Abstract
Though initially believed to primarily be a respiratory pathogen, the SARS-CoV-2 virus has manifested as a virus that has the potential to affect multiple organ systems causing a wide variety of disease and symptomatology. Children have been largely spared in comparison to adult morbidity and mortality; however, acute pediatric illness secondary to COVID-19 infection has become both more common and more serious. Here, we present a teenager with acute COVID-19 who presented to the hospital with profound weakness and oliguria and was discovered to have severe rhabdomyolysis causing life-threatening hyperkalemia and acute kidney injury. He required treatment with emergent renal replacement therapy in the intensive care unit. His initial CK was 584,886 U/L. Creatinine was 14.1 mg/dL and potassium was 9.9 mmol/L. He was successfully treated with CRRT and was discharged on hospital day 13 with normal kidney function on follow-up. Rhabdomyolysis and acute kidney injury are increasingly recognized as complications of acute SARS-CoV-2 infection and require vigilance given the potentially fatal complications and long-standing morbidity associated with these conditions.
Similar content being viewed by others
Introduction
Over the past few years, the world has faced the coronavirus disease 2019 (COVID-19) pandemic with uncertainty. At the beginning of the pandemic, the clinical illness caused by the SARS-Cov-2 virus was thought to be primarily a respiratory illness that encompassed a wide spectrum of clinical severity. Children were initially believed to be mostly spared from the effects of COVID-19; however, this notion was quickly disproven. Not only are children susceptible to respiratory disease caused by the virus, but children are also susceptible to a post-COVID disorder—multisystem inflammatory syndrome in children, or MIS-C [1, 2]. MIS-C is a hyperinflammatory disease marked by persistent fever, temporal relation to infection with SARS-CoV-2, and evidence of inflammatory changes in at least two organ systems [3]. Acute kidney injury (AKI) has been a documented complication of both SARS-CoV-2 viral infection and MIS-C, believed to be primarily a consequence of dehydration and inflammation [1]. As increasing numbers of children are infected with SARS-CoV-2, novel presentations of acute infection are emerging. While COVID-19-associated rhabdomyolysis has been observed in the adult population, it is rarer in pediatric patients [4]. Furthermore, while COVID-19-associated rhabdomyolysis has been observed in children, it rarely causes serious life-threatening morbidity [5]. Here, we present the case of a COVID-19-positive adolescent with severe rhabdomyolysis causing critical AKI and life-threatening hyperkalemia necessitating emergent dialysis in the pediatric intensive care unit (PICU).
Case Presentation
A 15-year-old male presented to a local emergency department (ED) with emesis, diarrhea, weakness, myalgias, and decreased oral intake. His past medical history was pertinent only for obesity with a BMI of 32 and attention deficit hyperactivity disorder for which he took Adderall XR. For 2 days prior to presentation, he had only urinated once per day. His symptoms were preceded by a mild cough, which had since resolved. At the time of presentation, he required assistance with ambulation. He denied any other symptoms including fever, chest pain, and dyspnea. He had not been ill in the previous 3 months. In the ED, the patient was described as minimally active, was afebrile, and had a positive viral polymerase chain reaction (PCR) test for SARS-CoV-2. He had not been previously vaccinated. The remainder of his respiratory pathogen PCR panel was negative. His laboratory tests at that time were significant for serum sodium 123 mmol/L, potassium 9.9 mmol/L, blood urea nitrogen (BUN) 116 mg/dL, creatinine 14.1 mg/dL, ionized calcium 0.77 mmol/L, aspartate amino transferase (AST) 2086 U/L, alanine amino transferase (ALT) 533 U/L, C-reactive protein (CRP) 42 mg/dL, creatinine kinase (CK) 584886 U/L, CK-MB 17.3 ng/mL, troponin-I 0.043 ng/mL, and procalcitonin 2.26 ng/mL. Results of B-type natriuretic peptide (BNP), albumin, bilirubin, alkaline phosphatase, and complete blood count were normal. An electrocardiogram (ECG) showed sinus rhythm with significantly peaked T-waves. He was given 1 L of intravenous fluid, 1 g of calcium gluconate, 100 mEq of sodium bicarbonate, 10 units of insulin with concentrated dextrose fluid, and Kayexalate. He was then placed on maintenance fluids at 100 mL/hr and was transferred to our tertiary care children’s hospital with a presumed diagnosis of severe viral-induced rhabdomyolysis.
