older adults. Information. 2020;11(75):23. https://doi.org/10.3390/info11020075.
Diehl JJ, Crowell CR, Villano M, Wier K, Tang K, Riek LD. Clinical applications of robots in autism spectrum disorder diagnosis and treatment. In: Patel VB, Preedy VR, Martin CR, editors. Comprehensive guide to autism. New York: Springer; 2014. p. 411–22.
Scassellati B, Henny A, Matarić M, Admoni H. Robots for use in autism research. Annu Rev Biomed Eng. 2012;14(1):275–94.
Vanderborght B, Simut R, Saldien J, Pop C, Rusu AS, Pintea S, et al. Using the social robot probo as a social story telling agent for children with ASD. Interact Stud. 2012;13(3):348–72. https://doi.org/10.1075/is.13.3.02van.
Warren ZE, Zheng Z, Swanson AR, Bekele E, Zhang L, Crittendon JA, et al. Can robotic interaction improve joint attention skills? J Autism Dev Disord. 2013;45(11):3726–34. https://doi.org/10.1007/s10803-013-1918-4.
Robins B, Dautenhahn K, Te Boekhorst R, Billard A. Robotic assistants in therapy and education of children with autism: can a small humanoid robot help encourage social interaction skills? Univ Access Inf Soc. 2005;4(2):105–20.
Robins B, Dautenhahn K. Developing play scenarios for tactile interaction with a humanoid robot: a case study exploration with children with autism. In: Social Robotics, Lecture Notes in Computer Sciencevol. 6414. Springer; 2010. p. 243–252.
Scoglio AA, Reilly ED, Gorman JA, Drebing CE. Use of social robots in mental health and well-being research: systematic review. J Med Internet Res. 2019;21(7): e13322. https://doi.org/10.2196/13322.
Costescu CA, Vanderborght B, David DO. The effects of robot-enhanced psychotherapy: a meta-analysis. Rev Gen Psychol. 2014;18(2):127–36. https://doi.org/10.1037/gpr0000007.
Short E, Swift-Spong K, Greczek J, Ramachandran A, Litoiu A, Grigore EC, et al. How to train your DragonBot: socially assistive robots for teaching children about nutrition through play. In: IEEE international symposium on robot and human interactive communication. 2014. p. 924–929.
Henkemans OAB, Bierman BPB, Janssen J, Looije R, Neerincx MA, van Dooren MMM, et al. Design and evaluation of a personal robot playing a self-management education game with children with diabetes Type 1. Int J Hum Comput Stud. 2017;106:63–76. https://doi.org/10.1016/j.ijhcs.2017.06.001.
Alemi M, Ghanbarzadeh A, Meghdari A, Moghadam LJ. Clinical application of a humanoid robot in pediatric cancer interventions. Int J Soc Robot. 2016;8(5):743–59. https://doi.org/10.1007/s12369-015-0294-y.
Kidd CD, Breazeal C. Robots at home: Understanding long-term human-robot interaction. In: IEEE/RSJ international conference on intelligent robots and systems. 2008. p. 3230–3235.
Görer B, Salah AA, Akın HL. A robotic fitness coach for the elderly. In: Ambient Intelligence, Lecture Notes in Computer Science, vol. 8309. Springer; 2013. p. 124–139.
Buitrago JA, Bolaños AM, Caicedo Bravo E. A motor learning therapeutic intervention for a child with cerebral palsy through a social assistive robot. Disabil Rehabil Assist Technol. 2020;15(3):357–62. https://doi.org/10.1080/17483107.2019.1578999.
Lins AA, de Oliveira JM, JPC Rodrigues J, de Albuquerque VCH, P C Rodrigues JJ. Robot-assisted therapy for rehabilitation of children with Cerebral Palsy—a complementary and alternative approach. Comput Hum Behav. 2019;100:152–167. https://doi.org/10.1016/j.chb.2018.05.012.
Malik NA, Yussof H, Hanapiah FA, Rahman RAA, Basri HH. Human-robot interaction for children with cerebral palsy: reflection and suggestion for interactive scenario design. Proc Comput Sci. 2015;76:388–93. https://doi.org/10.1016/j.procs.2015.12.315.
Ozeki T, Mouri T, Sugiura H, Yano Y, Miyosawa K. Use of communication robots to converse with people suffering from Schizophrenia. Robomech J. 2020;7(13):14. https://doi.org/10.1186/s40648-020-00161-6.
