Abstract
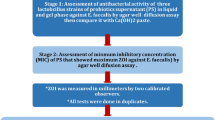
The aim of the present study was to evaluate, in vitro, the antimicrobial activity of the probiotic Bifidobacterium animalis subsp. lactis HN019, through the well technique, against 10 microorganisms can be found involved in endodontic infections. The antimicrobial activity of the probiotic was performed on Streptococcus mutans, Streptococcus sobrinus, Lacticaseibacillus casei, Enterococcus faecalis, Staphylococcus aureus, Candida albicans, Porphyromonas gingivalis, Porphyromonas endodontalis, Fusobacterium nucleatum and Prevotella intermedia. For the control group, it was used non-pathogenic bacteria Escherichia coli, Saccharomyces cerevisiae, and Kocuria rizhopilla. After 48 to 72 h of incubation of the petri dishes containing the culture medium, the microorganism strains, and the probiotic, the plates were examined to assess the uniformity of microbial growth, presence of contaminants, and the halo of inhibition. After visual inspection, the reading of the halo of inhibition was performed with the aid of a digital caliper using a reflected light source to illuminate the inverted plate on a black, opaque background after removing the cap. Thus, 3 values were obtained from each bacterial inoculum, which were added and divided by three to obtain the average of the values. The results of the in vitro study demonstrated that the probiotic B. animalis subsp. lactis HN019 promoted the inhibition of all strains of the pathogens evaluated, with the exception of Candida albicans, demonstrating antimicrobial activity on these microorganisms.



Similar content being viewed by others
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Food and Agriculture Organization and World Health Organization Expert Consultation (2001) Evaluation of health and nutritional properties of powder milk and live lactic acid bacteria. Córdoba, Argentina: Food and Agriculture Organization of the United Nations and World Health Organization; [cited 2005 September 8]. Available from: ftp://ftp.fao.org/es/esn/food/probio_report_en.pdf
Mahasneh SA, Mahasneh AD (2017) Probiotics: a promising role in dental health. Dent J 5(4):26. https://doi.org/10.3390/dj5040026
Keller MK, Hasslöf P, Dahlén G, Stecksén-Blicks G, Twetman S (2012) Probiotic supplements (lactobacillus reuteri dsm 17938 and atcc pta 5289) do not affect regrowth of mutans streptococci after full-mouth disinfection with chlorhexidine: a randomized controlled multicenter trial. Caries Res 46:140–146. https://doi.org/10.1159/000337098
McCabe LR, Parameswaran N (2018) Advances in probiotic regulation of bone and mineral metabolism. Calcif Tissue Int 102:480–488. https://doi.org/10.1007/s00223-018-0403-7
Aggarwal N, Breedon AME, Davis CM, Hwang IY, Chang MW (2020) Engineering probiotics for therapeutic applications: recent examples and translational outlook. Curr Opin Biotechnol 65:171–179. https://doi.org/10.1016/j.copbio.2020.02.016
Singh D, Khan MA, Siddique HR (2021) Therapeutic implications of probiotics in microbiota dysbiosis: a special reference to the liver and oral cancers. Life Sci 285:120008. https://doi.org/10.1016/j.lfs.2021.120008
Twetman L, Larsen U, Fiehn NE, Stecksén-Blicks C, Twetman S (2009) Coaggregation between probiotic bacteria and caries-associated strains: an in vitro study. Acta Odontol Scand 67:284–288. https://doi.org/10.1080/00016350902984237
Islam SU (2016) Clinical uses of probiotics. Medicine (Baltimore) 95(5):e2658. https://doi.org/10.1097/MD.0000000000002658
Meurman JH, Stamatova IV (2018) Probiotics: evidence of oral health implications. Folia Med (Plovdiv) 60:21–29. https://doi.org/10.1515/folmed-2017-0080
Butler MI, Mörkl S, Sandhu KV, Cryan JF, Dinan TG (2019) The gut microbiome and mental health: what should we tell our patients?: Le microbiote Intestinal et la Santé Mentale : que Devrions-Nous dire à nos Patients? Can J Psychiatry 64(11):747–760. https://doi.org/10.1177/0706743719874168
Seminario-Amez M, López-López J, Estrugo-Devesa A, Ayuso-Montero R, Jané-Salas E (2017) Probiotics and oral health: a systematic review. Med Oral Patol Oral Cir Bucal 22(3):e282–e288. https://doi.org/10.4317/medoral.21494
