Abstract
Calcitonin gene-related peptide (CGRP) has only recently emerged as a potential target in posttraumatic headache. To our knowledge, this is the first description of a patient with persistent posttraumatic headache following severe traumatic head injury who has been treated with the CGRP receptor monoclonal antibody erenumab. A 56-year-old man presented with a 30-year history of frequent migraine-like posttraumatic headaches following a high-voltage head injury that he treated with an excessive intake of peripheral analgesics. Although amitriptyline was reasonably effective, it had to be discontinued when the patient developed restless legs syndrome in the second year of treatment. Under therapy with erenumab, he achieved a rapid and stable reduction in his symptoms down to only 2–3 headache days per month without adverse events. This case demonstrates that the inhibition of the CGRP-receptor with erenumab could be an effective treatment option in migraine-like posttraumatic headache even decades after the traumatic event.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Severe posttraumatic headache (PTH) can have serious effects on the individual patient’s quality of life, particularly if it persists over a long period. However, the pathophysiological mechanisms of persistent PTH remain elusive [1] and there have been no targeted treatment approaches until now. Thus, treatment is usually guided by the recommendations for primary headache disorders [2].
Erenumab is an anti-CGRP receptor monoclonal antibody (CGRP, calcitonin gene-related peptide) and is effective in the prevention of episodic and chronic migraine [3, 4]. Interestingly, recent preclinical studies suggest a role of CGRP in the development of PTH [5, 6]. This case describes a 56-year-old man with a 30-year history of persistent migraine-like PTH who achieved significant reduction of pain and a remarkable improvement of his quality of life under therapy with erenumab.
Case Presentation
A 56-year-old man presented with frequent, severe headache attacks that persisted since a high-voltage electrical injury 30 years ago. During a work-related accident in the 1980s, current from a railway overhead line (15 kV) had entered through the right occipital region of the patient’s head and exited through the left foot. During a 2-month hospital stay, he underwent multiple operations. These included having to surgically remove parts of the skull bone and reconstruct the scalp with an advancement flap.
As a specialised accident hospital under the German Occupational Insurance Scheme we are specialised in the treatment and rehabilitation of patients who had a work-related accident. However, the patient presented himself at our hospital for the first time in 2016, 30 years after his accident. Medical records from his initial treatments and examinations were not available due to the time elapsed. The patient described a throbbing pain that emanated from the back of the head on the right and spread over the entire left side of the skull. He rated the pain intensity at 7–8 on a numerical rating scale (NRS 0–10). The attacks occurred on average at 12–13 days per month, lasted between 2 and 24 h, and were partly accompanied by nausea and vomiting. Furthermore, according to his partner, sometimes he had a ptosis on the left side during his attacks. No visual aura was present.
Apart from two initial, ineffective rehabilitation procedures and an interim attempt at acupuncture, over the past decades, pain management had merely consisted of medication with mainly peripheral analgesics as needed. It was only now that an attentive pharmacist, who had noticed the patient’s extensive need for painkillers, had suggested an evaluation by a pain specialist. At this time, the patient reported that his intake of ibuprofen, a fixed combination of ASA + paracetamol + caffeine, metamizole, and occasionally tramadol, amounted to more than 50 tablets each month (Table 1).
Clinical and neurological examination yielded normal results. Comorbid arterial hypertension was treated with lisinopril. Due to the frequent headaches, the patient had never been able to pursue a regular occupation and was prematurely retired aged 27. He accepted only offers of marginal employment with a maximum workload of 4 days per month, working as a test driver. His results from psychometric tests (German pain questionnaire in 2007) were in the range of chronic pain patients but with a depression score on a high normal level.
We diagnosed a persistent, migraine-like PTH. Despite the patient’s extremely frequent use of peripheral analgesics, we considered a medication-overuse headache (MOH) unlikely, since first, the pain location was strictly unilateral and second, the patient had experienced a pain-free period during a 2-week holiday which he managed to spend entirely without medication. As the pain stopped immediately and not gradually over time, we concluded his headache not to be associated with his medication. Furthermore, the accompanying migraine-like symptoms pointed towards the migraine-like phenotype of PTH, although initially a possible MOH could not be fully excluded. We are aware that the International Classification of Headache disorders 3 [7] does not include electric injury as a cause for PTH. However, because the attacks started shortly after his accident and because his headache attacks were accompanied by migraine-like symptoms over time, migraine-like PTH was the most obvious diagnosis in our opinion.