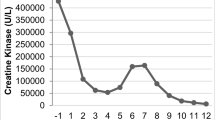
On admission to the PICU, the patient was somnolent, with a blood pressure of 142/83 mmHg, respiratory rate of 25 breaths per minute, pulse oximetry oxygen saturation of 100% on room air, and temperature of 36.9 °C. The patient’s serum potassium remained elevated at 8.4 mmol/L with BUN of 119 mg/dL and a creatinine of 11.3 mg/dL, and T-waves remained peaked on telemetry. For persistent symptomatic severe hyperkalemia, an additional liter of fluid was administered followed by 80 mg (about 0.8 mg/kg of actual body weight) of furosemide without improvement, so continuous renal replacement therapy (CRRT) was initiated after consultation with pediatric nephrology. A kidney ultrasound showed echogenic kidneys and no structural abnormalities. Additional pertinent lab tests included troponin which peaked at 1972 ng/L on hospital day 2, ferritin 1103 ng/mL, fibrinogen which peaked at 559 mg/dL on hospital day 3, sedimentation rate which peaked at 71 mm/hr on hospital day 4, and d-dimer which peaked at 3961 ng/mL on hospital day 10. Early in his CRRT course, he had significant ongoing hyperkalemia despite a low potassium bath, related to ongoing rhabdomyolysis (Fig. 1). The patient’s CK decline significantly with initiation of CRRT and continued to downtrend throughout his hospitalization (Fig. 2). CRRT was discontinued on hospital day 6 due to improving kidney function and urine output. He required intermittent hemodialysis once on hospital day 8, after which his kidney function and electrolytes remained stable.
The patient was notably hypertensive for age with systolic blood pressure range approximately 130–180 and diastolic blood pressure range of approximately 60–80. This was treated with effectively with esmolol and nicardipine infusions followed by amlodipine which was continued at discharge. Two echocardiograms obtained during his hospitalization showed normal cardiac function without evidence of myocarditis. He received full anticoagulation with heparin while on dialysis and was transitioned to venous thromboembolism prophylaxis, which was continued until his mobility improved given the risk of thrombosis in the setting of decreased mobility and acute COVID-19 infection. This was not continued at discharge. At the time of admission, the patient received one dose of intravenous immunoglobulin (IVIG) prior to completion of the full diagnostic evaluation given his degree of illness and the concern for MIS-C versus active COVID-19 disease. Daily dexamethasone was initiated on hospital day 3 given stagnant inflammatory markers. He completed a 10-day course with improvement in his inflammatory markers. COVID spike protein IgG and nucleocapsid IgG tests were positive, but the patient was at least 10–14 days out from initial infection and the constellation of symptoms more closely resembled active infection [5,6,7,8,9,10,11]; thus, the patient was presumed to have active COVID-19 and not MIS-C. He was able to transfer to the inpatient pediatric floor on hospital day 10 at his baseline mental status and was discharged home on hospital day 13. On 1-month follow-up, his creatinine was within normal range with no proteinuria and normal blood pressures. Amlodipine was discontinued.
Conclusions
COVID-19 symptomatology manifests variably across both the adult and the pediatric populations. AKI is a known complication of acute COVID infection and MIS-C in pediatric patients with the cause being likely multifactorial and is associated with increased morbidity and mortality [1, 2, 12, 13]. This example of rhabdomyolysis and AKI associated with acute COVID infection is currently one of only a few reported cases [6,7,8,9, 11, 14].
Rhabdomyolysis is a clinical syndrome in which striated muscle tissue breakdown leads to release of products such as CK, potassium, and myoglobin, which is nephrotoxic when released in amounts that overwhelm protein binding capacity [15]. This direct renal tubular injury and pre-renal hypovolemia caused by fluid sequestration in damaged muscle are major contributors to kidney injury. In children, causes of rhabdomyolysis include viral infection, trauma, toxic ingestion, medications, underlying rheumatologic or metabolic disease, malignant hyperthermia, seizures, and strenuous exercise [15, 16]. Viral infection is one of the most common causes in children, with influenza most frequently implicated. Complications of rhabdomyolysis in children include compartment syndrome caused by muscle ischemia and subsequent fluid sequestration, hypovolemia, calcium and phosphorus derangements, and hyperkalemia, which can be life-threatening. AKI is a common complication, though it is rare for children to require dialysis as a complication of rhabdomyolysis, especially if it is diagnosed and treated early. Dialysis is required in the setting of life-threatening hyperkalemia and anuria [15, 16].
