Abstract
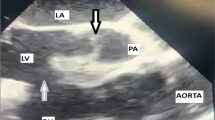
Dextro-transposition of the great arteries (D-TGA) is a congenital heart defect in which the pulmonary artery and aorta anomalously originate from the left and right ventricles, respectively. D-TGA is managed surgically in the first days of life. We describe a case of a patient with D-TGA who was managed at the age of 4 years. A Glenn shunt operation with pulmonary artery banding was performed to prepare the left ventricle for a second, definitive corrective surgery. The patient did not return for the definitive surgery. Ten years later at the age of 14, the patient started developing edema of the face and arms and was managed for bleeding esophageal varices. At the age of 19, she presented to our care with difficulty breathing and was diagnosed with superior vena cava (SVC) syndrome due to a failure of pulmonary artery banding. Glenn shunt with pulmonary artery banding was done for this patient with D-TGA at the age of 4 years, when the primary arterial switch operation was contraindicated. Pulmonary artery banding failure caused a functional obstruction of her Glenn shunt and, consequently, SVC syndrome.


Similar content being viewed by others
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Warnes CA. Transposition of the great arteries. Circ. 2006;114(24):2699–709. https://doi.org/10.1161/CIRCULATIONAHA.105.592352.
Prasad Verma R. Transposition of great arteries. In: Verma RP, editor. Congenital anomalies in newborn infants—clinical and etiopathological perspectives. IntechOpen. 2021. https://doi.org/10.5772/intechopen.99205.
Villafañe J, Lantin-Hermoso MR, Bhatt AB, Tweddell JS, Geva T, Nathan M, Elliott MJ, Vetter VL, Paridon SM, Kochilas L, Jenkins KJ, Beekman RH, Wernovsky G, Towbin JA, American College of Cardiology’s Adult Congenital and Pediatric Cardiology Council. D-transposition of the great arteries: the current era of the arterial switch operation. J Am Coll Cardiol. 2014;64(5):498–511. https://doi.org/10.1016/j.jacc.2014.06.1150.
Anderson BR, Ciarleglio AJ, Hayes DA, Quaegebeur JM, Vincent JA, Bacha EA. Earlier arterial switch operation improves outcomes and reduces costs for neonates with transposition of the great arteries. J Am Coll Cardiol. 2014;63(5):481–7. https://doi.org/10.1016/j.jacc.2013.08.1645.
Moss AJ, Allen HD, editors. Moss and Adams’ heart disease in infants, children, and adolescents: including the fetus and young adult. 7th ed. Wolters Kluwer Health/Lippincott Williams & Wilkins; 2008.
Ma K, Qi L, Hua Z, Yang K, Zhang H, Li S, Zhang S, He F, Wang G. Effectiveness of bidirectional Glenn shunt placement for palliation in complex congenitally corrected transposed great arteries. Tex Heart Inst J. 2020;47(1):15–22. https://doi.org/10.14503/THIJ-17-6555.
Nathan M. Late arterial switch operation for transposition with intact septum. World J Pediatr Congenit Heart Surg. 2014;5(2):226–8. https://doi.org/10.1177/2150135113518804.
Sharma R. The bidirectional Glenn shunt for univentricular hearts. Indian J Thorac Cardiovasc Surg. 2018;34(4):453–6. https://doi.org/10.1007/s12055-018-0653-z.
Mukherji A, Ghosh S, Das JN, Chattopadhyay A. Percutaneous salvage interventions in the Glenn circuit: a case series. Egypt Heart J. 2020;72(1):76. https://doi.org/10.1186/s43044-020-00113-w.
Klein-Weigel PF, Elitok S, Ruttloff A, Reinhold S, Nielitz J, Steindl J, Hillner B, Rehmenklau-Bremer L, Wrase C, Fuchs H, Herold T, Beyer L. Superior vena cava syndrome. Vasa. 2020;49(6):437–48. https://doi.org/10.1024/0301-1526/a000908.
Loudin M, Anderson S, Schlansky B. Bleeding ‘downhill’ esophageal varices associated with benign superior vena cava obstruction: case report and literature review. BMC Gastroenterol. 2016;16(1):134. https://doi.org/10.1186/s12876-016-0548-7.
Lasheen RA, ElTohamy A, Salaheldin EO. MIS-C frenzy: the importance of considering a broad differential diagnosis. SAGE Open Med Case Rep. 2022;10:2050313X221088397. https://doi.org/10.1177/2050313X221088397.
Salaheldin EO, Lasheen RA, ElTohamy A. The rising appendicitis mimicker: a case report of multisystem inflammatory syndrome in children (MIS-C) presenting with acute abdomen. SAGE Open Med Case Rep. 2022;10:2050313X221082903. https://doi.org/10.1177/2050313X221082903.
Author information
Authors and Affiliations
Contributions
Esraa Salaheldin took the history and physical examination, maintained clinical correspondence, and drafted the case report; Liliana Arriola-Montenegro contributed to the design and conclusion of the case report; Aya Yaseen contributed to the introduction and abstract; and Abdelrahman ElTohamy contributed to the design, discussion, and reviewing of the case report. All authors critically revised the manuscript and gave their final approval of this work.
Corresponding author
Ethics declarations
Ethics Approval
The Demerdash Hospital does not require ethics approval for reporting individual cases without patient identifying information.
Consent to Participate
Consent was obtained from both the patient and the legal guardian for participation in this report.
Consent for Publication
Written informed consent for publication of this case report and all included images was obtained from the legally authorized representative of the patient.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Salaheldin, E.O., Arriola-Montenegro, L., Yaseen, A. et al. Late Presentation of D-TGA Complicated by Functional Glenn Shunt Obstruction Led to SVC Syndrome 10 Years Later: a Rare Case Report. SN Compr. Clin. Med. 5, 181 (2023). https://doi.org/10.1007/s42399-023-01517-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-023-01517-w