Abstract
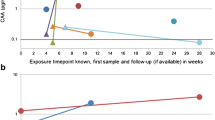
Sporotrichosis zoonotic transmission by cats has obtained hyperendemic magnitude in Rio de Janeiro, Brazil. Atypical cases, relapses, and reinfections as well as reduced diagnostic sensitivity of conventional methods have been reported. Previously, the anti-SsCBF enzyme-linked immunosorbent assay (ELISA) test was shown to be useful as a diagnostic tool for human sporotrichosis. Effective diagnosis and treatment are critical to interrupt the chain of transmission of this major pathogen in Brazilian Public Health. To evaluate its applicability for feline sporotrichosis diagnosis and/or therapeutic follow-up, 15 domestic cats from Rio de Janeiro were clinically and laboratory monitored by cytopathology, culture, Sporothrix genotyping, and anti-SsCBF IgG levels. Subsequently, animals were divided into satisfactory and non-satisfactory therapeutic responders. Averages of antibody serum levels obtained for diagnosis (first consultation) compared with the levels found after follow-up (last consultation) were significantly different in both groups (p = 0.0002 and p = 0.038, respectively). We conclude that the SsCBF ELISA test can predict feline sporotrichosis therapeutic responses even for animals with distinct clinical evolutions.



Similar content being viewed by others
References
Rodrigues AM, Teixeira M d M, de Hoog GS et al (2013) Phylogenetic analysis reveals a high prevalence of Sporothrix brasiliensis in feline sporotrichosis outbreaks. PLoS Negl Trop Dis 7:e2281. https://doi.org/10.1371/journal.pntd.0002281
Rodrigues AM, de Hoog GS, de Camargo ZP (2016) Sporothrix species causing outbreaks in animals and humans driven by animal–animal transmission. PLoS Pathog 12:e1005638. https://doi.org/10.1371/journal.ppat.1005638
Gremião IDF, Miranda LHM, Reis EG, Rodrigues AM, Pereira SA (2017) Zoonotic epidemic of sporotrichosis: cat to human transmission. PLoS Pathog 13:e1006077. https://doi.org/10.1371/journal.ppat.1006077
Castro R a, Kubitschek-Barreira PH, Teixeira P a C et al (2013) Differences in cell morphometry, cell wall topography and gp70 expression correlate with the virulence of Sporothrix brasiliensis clinical isolates. PLoS One 8:1–18. https://doi.org/10.1371/journal.pone.0075656
Fernandes GF, dos Santos PO, Rodrigues AM, Sasaki AA, Burger E, de Camargo ZP (2013) Characterization of virulence profile, protein secretion and immunogenicity of different Sporothrix schenckii sensu stricto isolates compared with S. globosa and S. brasiliensis species. Virulence 4:241–249. https://doi.org/10.4161/viru.23112
de Beer ZW, Duong TA, Wingfield MJ (2016) The divorce of Sporothrix and Ophiostoma: solution to a problematic relationship. Stud Mycol 83:165–191. https://doi.org/10.1016/j.simyco.2016.07.001
Della Terra PP, Rodrigues AM, Fernandes GF, Nishikaku AS, Burger E, de Camargo ZP (2017) Exploring virulence and immunogenicity in the emerging pathogen Sporothrix brasiliensis. PLoS Negl Trop Dis 11:1–23. https://doi.org/10.1371/journal.pntd.0005903
Orofino-Costa R, de Macedo PM, Rodrigues AM, Bernardes-Engemann AR (2017) Sporotrichosis: an update on epidemiology, etiopathogenesis, laboratory and clinical therapeutics. An Bras Dermatol 92:606–620. https://doi.org/10.1590/abd1806-4841.2017279
Arenas R, Carlos DS, Ramirez-hobak L et al (2018) Sporotrichosis : from KOH to. Mol Biol 4:1–10. https://doi.org/10.3390/jof4020062
Roberts GD, Larsh HW (1971) The serologic diagnosis of extracutaneous sporotrichosis. Am J Clin Pathol 56:597–600. https://doi.org/10.1093/ajcp/56.5.597
Welsh RD, Dolan CT (1973) Sporothrix whole yeast agglutination test: low-titer reactions of sera of subjects not known to have sporotrichosis. Am J Clin Pathol 59:82–85. https://doi.org/10.1093/ajcp/59.1.82