Pascher M, Baumeister A, Klein B, Schneegass S, Pascher M, Baumeister A, et al. Little helper: a multi-robot system in home health care environments. In: International workshop on human-drone interaction as part of the ACM conference on human factors in computing systems. 2019. p. 8.
Fischinger D, Einramhof P, Papoutsakis K, Wohlkinger W, Mayer P, Panek P, et al. Hobbit, a care robot supporting independent living at home: first prototype and lessons learned. Robot Auton Syst. 2016;75:60–78. https://doi.org/10.1016/j.robot.2014.09.029.
Asus. Zenbo—Your smart little companion. https://zenbo.asus.com/.
Buddy. Buddy, the emotional robot. https://buddytherobot.com/en/buddy-the-emotional-robot/.
Fraunhofer Institute for Manufacturing Engineering and Automation1. Care-O-bot 4. https://www.care-o-bot.de/en/care-o-bot-4.html.
Martinez-Martin E, Pobil AP. Personal robot assistants for elderly care: an overview. In: Personal assistants: emerging computational technologies, Intelligent Systems Reference Library, vol. 132. Springer; 2018. p. 77–91.
Volkhardt M, Gross HM. Finding people in apartments with a mobile robot. In: IEEE international conference on systems, man, and cybernetics. 2013. p. 4348–4353.
Wieser I, Toprak S, Grenzing A, Hinz T, Auddy S, Can Karaoğuz E, et al. A robotic home assistant with memory aid functionality. In: Friedrich G, Helmert M, Wotawa F, editors. KI 2016: advances in artificial intelligence, lecture notes in computer science, vol. 9904. Springer; 2016. p. 102–115.
Fernbach N, Rafferty S. Townsville Hospital hosts humanoid robot in Australian first trial. https://www.abc.net.au/news/2018-08-24/townsville-hospital-trials-robot-helper/10157200.
Ahn HS, Yep W, Lim J, Ahn BK, Johanson DL, Hwang EJ, et al. Hospital Receptionist Robot v2: design for enhancing verbal interaction with social skills. In: IEEE international conference on robot and human interactive communication. 2019. p. 6.
Johanson DL, Ahn HS, Sutherland CJ, Brown B, MacDonald BA, Lim JY, et al. Smiling and use of first-name by a healthcare receptionist robot: Effects on user perceptions, attitudes, and behaviours. Paladyn. 2020;11(1):40–51. https://doi.org/10.1515/pjbr-2020-0008.
Johnston M. Sydney Hospital trials multilingual wayfinding robot. https://www.itnews.com.au/news/sydney-hospital-deploys-multilingual-wayfinding-robot-539227.
Ahn HS, Datta C, Kuo IH, Stafford R, Kerse N, Peri K, et al. Entertainment services of a healthcare robot system for older people in private and public spaces. In: International conference on automation, robotics and applications. IEEE; 2015. p. 217–222.
Dawe J, Sutherland C, Barco A, Broadbent E. Can social robots help children in healthcare contexts? A scoping review. BMJ Paediatr Open. 2019;3(1): e000371. https://doi.org/10.1136/bmjpo-2018-000371.
Johnston C. Canberra Hospital’s most entertaining employee. https://www.act.gov.au/our-canberra/latest-news/2018/august/canberra-hospitals-most-entertaining-employee.
Beran TN, Ramirez-Serrano A, Vanderkooi OG, Kuhn S. Reducing children’s pain and distress towards flu vaccinations: a novel and effective application of humanoid robotics. Vaccine. 2013;7(31):2772–7. https://doi.org/10.1016/j.vaccine.2013.03.056.
Tasaki R, Kitazaki M, Miura J, Terashima K. Prototype design of medical round supporting robot ‘Terapio’. In: IEEE international conference on robotics and automation. IEEE; 2015. p. 829–834.
Aymerich-Franch L, Ferrer I. The implementation of social robots during the COVID-19 pandemic. 2020. p. 10.
Conti D, Nuovo S, Nuovo AD, Di Nuovo S, Buono S, Buono S, et al. Robots in education and care of children with developmental disabilities: a study on acceptance by experienced and future professionals. Int J Soc Robot. 2017;9(1):1–12. https://doi.org/10.1007/s12369-016-0359-6.