Rhabdomyolysis caused by SARS-CoV-2 is likely multifactorial. A proposed mechanism, unique to SARS-CoV-2 as compared to other viral-induced myositis, is direct muscle cell invasion via the ACE-2 receptor. Extrapulmonary effects of COVID-19 are thought to be mediated by the binding of SARS-CoV-2 spike proteins to ACE-2 receptors on small vessel endothelial cells, thereby causing endothelial damage. ACE-2 receptors are expressed on muscle cells, and damage is thought to occur by direct deposit of genetic material into myocytes via the spike protein and ACE-2 receptor binding mechanism [17]. Another mechanism thought to indirectly contribute to muscle damage is the up-regulation of T-cells resulting in increased inflammation. This hyperinflammatory state is characterized by elevations in pro-inflammatory cytokines and formation of antigen-antibody complexes which can be deposited in the musculature. Finally, SARS-CoV-2 viral antigens can inappropriately bind to myocytes via molecular mimicry with ensuing immunologic activation and destruction of myocytes [17].
The most common cause of rhabdomyolysis in pediatric patients is viral, and given the ever-growing list of clinical morbidities caused by COVID-19 infection, it may perhaps be unsurprising that it, too, causes rhabdomyolysis. However, when reviewing previous case reports of rhabdomyolysis in pediatric patients with COVID-19, the degree of CK elevation was often striking, reaching upwards of 400,000 U/L. Interestingly, these patients did not develop AKI [6, 7, 10]. Another case report of a 15-year-old male showed a CK of 22,000 U/L; however, that patient did develop AKI [8]. A small case series of eight children showed no significant morbidity and maximum CK of 7000 [5]. In all of these cases, the patients recovered with just supportive care [5,6,7,8, 10]. Mahajan et al. described a patient who developed multiorgan failure as well as rhabdomyolysis (CK upwards of 55,000 U/L) and subsequently went on to need CRRT. Given the severity and complexity of the patient’s illness, it would be difficult to attribute their AKI solely to rhabdomyolysis [18]. When assessing rates of severe AKI from rhabdomyolysis in the pediatric population not related to COVID-19, Mannix et al. observed that only one of the 191 patients they identified in a 10-year period who met criteria for rhabdomyolysis went on to require dialysis [16]. Multiple studies regarding AKI without rhabdomyolysis in pediatric patients have shown exceedingly low rates of renal replacement therapy [1, 2, 12].
The patient we presented in this case report was unique because his CK reached nearly 600,000 U/L and developed severe anuric AKI with hyperkalemia requiring emergent dialysis, but no other symptoms or organ failures from COVID-19 infection. The commonalities that emerged from the handful of case reports of pediatric patients with both COVID-19 and rhabdomyolysis were that the more severe cases were in adolescents. Two of the four more critically ill adolescents were also noted to be obese; BMI was not mentioned in the other two [6,7,8, 10]. These numbers are far too low to even begin to speculate with regards to risk factors for development of severe rhabdomyolysis; nonetheless, it is important for clinicians to be aware of the varied presentations and potentially fatal complications of rhabdomyolysis in patients infected with COVID-19. Given the growing number of cases and the potential for severe disease with lasting morbidity, clinicians should maintain a high index of suspicion for the development of rhabdomyolysis in their patients suffering from the COVID-19 disease.
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Basalely A, Gurusinghe S, Schneider J, Shah SS, Siegel LB, Pollack G, et al. Acute kidney injury in pediatric patients hospitalized with acute COVID-19 and multisystem inflammatory syndrome in children associated with COVID-19. Kidney Int. 2021;100(1):138–45. https://doi.org/10.1016/j.kint.2021.02.026.
Raina R, Chakraborty R, Mawby I, Agarwal N, Sethi S, Forbes M. Critical analysis of acute kidney injury in pediatric COVID-19 patients in the intensive care unit. Pediatr Nephrol. 2021;36(9):2627–38. https://doi.org/10.1007/s00467-021-05084-x.
Henderson LA, Canna SW, Friedman KG, Gorelik M, Lapidus SK, Bassiri H, et al. American College of Rheumatology clinical guidance for multisystem inflammatory syndrome in children associated with SARS-CoV-2 and hyperinflammation in pediatric COVID-19: version 3. Arthritis Rheumatol. 2022;74(4):e1–e20. https://doi.org/10.1002/art.42062.
Haroun MW, Dieiev V, Kang J, Barbi M, Marashi Nia SF, Gabr M, et al. Rhabdomyolysis in COVID-19 patients: a retrospective observational study. Cureus. 2021;13(1):e12552. https://doi.org/10.7759/cureus.12552.
Wu PS, Wong SB, Cheng CF, Yu CH. Rhabdomyolysis in pediatric patients with SARS-CoV-2 infection. Children (Basel). 2022;9(10):1441. https://doi.org/10.3390/children9101441.
