Abstract
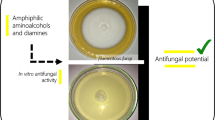
Fungal infections have emerged worldwide, and azole antifungals are widely used to control these infections. However, the emergence of antifungal resistance has been compromising the effectiveness of these drugs. Therefore, the objective of this study was to evaluate the antifungal and cytotoxic activities of the nine new 1,2,3 triazole compounds derived from thymol that were synthesized through Click chemistry. The binding mode prediction was carried out by docking studies using the crystallographic structure of Lanosterol 14α-demethylase G73E mutant from Saccharomyces cerevisiae. The new compounds showed potent antifungal activity against Trichophyton rubrum but did not show relevant action against Aspergillus fumigatus and Candida albicans. For T. rubrum, molecules nº 5 and 8 showed promising results, emphasizing nº 8, whose fungicidal and fungistatic effects were similar to fluconazole. In addition, molecule nº 8 showed low toxicity for keratinocytes and fibroblasts, concluding that this compound demonstrates promising characteristics for developing a new drug for dermatophytosis caused by T. rubrum, or serves as a structural basis for further research.






Similar content being viewed by others
References
Miceli MH, Díaz JA, Lee SA (2011) Emerging opportunistic yeast infections. Lancet Infect Dis 11:142–151. https://doi.org/10.1016/S1473-3099(10)70218-8
Wu S, Wang Y, Liu N, Dong G, Sheng C (2017) Tackling fungal resistance by biofilm inhibitors. J Med Chem 60:2193–2211. https://doi.org/10.1021/acs.jmedchem.6b01203
Carmona EM, Limper AH (2017) Overview of treatment approaches for fungal infections. Clin Chest Med 38:393–402. https://doi.org/10.1016/j.ccm.2017.04.003
Groll AH, Lumb J (2012) New developments in invasive fungal disease. Future Microbiol 7:179–184. https://doi.org/10.2217/fmb.11.154
Almeida F, Rodrigues ML, Coelho C (2019) The still underestimated problem of fungal diseases worldwide. Front Microbiol 10:1–5. https://doi.org/10.3389/fmicb.2019.00214
Munzen ME, Goncalves Garcia AD, Martinez LR (2023) An update on the global treatment of invasive fungal infections. Future Microbiol 18:1095–1117. https://doi.org/10.2217/fmb-2022-0269
Peixoto I, Maquine G, Francesconi VA, Francesconi F (2010) Dermatophytosis caused by Tricophyton rubrum as an opportunistic infection in patients with Cushing disease. An Bras Dermatol 85:888–890
Huang C, Peng Y, Zhang Y, Li R, Wan Z, Wang X (2019) Deep dermatophytosis caused by Trichophyton rubrum. Lancet Infect Dis 19:1380. https://doi.org/10.1016/S1473-3099(19)30551-1
Burmester A, Hipler UC, Uhrlaß S, Nenoff P, Singal A, Verma SB, Elsner P, Wiegand C (2020) Indian Trichophyton mentagrophytes squalene epoxidase erg1 double mutants show high proportion of combined fluconazole and terbinafine resistance. Mycoses 63:1175–1180. https://doi.org/10.1111/myc.13150
Bouchara JP, Mignon B, Chaturvedi V (2017) Dermatophytes and dermatophytoses: a thematic overview of state of the art, and the directions for future research and developments. Mycopathologia 182:1–4. https://doi.org/10.1007/s11046-017-0114-z
Arikan S, Rex J H (2001) Nystatin LF (Aronex/Abbott). Current opinion in investigational drugs (London, England: 2000) 2:488–495
Allen D, Wilson D, Drew R, Perfect J (2015) Azole antifungals: 35 years of invasive fungal infection management. Expert Rev Anti Infect Ther 13:787–798. https://doi.org/10.1586/14787210.2015.1032939
Denning DW (2003) Echinocandin antifungal drugs. Lancet 362:1142–1151. https://doi.org/10.1016/S0140-6736(03)14472-8
Moudgal V, Sobel J (2010) Antifungals to treat Candida albicans. Expert Opin Pharmacother 11:2037–2048. https://doi.org/10.1517/14656566.2010.493875
Bhatia A, Kanish B, Badyal D, Kate P (2019) Efficacy of oral terbinafine versus itraconazole in treatment of dermatophytic infection of skin—A prospective, randomized comparative study. Indian J Pharmacol 51:116–119. https://doi.org/10.1016/B978-0-323-60984-5.00062-7