Robinson NL, Cottier TV, Kavanagh DJ. Psychosocial health interventions by social robots: systematic review of randomized controlled trials. J Med Internet Res. 2019;21(5): e13203. https://doi.org/10.2196/13203.
Krishna JR. Telerobotic surgery: transcending barriers. World J Laparosc Surg. 2017;10(2):57–60. https://doi.org/10.5005/jp-journals-10033-1304.
Marescaux J, Leroy J, Rubino F, Smith M, Vix M, Simone M, et al. Transcontinental robot-assisted remote telesurgery: feasibility and potential applications. Ann Surg. 2002;235(4):487–92. https://doi.org/10.1097/00000658-200204000-00005.
Evans CR, Medina MG, Dwyer AM. Telemedicine and telerobotics: from science fiction to reality. Updates Surg. 2018;70(3):357–62. https://doi.org/10.1007/s13304-018-0574-9.
Avgousti S, Panayides AS, Christoforou EG, Argyrou A, Jossif A, Masouras P, et al. Medical telerobotics and the remote ultrasonography paradigm over 4G wireless networks. In: IEEE international conference on e-health networking, applications and services, Healthcom. IEEE; 2018. p. 5.
Plazas-Roa ID, Ruiz-Olaya AF. A tele-robotic system for real-time remote evaluation of upper-limb function. In: IFMBE proceedings. 2015.
Atashzar SF, Polushin IG, Patel RV. A small-gain approach for nonpassive bilateral telerobotic rehabilitation: stability analysis and controller synthesis. IEEE Trans Robot. 2017;33(1):49–66. https://doi.org/10.1109/TRO.2016.2623336.
Ackerman E. iRobot and InTouch Health Announce RP-VITA Telemedicine Robot. IEEE Spectrum. 2012. p. 4.
Smith A. iRobot’s Medical Robot Gets FDA Approval for Hospital Use. MashableAustralia. 2013. p. 5.
Cortellessa G, Fracasso F, Sorrentino A, Orlandini A, Bernardi G, Coraci L, et al. ROBIN, a telepresence robot to support older users monitoring and social inclusion: development and evaluation. Telemed e-Health. 2018;24(2):145–54. https://doi.org/10.1089/tmj.2016.0258.
Agarwal R, Levinson AW, Allaf M, Markov D, Nason A, Su LM. The RoboConsultant: telementoring and remote presence in the operating room during minimally invasive urologic surgeries using a novel mobile robotic interface. Urology. 2007;70(5):970–4. https://doi.org/10.1016/j.urology.2007.09.053.
Gandsas A, Parekh M, Bleech MM, Tong DA. Robotic telepresence: profit analysis in reducing length of stay after laparoscopic gastric bypass. J Am Coll Surg. 2007;205(1):72–7. https://doi.org/10.1016/j.jamcollsurg.2007.01.070.
Vespa PM, Miller C, Hu X, Nenov V, Buxey F, Martin NA. Intensive care unit robotic telepresence facilitates rapid physician response to unstable patients and decreased cost in neurointensive care. Surg Neurol. 2007;67(4):331–7. https://doi.org/10.1016/j.surneu.2006.12.042.
Petelin JB, Nelson ME, Goodman J. Deployment and early experience with remote-presence patient care in a community hospital. Surg Endosc Other Interv Tech. 2007;21(1):53–6. https://doi.org/10.1007/s00464-005-0261-z.
Ellison LM, Nguyen M, Fabrizio MD, Soh A, Permpongkosol S, Kavoussi LR. Postoperative robotic telerounding: a multicenter randomized assessment of patient outcomes and satisfaction. Arch Surg. 2007;142(12):1177–81. https://doi.org/10.1001/archsurg.142.12.1177.
Daruwalla ZJ, Collins DR, Moore DP. “Orthobot, to your station!’’ The application of the remote presence robotic system in orthopaedic surgery in Ireland: a pilot study on patient and nursing staff satisfaction. J Robot Surg. 2010;4(3):177–82. https://doi.org/10.1007/s11701-010-0207-x.
Friedman N, Cabral A. Using a telepresence robot to improve self-efficacy of people with developmental disabilities. In: ACM conference on computers and accessibility. 2018. p. 489–491.
Shi G, Shah P, Canares T, Zimmer-Galler I. Improving the pediatric hospital experience using telepresence robotics. JMIR. 2019;5(1): e15259. https://doi.org/10.2196/15259.
Zhang G, Hansen JP. People with motor disabilities using gaze to control telerobots. In: International conference in human-computer interaction. 2020. p. 1–9.