Bernardes-Engemann AR, Orofino Costa RC, Miguens BP, Penha CVL, Neves E, Pereira BAS, Dias CMP, Mattos M, Gutierrez MC, Schubach A, Oliveira Neto MP, Lazéra M, Lopes-Bezerra LM (2005) Development of an enzyme-linked immunosorbent assay for the serodiagnosis of several clinical forms of sporotrichosis. Med Mycol 43:487–493. https://doi.org/10.1080/13693780400019909
Fernandes GF, Lopes-Bezerra LM, Bernardes-Engemann AR, Schubach TMP, Dias MAG, Pereira SA, Camargo ZP (2011) Serodiagnosis of sporotrichosis infection in cats by enzyme-linked immunosorbent assay using a specific antigen, SsCBF, and crude exoantigens. Vet Microbiol 147:445–449. https://doi.org/10.1016/j.vetmic.2010.07.007
Almeida-Paes R, Pimenta MA, Monteiro PCF, Nosanchuk JD, Zancopé-Oliveira RM (2007) Immunoglobulins G, M, and A against Sporothrix schenckii exoantigens in patients with sporotrichosis before and during treatment with itraconazole. Clin Vaccine Immunol 14:1149–1157. https://doi.org/10.1128/CVI.00149-07
Almeida-Paes R, Pimenta MA, Pizzini CV, Monteiro PCF, Peralta J́M, Nosanchuk JD, Zancopé-Oliveira RM (2007) Use of mycelial-phase Sporothrix schenckii exoantigens in an enzyme-linked immunosorbent assay for diagnosis of sporotrichosis by antibody detection. Clin Vaccine Immunol 14:244–249. https://doi.org/10.1128/CVI.00430-06
Rodrigues AM, de Hoog GS, de Camargo ZP (2015) Molecular diagnosis of pathogenic Sporothrix species. PLoS Negl Trop Dis 9:e0004190. https://doi.org/10.1371/journal.pntd.0004190
Alvarado P, Ostos A, Franquiz N et al (2015) Diagnóstico serológico de la esporotricosis mediante el empleo del antígeno de micelio de Sporothrix schenckii sensu stricto. Investig Clin 56
Bernardes-Engemann AR, de Lima Barros M, Zeitune T et al (2015) Validation of a serodiagnostic test for sporotrichosis: a follow-up study of patients related to the Rio de Janeiro zoonotic outbreak. Med Mycol 53:28–33. https://doi.org/10.1093/mmy/myu058
Barros MBDL, Schubach TP, Coll JO, Gremião ID, Wanke B, Schubach A (2010) Esporotricose: a evolução e os desafios de uma epidemia. Rev Panam Salud Publica 27:455–460
Macêdo-Sales PA, Souto SRLS, Destefani CA, Lucena RP, Machado RLD, Pinto MR, Rodrigues AM, Lopes-Bezerra LM, Rocha EMS, Baptista ARS (2018) Domestic feline contribution in the transmission of Sporothrix in Rio de Janeiro State, Brazil: a comparison between infected and non-infected populations. BMC Vet Res 14:19. https://doi.org/10.1186/s12917-018-1340-4
Macedo PM, Lopes-Bezerra LM, Bernardes-Engemann AR, Orofino-Costa R (2015) New posology of potassium iodide for the treatment of cutaneous sporotrichosis: study of efficacy and safety in 102 patients. J Eur Acad Dermatology Venereol 29:719–724. https://doi.org/10.1111/jdv.12667
Penha CV, Bezerra LM (2000) Concanavalin A-binding cell wall antigens of Sporothrix schenckii: a serological study. Med Mycol 38:1–7
Orofino-Costa R, Bóia MN, Magalhães GAP et al (2010) Arthritis as a hypersensitivity reaction in a case of sporotrichosis transmitted by a sick cat: clinical and serological follow up of 13 months. Mycoses 53:81–83. https://doi.org/10.1111/j.1439-0507.2008.01661.x
Orofino-Costa R, Unterstell N, Carlos Gripp A, de Macedo PM, Brota A, Dias E, de Melo Teixeira M, Felipe MS, Bernardes-Engemann AR, Lopes-Bezerra LM (2013) Pulmonary cavitation and skin lesions mimicking tuberculosis in a HIV negative patient caused by Sporothrix brasiliensis. Med Mycol Case Rep 2:65–71. https://doi.org/10.1016/j.mmcr.2013.02.004
Macedo PM, Sztajnbok DCN, Camargo ZP et al (2015) Dacryocystitis due to Sporothrix brasiliensis : a case report of a successful clinical and serological outcome with low-dose potassium iodide treatment and oculoplastic surgery. Br J Dermatol 172:1116–1119. https://doi.org/10.1111/bjd.13378