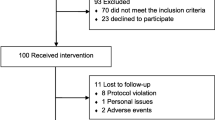
Figure 1 provides an overview over the patient’s pain management. The patient started treatment with amitriptyline up to 20 mg daily. He reported considerable relief especially in pain intensity and duration, which led to a substantial reduction in his analgesic medication (Table 1). He now was able to control the attacks solely with metamizole, which he used at 10 days/month (corresponding to 10 headache days/month). However, after 16 months of amitriptyline treatment, he developed restless leg syndrome (RLS). Since antidepressants are suspected to induce or worsen RLS [8], a switch to metoprolol was attempted. However, it was ineffective, the headaches markedly recurred, and the patient resumed amitriptyline in combination with levodopa/benserazide. In this way, he achieved satisfactory control of both headaches and RLS.
With additional intensive transcutaneous supraorbital nerve stimulation (t-SNS; Cefaly®, Cefaly Technology, Seraign, Belgium), the patient was able to discontinue amitriptyline after 2 years of treatment. He then reported intake of ibuprofen at 10 days/month (corresponding to 10 headache days/month) and levodopa/benserazide as needed every 4–5 days.
However, due to the side effects of this medication, such as fatigue, a dry mouth, and changes in sexual drive, the patient sought a treatment option with less side effects and therefore inquired about erenumab as an alternative. We informed the patient about erenumab being off-label for his indication and about potential risks associated with this antibody. Treatment started 8 months later (after approval of erenumab and approval of cost reimbursement) with monthly subcutaneous injections of 70 mg erenumab. After the first injection, the number of headache days per month had already declined to 2–3 and has remained stable over the 9 months of treatment so far. The patient reported that the remaining headache attacks mainly occurred during the last days before the next erenumab injection was due and treatment with ibuprofen was sufficient. Pain intensity was rated at NRS 4–5. He also discontinued t-SNS application. The patient has not experienced adverse events so far and is extremely satisfied with the treatment. The RLS remained stable and is currently treated with dermal application of rotigotine. After the initiation of erenumab treatment, the patient realised in retrospect that his social participation had been rather limited before and was now expanding. Among other activities, he had accepted more test-driving projects and had ventured on a holiday abroad.
Conclusions
This patient with persistent, migraine-like PTH only received structured pain management after 30 years of treatment with analgesics as needed. Unfortunately, this is not uncommon, as PTH remains an entity that is challenging to treat [9]. Often, the referral to a pain management specialist constitutes a hurdle that prevents patients from receiving optimal treatment. Only now, an attentive pharmacist who noticed the patient’s extensive need of painkillers suggested an evaluation by a pain specialist.
Although amitriptyline treatment was effective and the patient was able to drastically reduce his extensive use of analgesics, it transpired not to be the optimal treatment when the patient developed RLS. Although it remains unclear whether the RLS was actually induced by amitriptyline or was a late effect of the injury, discontinuation of treatment was advisable due to a substantial risk of worsening the RLS symptoms [8].
Erenumab rapidly and effectively reduced the number of headache days per month to 2–3, without the need for additional t-SNS application. This was the best outcome the patient had experienced since his accident over 30 years ago and it substantially improved his psychosocial conditions and life circumstances. Only then did he realise that he had been rather limited by the constant fear of provoking headache attacks that had accompanied him through his entire adult life.
Erenumab is a fully human monoclonal antibody directed specifically against the CGRP receptor. Unlike amitriptyline, it does not interfere with serotonin or histamine pathways and thus there is no reason for it to influence the existing RLS. Furthermore, the recently published results of the HER-MES trial showed that erenumab is superior to topiramate in migraine prophylaxis, in terms of tolerability and efficacy [10].
Regarding his 30-year pain history, we expect that this patient will require long-term erenumab treatment. The proven long-term efficacy and excellent safety profile over 5 years so far are thus reassuring [11]. Importantly, erenumab has a low interaction potential which is favourable considering the patient’s comedication.