La Rose D, Taylor RH, Funda J, Eldridge B, Gomory S, Talamini M, et al. A telerobotic assistant for laparoscopic surgery. IEEE Eng Med Biol Mag. 1995. https://doi.org/10.1109/51.391776.
Charles S, Das H, Ohm T, Boswell C, Rodriguez G, Steele R, et al. Dexterity-enhanced telerobotic microsurgery. In: International conference on advanced robotics. 1997. p. 5–10.
Butner SE, Ghodoussi M. Transforming a surgical robot for human telesurgery. IEEE Trans Robot Autom. 2003;19(5):818–24. https://doi.org/10.1109/TRA.2003.817214.
Intuitive Surgical. Da Vinci Surgical systems: integrated technologies for robotic-assisted surgery. https://www.intuitive.com/en-us/products-and-services/da-vinci/systems.
Riga CV, Bicknell CD, Rolls A, Cheshire NJ, Hamady MS. Robot-assisted fenestrated endovascular aneurysm repair (FEVAR) using the Magellan system. J Vasc Interv Radiol. 2013;24(2):191–6. https://doi.org/10.1016/j.jvir.2012.10.006.
Auris Health. Monarch: Endoscopy transformed. https://www.aurishealth.com/monarch-platform.
Voros S, Haber GP, Menudet JF, Long JA, Cinquin P. ViKY robotic scope holder: initial clinical experience and preliminary results using instrument tracking. IEEE/ASME Trans Mechatron. 2010;15(6):879–86. https://doi.org/10.1109/TMECH.2010.2080683.
Zhang Q, Han XG, Xu YF, Fan MX, Zhao JW, Liu YJ, et al. Robotic navigation during spine surgery. Expert Rev Med Devices. 2020;17(1):27–32. https://doi.org/10.1080/17434440.2020.1699405.
Lefranc M, Peltier J. Evaluation of the ROSA™ Spine robot for minimally invasive surgical procedures. Expert Rev Med Devices. 2016;13(10):899–906. https://doi.org/10.1080/17434440.2016.1236680.
Miller R. Medtronic launches hugo to rival Intuitive’s Robotic Surgery System. Informa Pharma Intell. 2019;164:21–3.
Li QH, Zamorano L, Pandya A, Perez R, Gong J, Diaz F. The application accuracy of the NeuroMate robot–a quantitative comparison with frameless and frame-based surgical localization systems. Comput Aided Surg. 2002;7(2):90–8. https://doi.org/10.3109/10929080209146020.
Herry Y, Batailler C, Lording T, Servien E, Neyret P, Lustig S. Improved joint-line restitution in unicompartmental knee arthroplasty using a robotic-assisted surgical technique. Int Orthopaed. 2017;41(11):2265–71. https://doi.org/10.1007/s00264-017-3633-9.
Feng Y, Guo Z, Dong Z, Zhou XY, Kwok KW, Ernst S, et al. An efficient cardiac mapping strategy for radiofrequency catheter ablation with active learning. Int J Comput Assist Radiol Surg. 2017;12(7):1199–207. https://doi.org/10.1007/s11548-017-1587-4.
Jakopec M, Rodriguez y Baena F, Harris SJ, Gomes P, Cobb J, Davies BL. The hands-on orthopaedic robot "Acrobot": early clinical trials of total knee replacement surgery. IEEE Trans Robot Autom. 2003;19(5):902–911. https://doi.org/10.1109/TRA.2003.817510.
Stryker. Mako: Robotic-Arm Assisted Surgery. https://www.stryker.com/us/en/portfolios/orthopaedics/joint-replacement/mako-robotic-arm-assisted-surgery.html.
Lang JE, Mannava S, Floyd AJ, Goddard MS, Smith BP, Mofidi A, et al. Robotic systems in orthopaedic surgery. J Bone Jt Surg Ser B. 2011;93(10):1296–9. https://doi.org/10.1302/0301-620X.93B10.27418.
Varghese A, Doglioli M, Fader AN. Updates and controversies of robotic-assisted surgery in gynecologic surgery. Clin Obstet Gynecol. 2019;176(3):139–48. https://doi.org/10.1097/GRF.0000000000000489.Updates.