Roemer T, Krysan DJ (2014) Antifungal drug development: challenges, unmet clinical needs, and new approaches. Cold Spring Harb Perspect Med. https://doi.org/10.1101/cshperspect.a019703
Monk BC, Sagatova AA, Hosseini P, Ruma YN, Wilson RK, Keniya MV (2019) Fungal Lanosterol 14α-demethylase: A target for next-generation antifungal design. Biochim Biophys Acta Proteins Proteom. https://doi.org/10.1016/j.bbapap.2019.02.008
Yin W, Zhang Y, Cui H, Jiang H, Liu L, Zheng Y, Wu T, Zhao L, Sun Y, Su X, Li S, Zhao D, Cheng M (2021) Design, synthesis and evaluation of novel 5-phenylthiophene derivatives as potent fungicidal of Candida albicans and antifungal reagents of fluconazole-resistant fungi. Eur J Med Chem 225:113740. https://doi.org/10.1016/j.ejmech.2021.113740
Zhao L, Sun Y, Yin W, Tian L, Sun N, Zheng Y, Zhang C, Zhao S, Su X, Zhao D, Cheng M (2022) Design, synthesis, and biological activity evaluation of 2-(benzo[b]thiophen-2-yl)-4-phenyl-4,5-dihydrooxazole derivatives as broad-spectrum antifungal agents. Eur J Med Chem 228:113987. https://doi.org/10.1016/j.ejmech.2021.113987
Thamban Chandrika N, Shrestha SK, Ngo HX, Tsodikov OV, Howard KC, Garneau-Tsodikova S (2018) Alkylated piperazines and piperazine-azole hybrids as antifungal agents. J Med Chem 61:158–173. https://doi.org/10.1021/acs.jmedchem.7b01138
Liu N, Tu J, Dong G, Wang Y, Sheng C (2018) Emerging new targets for the treatment of resistant fungal infections. J Med Chem 61:5484–5511. https://doi.org/10.1021/acs.jmedchem.7b01413
Corrêa JCR, Salgado HRN (2011) Review of fluconazole properties and analytical methods for its determination. Crit Rev Anal Chem 41:124–132. https://doi.org/10.1080/10408347.2011.557980
Fisher MC, Hawkins NJ, Sanglard D, Gurr SJ (2018) Worldwide emergence of resistance to antifungal drugs challenges human health and food security. Science 360:739–742. https://doi.org/10.1126/science.aap7999
Agnello S, Brand M, Chellat MF, Gazzola S, Riedl R (2019) A structural view on medicinal chemistry strategies against drug resistance. Angew Chem Int Ed Engl 58:3300–3345. https://doi.org/10.1002/anie.201802416
Han G, Liu N, Li C, Tu J, Li Z, Sheng C (2020) Discovery of novel fungal lanosterol 14α-demethylase (CYP51)/histone deacetylase dual inhibitors to treat azole-resistant candidiasis. J Med Chem 63:5341–5359. https://doi.org/10.1021/acs.jmedchem.0c00102
Da X, Nishiyama Y, Tie D, Hein KZ, Yamamoto O, Morita E (2019) Antifungal activity and mechanism of action of Ou-gon (Scutellaria root extract) components against pathogenic fungi. Sci Rep 9:1683. https://doi.org/10.1038/s41598-019-38916-w
Arif T, Bhosale JD, Kumar N, Mandal TK, Bendre RS, Lavekar GS, Dabur R (2009) Natural products–antifungal agents derived from plants. J Asian Nat Prod Res 11:621–638. https://doi.org/10.1080/10286020902942350
Guo N, Liu J, Wu X, Bi X, Meng R, Wang X, Xiang H, Deng X, Yu L (2009) Antifungal activity of thymol against clinical isolates of fluconazole-sensitive and -resistant Candida albicans. J Med Microbiol 58:1074–1079. https://doi.org/10.1099/jmm.0.008052-0
Zhao J, Li Y, Liu Q, Gao K (2010) Antimicrobial activities of some thymol derivatives from the roots of Inula hupehensis. Food Chem 120:512–516. https://doi.org/10.1016/j.foodchem.2009.10.045
Tyndall JDA, Sabherwal M, Sagatova AA, Keniya MV, Negroni J, Wilson RK, Woods MA, Tietjen K, Monk BC (2016) Structural and functional elucidation of yeast lanosterol 14α-demethylase in complex with agrochemical antifungals. PLoS One 11:e0167485. https://doi.org/10.1371/journal.pone.0167485
Alves Eloy M, Ribeiro R, Martins Meireles L, Antonio De Sousa Cutrim T, Santana Francisco C, LirianJavarini C, Borges WDS, Costa AV, De Queiroz VT, Scherer R, Lacerda V, Alves BezerraMorais P (2021) Thymol as an interesting building block for promising fungicides against fusarium solani. J Agric Food Chem 69:6958–6967. https://doi.org/10.1021/acs.jafc.0c07439
Clinical and Laboratory Standards Institute (2008) Reference method for broth dilution antifungal susceptibility testing of yeast; approved standard—3rd ed. CLSI document M27–3A. Clinical and Laboratory Standards Institute, Wayne, PA.