Radaic A, Ye C, Parks B, Gao L, Kuraji R, Malone E, Kamarajan P, Zhan L, Kapila YL (2020) Modulation of pathogenic oral biofilms towards health with nisin probiotic. J Oral Microbiol 12(1):1809302. https://doi.org/10.1080/20002297.2020.1809302
Hirasawa M, Kurita-Ochia T (2020) Probiotic potential of Lactobacilli isolated from saliva of periodontally healthy individuals. Oral Health Prev Dent 18(1):563–570. https://doi.org/10.3290/j.ohpd.a44693
Vestman N, Chen T, Lif Holgerson P, Öhman C, Johansson I (2015) Oral microbiota shift after 12-week supplementation with Lactobacillus reuteri DSM 17938 and PTA 5289: a randomized control trial. PLoS One 6(10):e0125812. https://doi.org/10.1371/journal.pone.0125812
Bustamante M, Oomah BD, Mosi-Roa Y, Rubilar M, Burgos-Díaz C (2020) Probiotics as an adjunct therapy for the treatment of halitosis, dental caries and periodontitis. Probiotics Antimicrob Proteins 12(2):325–334. https://doi.org/10.1007/s12602-019-9521-4
Kraft-Bodi E, Jørgensen MR, Keller MK, Kragelund C, Twetman S (2015) Effect of probiotic bacteria on oral Candida in frail elderly. J Dent Res 94(9 Suppl):181S–186S. https://doi.org/10.1177/0022034515595950
Matsubara VH, Bandara HM, Mayer MP, Samaranayake LP (2016) Probiotics as antifungals in mucosal candidiasis. Clin Infect Dis 62(9):1143–1153. https://doi.org/10.1093/cid/ciw038
York A (2019) A probiotic for candidiasis? Nat Rev Microbiol 17(12):723. https://doi.org/10.1038/s41579-019-0296-0
Keller MK, Hasslöf P, Stecksén-Blicks C, Twetman S (2011) Co-aggregation and growth inhibition of probiotic lactobacilli and clinical isolates of mutans streptococci: an in vitro study. Acta Odontol Scand 69:263–268. https://doi.org/10.3109/00016357.2011.554863
Jiang Q, Stamatova I, Kainulainen V, Korpela R, Meurman JH (2016) Interactions between Lactobacillus rhamnosus GG and oral micro-organisms in an in vitro biofilm model. BMC Microbiol 12(16):149. https://doi.org/10.1186/s12866-016-0759-7
Lin TH, Lin CH, Pan TM (2018) The implication of probiotics in the prevention of dental caries. Appl Microbiol Biotechnol 102(2):577–586. https://doi.org/10.1007/s00253-017-8664-z
Zaura E, Twetman S (2019) Critical appraisal of oral pre- and probiotics for caries prevention and care. Caries Res 53(5):514–526. https://doi.org/10.1159/000499037
Ricoldi MST, Furlaneto FAC, Oliveira LFF, Teixeira GC, Pischiotini JP, Moreira ALG, Ervolino E, de Oliveira MN, Bogsan CSB, Salvador SL, Messora MR (2017) Effects of the probiotic Bifidobacterium animalis subsp. lactis on the non-surgical treatment of periodontitis. A histomorphometric, microtomographic and immunohistochemical study in rats. PLoS One 12(6). https://doi.org/10.1371/journal.pone.0179946
Morales A, Gandolfo A, Bravo J, Carvajal P, Silva N, Godoy C, Garcia-Sesnich J, Hoare A, Diaz P, Gamonal J (2018) Microbiological and clinical effects of probiotics and antibiotics on nonsurgical treatment of chronic periodontitis: a randomized placebo- controlled trial with 9-month follow-up. J Appl Oral Sci 26:e20170075. https://doi.org/10.1590/1678-7757-2017-0075
Schmitter T, Fiebich BL, Fischer JT, Gajfulin M, Larsson N, Rose T, Goetz MR (2018) Ex vivo anti- inflammatory effects of probiotics for periodontal health. J Oral Microbiol 25(10):1502027. https://doi.org/10.1080/20002297.2018.1502027
Messora MR, Oliveira LF, Foureaux RC, Taba M Jr, Zangerônimo MG, Furlaneto FA, Pereira LJ (2013) Probiotic therapy reduces periodontal tissue destruction and improves the intestinal morphology in rats with ligature-induced periodontitis. J Periodontol 84(12):1818–1826. https://doi.org/10.1902/jop.2013.120644
Grusovin MG, Bossini S, Calza S, Cappa V, Garzetti G, Scotti E, Gherlone EF, Mensi M (2020) Clinical efficacy of Lactobacillus reuteri-containing lozenges in the supportive therapy of generalized periodontitis stage III and IV, grade C: 1-year results of a double-blind randomized placebo-controlled pilot study. Clin Oral Investig 24(6):2015–2024. https://doi.org/10.1007/s00784-019-03065-x