Despite a very similar phenotype, migraine-like posttraumatic headache and primary migraine were shown to be associated with differences in brain structure in a recent study based on magnetic resonance imaging suggesting differences in pathophysiology [12]. However, this does not exclude a common role for CGRP as both entities are supposedly multifactorial processes and several publications underline a possible role for CGRP and its receptor also in PTH. Recent preclinical studies of mild traumatic brain injury, using rat models, showed that treatment with an anti-CGRP monoclonal antibody following concussion ameliorated pain-related behaviour and hypersensitivity in the acute phase [5, 6]. However, delayed administration of the CGRP inhibitor appeared to be ineffective in preventing persistent PTH in rodents which led the authors to the conclusion that GCRP was mainly involved in the development of central sensitisation after the event and was thus associated with promoting (but not sustaining) persistent PTH [6].
La Fountaine et al. recently published the results of a small prospective study in athletes who incurred a concussion. The athletes were checked for single-nucleotide polymorphisms in one isoform of CGRP and a subunit of the CGRP receptor. They found that a specific combination of single-nucleotide polymorphisms resulted in a greater burden of acute PTH after concussion [13].
In a recent report, impressive results were obtained with erenumab in 7 severely symptomatic patients with acute migraine-like PTH secondary to mild traumatic head injury. The patients started treatment between 4 and 11 weeks after the trauma and all achieved a ≥ 95% reduction in headache days per month [14].
Furthermore, Ashina et al. conducted a single-arm, open-label study with erenumab for the prevention of persistent PTH attributed to mild traumatic brain injury. During the 12-week treatment period, erenumab reduced the monthly number of headache days by 2.8 days among 89 patients (baseline: 15.7 mean headache days per month) [15]. Additionally, in another study, Ashina et al. were able to induce migraine-like headache in a group of patients with a known history of persistent PTH attributed to mild traumatic brain injury by intravenous infusion of CGRP [16].
Lately, Ashina and Moskowitz published an article summarising the available data on a possible involvement of the trigeminovascular system in the pathophysiology of PTH. They concluded that the trigeminovascular system is the shared biological foundation of headache pathogenesis in both, PTH and migraine [17].
Taken together, there is increasing evidence that CGRP could play a role in PTH similar to its role in migraine. This would provide a possible explanation for the effectiveness of erenumab in our patient.
Our case provides a first observation that erenumab can also be effective in persistent PTH following severe traumatic head injury even decades after the onset of symptoms. Since persistent PTH is a common health issue, robust controlled studies on anti-CGRP receptor treatment should be undertaken.
Therefore, erenumab should be considered a therapy, which seems to be safe, convenient, and low in side effects in the treatment of persistent PTH with migraine-like phenotype.
Data availability
Not applicable.
Code availability
Not applicable.
Abbreviations
- ASA:
-
acetylsalicylic acid
- CGRP:
-
calcitonin gene-related peptide
- MOH:
-
medication-overuse headache
- NRS:
-
numerical rating scale
- PTH:
-
posttraumatic headache
- RLS:
-
restless leg syndrome
- t-SNS:
-
transcutaneous supraorbital nerve stimulation.
References
Defrin R. Chronic post-traumatic headache: clinical findings and possible mechanisms. J Man Manip Ther. 2014;22(1):36–44. https://doi.org/10.1179/2042618613Y.0000000053.
Larsen EL, Ashina H, Iljazi A, Al-Khazali HM, Seem K, Ashina M, et al. Acute and preventive pharmacological treatment of post-traumatic headache: a systematic review. J Headache Pain. 2019;20(1):98. https://doi.org/10.1186/s10194-019-1051-7.
Goadsby PJ, Reuter U, Hallstrom Y, Broessner G, Bonner JH, Zhang F, et al. A controlled trial of erenumab for episodic migraine. N Engl J Med. 2017;377(22):2123–32. https://doi.org/10.1056/NEJMoa1705848.
Tepper S, Ashina M, Reuter U, Brandes JL, Dolezil D, Silberstein S, et al. Safety and efficacy of erenumab for preventive treatment of chronic migraine: a randomised, double-blind, placebo-controlled phase 2 trial. Lancet Neurol. 2017;16(6):425–34. https://doi.org/10.1016/S1474-4422(17)30083-2.
Bree D, Levy D. Development of CGRP-dependent pain and headache related behaviours in a rat model of concussion: implications for mechanisms of post-traumatic headache. Cephalalgia. 2018;38(2):246–58. https://doi.org/10.1177/0333102416681571.
Navratilova E, Rau J, Oyarzo J, Tien J, Mackenzie K, Stratton J, et al. CGRP-dependent and independent mechanisms of acute and persistent post-traumatic headache following mild traumatic brain injury in mice. Cephalalgia. 2019;39(14):1762–75. https://doi.org/10.1177/0333102419877662.