Clinical and Laboratory Standards Institute (2008) Reference method for broth dilution antifungal susceptibility testing of filamentous fungi; approved standard, 2nd ed CLSI M38-A2 Clinical and Laboratory Standards Institute, Wayne, PA.
Espinel-Ingroff A, Fothergil A, Peter J, Rinaldi M, Walsh T (2002) Testing conditions for determination of minimum fungicidal concentrations of new and established antifungal agents for, society. 40:3204–3208. https://doi.org/10.1128/JCM.40.9.3204
Van Dijck P, Sjollema J, Camue BPA, Lagrou K, Berman J, D’Enfert C, Andes DR, Arendrup MC, Brakhage AA, Calderone R, Cantón E, Coenye T, Cos P, Cowen LE, Edgerton M, Espinel-Ingroff A, Filler SG, Ghannoum M, Gow NAR, Haas H, Jabra-Rizk MA, Johnson EM, Lockhart SR, Lopez-Ribot JL, Maertens J, Munro CA, Nett JE, Nobile CJ, Pfaller MA, Ramage G, Sanglard D, Sanguinetti M, Spriet I, Verweij PE, Warris A, Wauters J, Yeaman MR, Zaat SAJ, Thevissen K (2018) Methodologies for in vitro and in vivo evaluation of efficacy of antifungal and antibiofilm agents and surface coatings against fungal biofilms. Microbial Cell 5:300–326. https://doi.org/10.15698/mic2018.07.638
Klepser ME, Ernst EJ, Lewis RE, Ernst ME, Pfaller MA (1998) Influence of test conditions on antifungal time-kill curve results: Proposal for standardized methods. Antimicrob Agents Chemother 42:1207–1212
Ghannoum M, Isham N, Verma A, Plaum S, Fleischer A, Hardas B (2013) In vitro antifungal activity of naftifine hydrochloride against dermatophytes. Antimicrob Agents Chemother 57:4369–4372. https://doi.org/10.1128/AAC.01084-13
Mosmann T (1983) Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Methods 16:55–63
Kumar S, Sharma B, Mehra V, Kumar V (2021) Recent accomplishments on the synthetic/biological facets of pharmacologically active 1H–1,2,3-triazoles. Eur J Med Chem 212:1–32. https://doi.org/10.1016/j.ejmech.2020.113069
Teng X, Wang Y, Gu J, Shi P, Shen Z, Ye L (2018) Antifungal agents: Design, synthesis, antifungal activity and molecular docking of phloroglucinol derivatives. Molecules 23. https://doi.org/10.3390/molecules23123116
Resende DISP, Pereira-Terra P, Inácio ÂS, Da Costa PM, Pinto E, Sousa E, Pinto MMM (2018) Lichen xanthones as models for new antifungal agents. Molecules 23. https://doi.org/10.3390/molecules23102617
Magagnin CM, Stopiglia CD, Vieira FJ, Heidrich D, Machado M, Vetoratto G, Lamb FM, Scroferneker ML (2011) Antifungal susceptibility of dermatophytes isolated from patients with chronic renal failure. An Bras Dermatol 86(4):694–701. https://doi.org/10.1590/s0365-05962011000400011
Ni T, Pang L, Cai Z, Xie F, Ding Z, Hao Y, Li R, Yu S, Chai X, Wang T, Jin Y, Zhang D, Jiang Y (2018) Design, synthesis, and in vitro antifungal evaluation of novel triazole derivatives bearing alkynyl side chains. J Saudi Chem Soc. https://doi.org/10.1016/j.jscs.2018.10.003
Allahdadi M, Hajihossein R, Kord M, Rahmati E, Amanloo S, Didehdar M (2019) Molecular characterization and antifungal susceptibility profile of dermatophytes isolated from scalp dermatophyte carriage in primary school children in Arak city, Center of Iran. J Mycol Med. https://doi.org/10.1016/j.mycmed.2019.01.002
Wiederhold NP (2022) Pharmacodynamics, mechanisms of action and resistance, and spectrum of activity of new antifungal agents. J Fungi 8. https://doi.org/10.3390/jof8080857