Gefen AM, Palumbo N, Nathan SK, Singer PS, Castellanos-Reyes LJ, Sethna CB. Pediatric COVID-19-associated rhabdomyolysis: a case report. Pediatr Nephrol. 2020;35(8):1517–20. https://doi.org/10.1007/s00467-020-04617-0.
Samies NL, Pinninti S, James SH. Rhabdomyolysis and acute renal failure in an adolescent with coronavirus disease 2019. J Pediatric Infect Dis Soc. 2020;9(4):507–9. https://doi.org/10.1093/jpids/piaa083.
Tram N, Chiodini B, Montesinos I, Vicinanza A, Beretta-Piccoli X, Gubbelmans N, et al. Rhabdomyolysis and Acute Kidney Injury as Leading COVID-19 Presentation in an Adolescent. Pediatr Infect Dis J. 2020;39(10):e314–e5. https://doi.org/10.1097/INF.0000000000002853.
Anwar H, Al LA. Adolescent COVID-19-Associated datal rhabdomyolysis. J Prim Care Community Health. 2020;11:2150132720985641. https://doi.org/10.1177/2150132720985641.
Gilpin S, Byers M, Byrd A, Cull J, Peterson D, Thomas B, et al. Rhabdomyolysis as the initial presentation of SARS-CoV-2 in an adolescent. Pediatrics. 2021;147(3):e2020019273. https://doi.org/10.1542/peds.2020-019273.
Jin M, Tong Q. Rhabdomyolysis as potential late complication associated with COVID-19. Emerg Infect Dis. 2020;26(7):1618–20. https://doi.org/10.3201/eid2607.200445.
Wang X, Chen X, Tang F, Luo W, Fang J, Qi C, et al. Be aware of acute kidney injury in critically ill children with COVID-19. Pediatr Nephrol. 2021;36(1):163–9. https://doi.org/10.1007/s00467-020-04715-z.
Kari JA, Shalaby MA, Albanna AS, Alahmadi TS, Alherbish A, Alhasan KA. Acute kidney injury in children with COVID-19: a retrospective study. BMC Nephrol. 2021;22(1):202. https://doi.org/10.1186/s12882-021-02389-9.
Suwanwongse K, Shabarek N. Rhabdomyolysis as a presentation of 2019 novel coronavirus disease. Cureus. 2020;12(4):e7561. https://doi.org/10.7759/cureus.7561.
Elsayed EF, Reilly RF. Rhabdomyolysis: a review, with emphasis on the pediatric population. Pediatric nephrology (Berlin, West). 2010;25(1):7–18. https://doi.org/10.1007/s00467-009-1223-9.
Mannix R, Tan ML, Wright R, Baskin M. Acute pediatric rhabdomyolysis: causes and rates of renal failure. Pediatrics. 2006;118(5):2119–25. https://doi.org/10.1542/peds.2006-1352.
Saud A, Naveen R, Aggarwal R, Gupta L. COVID-19 and myositis: what we know so far. Curr Rheumatol Rep. 2021;23(8):63. https://doi.org/10.1007/s11926-021-01023-9.
Mahajan R, Lipton M, Broglie L, Jain NG, Uy NS. Eculizumab treatment for renal failure in a pediatric patient with COVID-19. J Nephrol. 2020;33(6):1373–6. https://doi.org/10.1007/s40620-020-00858-2.
Author information
Authors and Affiliations
Contributions
- Danielle Geeting, MD, did the original chart review, data gathering, draft writing, and gathering of references. She also participated in the review and submission process.
- Palen Mallory, MD, also gathered references and participated in draft writing and reviewing the manuscript.
- Omar Alibrahim, MD, reviewed the case, reviewed drafts, and helped with the submission process.
- Mital Patel, MD, reviewed the case and participated in the draft writing and editing process.
- Reeti Kumar, MD, reviewed the case and participated in the draft writing and editing process.
Corresponding author
Ethics declarations
Ethics Approval
This article does not contain any studies with human participants or animals performed by any of the authors. Ethical approval is not required for the retrospective analysis of this case.
Consent to Participate
Written informed consent was obtained from the patient’s parent for publication of this case report.
Consent for Publication
Consent for publication was given by all authors and necessary parties prior to submission.
Conflict of Interest
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Covid-19
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Geeting, D., Alibrahim, O., Patel, M. et al. COVID-19 and Severe Rhabdomyolysis Causing Acute Kidney Injury and Life-Threatening Hyperkalemia in a Pediatric Patient: a Case Report. SN Compr. Clin. Med. 5, 121 (2023). https://doi.org/10.1007/s42399-023-01453-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-023-01453-9