Messora MR, Pereira LJ, Foureaux R, Oliveira LF, Sordi CG, Alves AJ, Napimoga MH, Nagata MJ, Ervolino E, Furlaneto FA (2016) Favourable effects of Bacillus subtilis and Bacillus licheniformis on experimental periodontitis in rats. Arch Oral Biol 66:108–119. https://doi.org/10.1016/j.archoralbio.2016.02.014
Oliveira LF, Salvador SL, Silva PHF, Furlaneto FAC, Figueiredo L, Casarin R, Ervolino E, Palioto DB, Souza SLS, Taba MJ, Novaes ABNJ, Messora MR (2017) Benefits of Bifidobacterium animalis subsp. lactis Probiotic in Experimental Periodontitis. J Periodontol 88:197–208. https://doi.org/10.1902/jop.2016.160217
Luo W, Li H, Ye F (2021) Clinical therapeutic effects of probiotics in combination with antibiotics on periodontitis: a protocol for systematic review and meta-analysis. Medicine (Baltimore) 100(4):e23755. https://doi.org/10.1097/MD.0000000000023755
Gomez A, Nelson KE (2017) The oral microbiome of children: development, disease, and implications beyond oral health. Microb Ecol 73(2):492–503. https://doi.org/10.1007/s00248-016-0854-1
Sharma N, Bhatia S, Sodhi AS, Batra N (2018) Oral microbiome and health. AIMS Microbiol 4(1):42–66. https://doi.org/10.3934/microbiol.2018.1.42
Belibasakis GN, Bostanci N, Marsh PD, Zaura E (2019) Applications of the oral microbiome in personalized dentistry. Arch Oral Biol 104:7–12. https://doi.org/10.1016/j.archoralbio.2019.05.023
Xiao J, Fiscella KA, Gill SR (2020) Oral microbiome: possible harbinger for children’s health. Int J Oral Sci 12(1):12. https://doi.org/10.1038/s41368-020-0082-x
Sasaki H, Okamatsu Y, Kawai T, Kent R, Taubman M, Stashenko P (2004) The interleukin-10 knockout mouse is highly susceptible to Porphyromonas gingivalis-induced alveolar bone loss. J Periodontal Res 39:432–441. https://doi.org/10.1111/j.1600-0765.2004.00760.x
Neelakantan P, Romero M, Vera J, Daood U, Khan AU, Yan A, Cheung GSP (2017) Biofilms in endodontics-current status and future directions. Int J Mol Sci 18(8):1748. https://doi.org/10.3390/ijms18081748
Iqbal A (2012) Antimicrobial irrigants in the endodontic therapy. Int J Health Sci 6:186–192
Marsh PD (2010) Microbiology of dental plaque biofilms and their role in oral health and caries. Dent Clin N Am 54:441–454. https://doi.org/10.1016/j.cden.2010.03.002
Allaker RP, Stephen AS (2017) Use of probiotics and oral health. Curr Oral Health Rep 4:309–318. https://doi.org/10.1007/s40496-017-0159-6
Samaranayake L, Matsubara VH (2017) Normal oral flora and the oral ecosystem. Dent Clin N Am 61:199–215. https://doi.org/10.1016/j.cden.2016.11.002
Brook I (2003) Microbiology and management of endodontic infections in children. J Clin Pediatr Dent 28:13–18. https://doi.org/10.17796/jcpd.28.1.uwjxq61753506255
Siqueira JF, Roças I (2014) Present status and future directions in endodontic microbiology. Endod Topics 30:3–22. https://doi.org/10.1111/iej.13677
Bohora A, Kokate S (2017) Evaluation of the role of probiotics in endodontic treatment: a preliminary study. J Int Soc Prev Community Dent 7(1):46–51. https://doi.org/10.4103/2231-0762.200710
Bohora AA, Kokate SR, Khedkar S, Vankudre A (2019) Antimicrobial activity of probiotics against endodontic pathogens: - a preliminary study. Indian J Med Microbiol 37(1):5–11. https://doi.org/10.4103/ijmm.IJMM_18_333
El-Sayed H, Aly Y, Elgamily H, Nagy MM (2019) A promising probiotic irrigant: an in vitro study. Open Access Maced J Med Sci 7(3):407–411. https://doi.org/10.3889/oamjms.2019.074
Cosme-Silva L, Dal-Fabbro R, Cintra LTA, Dos Santos VR, Duque C, Ervolino E, Mogami Bomfim S, Gomes-Filho JE (2019) Systemic administration of probiotics reduces the severity of apical periodontitis. Int Endod J 52(12):1738–1749. https://doi.org/10.1111/iej.13192
Cosme-Silva L, Dal-Fabbro R, Cintra LTA, Ervolino E, Plazza F, Mogami Bomfim S, Duarte PCT, Junior VEDS, Gomes-Filho JE (2020) Reduced bone resorption and inflammation in apical periodontitis evoked by dietary supplementation with probiotics in rats. Int Endod J 53(8):1084–1092. https://doi.org/10.1111/iej.13311