Harrison JR, Brand S, Smith V, Robinson DA, Thompson S, Smith A, Davies K, Mok N, Torrie LS, Collie I, Hallyburton I, Norval S, Simeons FRC, Stojanovski L, Frearson JA, Brenk R, Wyatt PG, Gilbert IH, Read KD (2018) A molecular hybridization approach for the design of potent, highly selective, and brain-penetrant N-Myristoyltransferase inhibitors. J Med Chem 61:8374–8389. https://doi.org/10.1021/acs.jmedchem.8b00884
Iman M, Peroomian T, Davood A, Amini M, Sardari S, Azerang P (2016) Design, synthesis and evaluation of new azoles as antifungal agents: a molecular hybridization approach. Pharm Chem J 49:687–693. https://doi.org/10.1007/s11094-016-1354-9
Nepali K, Lee H-Y, Liou J-P (2019) Nitro-group-containing drugs. J Med Chem 62:2851–2893. https://doi.org/10.1021/acs.jmedchem.8b00147
Benedetto Tiz D, Bagnoli L, Rosati O, Marini F, Sancineto L, Santi C (2022) New halogen-containing drugs approved by FDA in 2021: an overview on their syntheses and pharmaceutical use. Molecules 27:1643. https://doi.org/10.3390/molecules27051643
Curran MP, McCormack PL (2008) Methoxy polyethylene glycol-epoetin beta: a review of its use in the management of anaemia associated with chronic kidney disease. Drugs 68:1139–1156. https://doi.org/10.2165/00003495-200868080-00009
Nivoix Y, Ledoux MP, Herbrecht R (2020) Antifungal therapy: new and evolving therapies. Semin Respir Crit Care Med 41:158–174. https://doi.org/10.1055/s-0039-3400291
Öz Y, Özdemir HG, Gökbolat E, Kiraz N, Ilkit M, Seyedmousavi S (2016) Time-kill kinetics and in vitro antifungal susceptibility of non-fumigatus aspergillus species isolated from patients with ocular mycoses. Mycopathologia 181:225–233. https://doi.org/10.1007/s11046-015-9969-z
Kowalczyk A, Fecka I, Przychodna M, Sopata S, Bodalska A (2020) Thymol and thyme essential oil—new insights into selected therapeutic applications. Molecules 25:4125–4142
Jafri H, Ahmad I (2020) Thymus vulgaris essential oil and thymol inhibit biofilms and interact synergistically with antifungal drugs against drug resistant strains of Candida albicans and Candida tropicalis. J Mycol Med 30:100911. https://doi.org/10.1016/j.mycmed.2019.100911
Khan MSA, Malik A, Ahmad I (2012) Anti-candidal activity of essential oils alone and in combination with amphotericin B or fluconazole against multi-drug resistant isolates of Candida albicans. Med Mycol 50:33–42. https://doi.org/10.3109/13693786.2011.582890
Adan A, Kiraz Y, Baran Y (2016) Cell proliferation and cytotoxicity assays. Curr Pharm Biotechnol 17:1213. https://doi.org/10.2174/1389201017666160808160513
Gupta AK, Lyons DCA (2015) The rise and fall of oral ketoconazole. J Cutan Med Surg 19:352–357. https://doi.org/10.1177/1203475415574970
Funding
This work was supported by the Foundation for Support to Research and Innovation of Espírito Santo-FAPES. In addition, this study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brazil (CAPES)—Finance Code 001.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Responsible Editor: Luis Augusto Nero
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
de Sousa Cutrim, T.A., Eloy, M.A., Barcelos, F.F. et al. New thymol-derived triazole exhibits promising activity against Trichophyton rubrum. Braz J Microbiol (2024). https://doi.org/10.1007/s42770-024-01295-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s42770-024-01295-0