Headache Classification Committee of the International Headache Society (IHS). International Classification of Headache disorders 3, German version. https://ichd-3.org/de/.
Kolla BP, Mansukhani MP, Bostwick JM. The influence of antidepressants on restless legs syndrome and periodic limb movements: a systematic review. Sleep Med Rev. 2018;38:131–40. https://doi.org/10.1016/j.smrv.2017.06.002.
Seifert TD, Evans RW. Posttraumatic headache: a review. Curr Pain Headache Rep. 2010;14(4):292–8. https://doi.org/10.1007/s11916-010-0117-7.
Reuter U, Ehrlich M, Gendolla A, Heinze A, Klatt J, Wen S, et al. Erenumab versus topiramate for the prevention of migraine - a randomised, double-blind, active-controlled phase 4 trial. Cephalalgia. 2022;42(2):108–18. https://doi.org/10.1177/03331024211053571.
Ashina M, Goadsby PJ, Reuter U, Silberstein S, Dodick DW, Xue F, et al. Long-term efficacy and safety of erenumab in migraine prevention: results from a 5-year, open-label treatment phase of a randomized clinical trial. Eur J Neurol. 2021; https://doi.org/10.1111/ene.14715.
Schwedt TJ, Chong CD, Peplinski J, Ross K, Berisha V. Persistent post-traumatic headache vs. migraine: an MRI study demonstrating differences in brain structure. J Headache Pain. 2017;18(1):87. https://doi.org/10.1186/s10194-017-0796-0.
La Fountaine MF, Hohn AN, Leahy CL, Weir JP, Testa AJ. Observations from a prospective small cohort study suggest that CGRP genes contribute to acute posttraumatic headache burden after concussion. Front Neurol. 2022;13:947524. https://doi.org/10.3389/fneur.2022.947524.
Charles JA. Treatment of posttraumatic headache migraine phenotype with erenumab – An observational study. J Concussion. 2019;3:1–4. https://doi.org/10.1177/2059700219878292.
Ashina H, Iljazi A, Al-Khazali HM, Eigenbrodt AK, Larsen EL, Andersen AM, et al. Efficacy, tolerability, and safety of erenumab for the preventive treatment of persistent post-traumatic headache attributed to mild traumatic brain injury: an open-label study. J Headache Pain. 2020;21(1):62. https://doi.org/10.1186/s10194-020-01136-z.
Ashina H, Iljazi A, Al-Khazali HM, Do TP, Eigenbrodt AK, Larsen EL, et al. CGRP-induced migraine-like headache in persistent post-traumatic headache attributed to mild traumatic brain injury. J Headache Pain. 2022;23(1):135. https://doi.org/10.1186/s10194-022-01499-5.
Ashina H, Moskowitz MA. Shared biological foundations of post-traumatic headache and migraine. Headache. 2021;61(3):558–9. https://doi.org/10.1111/head.14084.
Acknowledgements
The authors thank Rainer Lauterbach, Ph.D., of Novartis Pharma GmbH, Germany, and Sonja Hergeth, Ph.D., of medizinwelten-services GmbH, Stuttgart, Germany, for providing medical writing/editorial support, and Reiner Czaniera of Novartis Pharma GmbH, Germany, and Daniela Mailänder-Sánchez, Ph.D., of medizinwelten-services GmbH, Stuttgart, Germany, for providing editorial support for the revision of this manuscript which was funded by Novartis Pharma GmbH, Germany, in accordance with Good Publication Practice Guidelines.
Funding
Open Access funding enabled and organized by Projekt DEAL and the Open Access Publication Fund of the University of Duisburg-Essen. Medical writing support was funded by Novartis Pharma GmbH.
Author information
Authors and Affiliations
Contributions
MP: conception, drafting, final approval, agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
MD: funding acquisition, critically revising, and adding important intellectual content
MP and MD: All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval
Ethics approval was not required since this report describes a case from routine clinical practice.
Consent to participate
Consent to participate was not required since this report describes a case from routine clinical practice.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Papenhoff, M., Dudda, M. Treatment of Persistent Posttraumatic Headache with the Anti-CGRP Receptor Antibody Erenumab: a Case Report. SN Compr. Clin. Med. 5, 169 (2023). https://doi.org/10.1007/s42399-023-01503-2
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-023-01503-2