Kumar G, Tewari S, Tagg J, Chikindas ML, Popov IV, Tiwari SK (2021) Can probiotics emerge as effective therapeutic agents in apical periodontitis? A review. Probiotics Antimicrob Proteins 13(2):299–314. https://doi.org/10.1007/s12602-021-09750-2
Rakhimova O, Schmidt A, Landström M, Johansson A, Kelk P, Romani Vestman N (2021) Cytokine secretion, viability, and real-time proliferation of apical-papilla stem cells upon exposure to oral bacteria. Front Cell Infect Microbiol 10:620801. https://doi.org/10.3389/fcimb.2020.620801
Invernici MM, Furlaneto FAC, Salvador SL, Ouwehand AC, Salminen S, Mantziari A, Vinderola G, Ervolino E, Santana SI, Silva PHF, Messora MR (2020) Bifidobacterium animalis subsp. lactis HN019 presents antimicrobial potential against periodontopathogens and modulates the immunological response of oral mucosa in periodontitis patients. PLoS One 15(9):e0238425. https://doi.org/10.1371/journal.pone.0238425
Vives-Soler A, Chimenos-Küstner E (2020) Effect of probiotics as a complement to non-surgical periodontal therapy in chronic periodontitis: a systematic review. Med Oral Patol Oral Cir Bucal 25(2):e161–e167. https://doi.org/10.4317/medoral.23147
Hu L, Zhou M, Young A, Zhao W, Yan Z (2019) In vivo effectiveness and safety of probiotics on prophylaxis and treatment of oral candidiasis: a systematic review and meta-analysis. BMC Oral Health 19(1):140. https://doi.org/10.1186/s12903-019-0841-2
Cheng B, Zeng X, Liu S, Zou J, Wang Y (2020) The efficacy of probiotics in management of recurrent aphthous stomatitis: a systematic review and meta-analysis. Sci Rep 10(1):21181. https://doi.org/10.1038/s41598-020-78281-7
İnce G, Gürsoy H, İpçi ŞD, Cakar G, Emekli-Alturfan E, Yılmaz S (2015) Clinical and biochemical evaluation of lozenges containing Lactobacillus reuteri as an adjunct to non-surgical periodontal therapy in chronic periodontitis. J Periodontol 86(6):746–754. https://doi.org/10.1902/jop.2015.140612
Tekce M, Ince G, Gursoy H, Dirikan Ipci S, Cakar G, Kadir T, Yılmaz S (2015) Clinical and microbiological effects of probiotic lozenges in the treatment of chronic periodontitis: a 1-year follow-up study. J Clin Periodontol 42(4):363–372. https://doi.org/10.1111/jcpe.12387
Morales A, Carvajal P, Silva N, Hernandez M, Godoy C, Rodriguez G, Cabello R, Garcia-Sesnich J, Hoare A, Diaz PI, Gamonal J (2016) Clinical effects of Lactobacillus rhamnosus in non-surgical treatment of chronic periodontitis: a randomized placebo-controlled trial with 1-year follow-up. J Periodontol 87(8):944–952. https://doi.org/10.1902/jop.2016.150665
Gill HS, Rutherfurd KJ, Prasad J, Gopal PK (2000) Enhancement of natural and acquired immunity by Lactobacillus rhamnosus (HN001), Lactobacillus acidophilus (HN017) and Bifidobacterium lactis (HN019). Br J Nutr 83(2):167–176. https://doi.org/10.1017/s0007114500000210
Toiviainen A, Jalasvuori H, Lahti E, Gursoy U, Salminen S, Fontana M, Flannagan S, Eckert G, Kokaras A, Paster B, Söderling E (2015) Impact of orally administered lozenges with Lactobacillus rhamnosus GG and Bifidobacterium animalis subsp. lactis BB-12 on the number of salivary mutans streptococci, amount of plaque, gingival inflammation and the oral microbiome in healthy adults. Clin Oral Investig 19(1):77–83. https://doi.org/10.1007/s00784-014-1221-6
Dahlén G (2017) Culture-based analysis of endodontic infections. In: Fouad AF (ed) Endodontic microbiology, 2nd edn. Wiley, New York, pp 57–79
Hernández-Bautista LM, Márquez-Preciado R, Ortiz-Magdaleno M, Pozos-Guillén A, Aranda-Romo S, Sánchez-Vargas LO (2020) Effect of five commercial probiotic formulations on Candida albicans growth: in vitro study. J Clin Pediatr Dent 44(5):315–322. https://doi.org/10.17796/1053-4625-44.5.5
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Responsible Editor: Carla Taddei
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Araujo, L.D.C., da Silva, R.A.B., Silva, C.M.P.C. et al. Bifidobacterium animalis subsp. lactis HN019 has antimicrobial activity against endodontic pathogens in vitro. Braz J Microbiol 54, 2289–2295 (2023). https://doi.org/10.1007/s42770-023-01083-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42770-023-01083-2