Alemzadeh H, Raman J, Leveson N, Kalbarczyk Z, Iyer RK. Adverse events in robotic surgery: a retrospective study of 14 years of data. PLoS One. 2016;11(4): e0151470. https://doi.org/10.1371/journal.pone.0151470.
Choi H, Kwak HS, Lim YA, Kim HJ. Surgical robot for single-incision laparoscopic surgery. IEEE Trans Biomed Eng. 2014;61(9):2458–66. https://doi.org/10.1109/TBME.2014.2320941.
Wang X, Meng MQH. Robotics for natural orifice transluminal endoscopic surgery: a review. J Robot. 2012;2012:1–9. https://doi.org/10.1155/2012/512616.
Valdastri P, Simi M, Webster RJ. Advanced technologies for gastrointestinal endoscopy. Annu Rev Biomed Eng. 2012. https://doi.org/10.1146/annurev-bioeng-071811-150006.
Banerjee H, Shen S, Ren H. Magnetically actuated minimally invasive microbots for biomedical applications. In: Sun HR, J, editors. Electromagnetic actuation and sensing in medical robotics. BioEngineering. Singapore: Springer Nature; 2018. p. 11–41.
Zhao Q, Li M, Wang Z, Li J, Luo J. A quorum sensing algorithm to control nanorobot population and drug concentration in cancer area. In: IEEE international conference on robotics and biomimetics. 2015. p. 42–47.
Ahmad U, Faiyazuddin M. Smart nanobots: the future in nanomedicine and biotherapeutics. J Nanomed Biother Discov. 2016;6(1):2. https://doi.org/10.4172/2155-983x.1000e140.
Baudrit JRV, Gutierrez B, Bermudez CV, Urena YRC, Chacon SV. Nanobots: development and future. Int J Biosens Bioelectron. 2017;2(5):00037. https://doi.org/10.15406/ijbsbe.2017.02.00037
Taylor RH, Menciassi A, Fichtinger G, Fiorini P, Dario P. Medical robotics and computer integrated surgery. In: Siciliano B, Khatib O, editors. Springer handbook of robotics. Berlin: Springer International Publishing; 2016. p. 1657–83.
Iyer S, Looi T, Drake J. A single arm, single camera system for automated suturing. In: IEEE international conference on robotics and automation. 2013. p. 239–244.
Beasley RA. Medical robots: current systems and research directions. J Robot. 2012;2012:1–14. https://doi.org/10.1155/2012/401613.
Kasahara Y, Kawana H, Usuda S, Ohnishi K. Telerobotic-assisted bone-drilling system using bilateral control with feed operation scaling and cutting force scaling. Int J Med Robot Comput Assist Surg. 2012;8(2):221–9. https://doi.org/10.1002/rcs.457.
Hu Y, Li D, Zong G, Sun X. Robotic system for microsurgical keratoplasty. In: Annual international conference of the ieee engineering in medicine and biology. 2005. p. 43.
Rafii-Tari H, Payne CJ, Yang GZ. Current and emerging robot-assisted endovascular catheterization technologies: a review. Ann Biomed Eng. 2014;42(4):697–715. https://doi.org/10.1007/s10439-013-0946-8.
Li SQ, Guo WL, Liu H, Wang T, Zhou YY, Yu T, et al. Clinical application of an intelligent oropharyngeal swab robot: implication for the COVID-19 pandemic. Eur Respir J. 2020. https://doi.org/10.1183/13993003.01912-2020.
Lifeline Robotics. World’s First Automatic Swab Robot. https://www.lifelinerobotics.com/.
Vitiello V, Lee SL, Cundy TP, Yang GZ. Emerging robotic platforms for minimally invasive surgery. IEEE Rev Biomed Eng. 2013;6:111–26. https://doi.org/10.1109/RBME.2012.2236311.
Carros F, Meurer J, Löffler D, Unbehaun D, Matthies S, Koch I, et al. Exploring human-robot interaction with the elderly: results from a ten-week case study in a care home. In: Conference on human factors in computing systems. 2020. p. 12.
Funding
Open access funding provided by CSIRO Library Services. This work was supported by Queensland Health.
Author information
Authors and Affiliations
Contributions
Not applicable, single author.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial or non-financial conflict of interests to disclose.
Consent to participate
Not applicable.
Ethics approval
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Silvera-Tawil, D. Robotics in Healthcare: A Survey. SN COMPUT. SCI. 5, 189 (2024). https://doi.org/10.1007/s42979-023-02551-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s42979-023-02551-0