Miranda LHM, Conceição-Silva F, Quintella LP, Kuraiem BP, Pereira SA, Schubach TMP (2013) Feline sporotrichosis: Histopathological profile of cutaneous lesions and their correlation with clinical presentation. Comp Immunol Microbiol Infect Dis 36:425–432. https://doi.org/10.1016/j.cimid.2013.03.005
Feldman EC, Ettinger SJ (2004) Tratado de Medicina Interna Veterinária - Doenças do Cão e do Gato, 5th edn. Guanabara Koogan, Rio de Janeiro
Reis ÉG, Schubach TMP, Pereira SA, Silva JN, Carvalho BW, Quintana MSB, Gremião IDF (2016) Association of itraconazole and potassium iodide in the treatment of feline sporotrichosis: a prospective study. Med Mycol 54:684–690. https://doi.org/10.1093/mmy/myw027
Rippon JW (1988) Sporotrichosis. In: Medical mycology: the pathogenic fungi and the pathogenic actinomycetes, 3rd ed. Philadelphia, p 797
Gremião I, Schubach T, Pereira S, Rodrigues AM, Honse CO, Barros MBL (2011) Treatment of refractory feline sporotrichosis with a combination of intralesional amphotericin B and oral itraconazole. Aust Vet J 89:346–351. https://doi.org/10.1111/j.1751-0813.2011.00804.x
Orofino-Costa R, de Macedo PM, Carvalhal A, Bernardes-Engemann AR (2013) Use of potassium iodide in dermatology: updates on an old drug. An Bras Dermatol 88:396–402. https://doi.org/10.1590/abd1806-4841.20132377
Xavier MO, Bittencourt LR, da Silva CM et al (2013) Atypical presentation of sporotrichosis: report of three cases. Rev Soc Bras Med Trop 46:116–118. https://doi.org/10.1590/0037-868215282013
Mialski R, de Oliveira JN, da Silva LH et al (2018) Chronic meningitis and hydrocephalus due to Sporothrix brasiliensis in immunocompetent adults: a challenging entity. Open Forum Infect Dis 5. https://doi.org/10.1093/ofid/ofy081
Barros MBDL, Schubach ADO, Schubach TMP et al (2008) An epidemic of sporotrichosis in Rio de Janeiro, Brazil: epidemiological aspects of a series of cases. Epidemiol Infect 136:1192–1196. https://doi.org/10.1017/S0950268807009727
Silva JN, Miranda LHM, Menezes RC, Gremião IDF, Oliveira RVC, Vieira SMM, Conceição-Silva F, Ferreiro L, Pereira SA (2018) Comparison of the sensitivity of three methods for the early diagnosis of sporotrichosis in cats. J Comp Pathol 160:72–78. https://doi.org/10.1016/j.jcpa.2018.03.002
Acknowledgments
The authors would like to thank the veterinarian collaborators and cat owners for allowing their animals to take part in this study. We also thank Dr. Anderson Messias Rodrigues from the Laboratory of Emerging Fungal Pathogens, São Paulo Federal University, for assisting our group on Sporothrix spp. genotyping. We are grateful to Dr. Norman Ratcliffe for editing and suggestions for improvements of the manuscript.
Funding
The authors would like to thank the National Council for Scientific and Technological Development (Conselho Nacional de Desenvolvimento Científico e Tecnológico—CNPq) for granting fellowships (PIBIC-CNPq-UFF) and the Rio de Janeiro Research Foundation (Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro—FAPERJ; E-26/103.198/2011 and E-26/010.001882/2014). Also, it was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brasil (CAPES)—Finance Code 001 and PROEX-MEC. ARSB and RLDM are research fellows of CNPq (PQ/CNPq).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Responsible Editor: Sandro Rogerio de Almeida.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 16 kb)
Rights and permissions
About this article
Cite this article
Baptista, V.S., Mothé, G.B., Santos, G.M.P. et al. Promising application of the SsCBF ELISA test to monitor the therapeutic response of feline sporotrichosis caused by Sporothrix brasiliensis from Brazilian epidemics. Braz J Microbiol 52, 145–153 (2021). https://doi.org/10.1007/s42770-020-00362-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42770-020-00362-6