Abstract
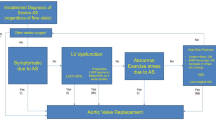
In patients with aortic stenosis, current guidelines recommend valve replacement therapy in case of severe valve narrowing in combination with symptoms and/or left ventricular dysfunction (ejection fraction < 50%). It is increasingly recognized that left ventricular ejection fraction offers a crude interpretation of a complex disease entity that is in need of refinement to optimize the timing of valve replacement therapy and patient outcome. In this state-of-the-art review article, we discuss the pathophysiological transition from left ventricular hypertrophy to other types of cardiac remodeling and myocardial fibrosis in response to progressive narrowing of the aortic valve, and how new imaging developments and biomarkers may help identify patients with a dismal outcome at earlier stages of disease. Also, the digital transformation of health care and novel analytical methods such as artificial intelligence that can help improve treatment decision is evaluated. This is in combination with the increased use of minimally invasive treatment modalities that may fulfill the goal of offering valve replacement in patients with aortic stenosis at earlier stages of disease and prior to the onset of symptoms but nevertheless at risk of left ventricular deterioration.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acquired aortic valve stenosis (AoS) is a degenerative valvular heart disease whose incidence increases with age [1, 2]. It exposes the left ventricle (LV) to a progressive increase in afterload, leading to changes in cardiac structure, function, and morphology (remodeling) [3,4,5]. Typically, the cardiomyocytes respond with an increase in cell size (myocyte hypertrophy) and consequently cardiac mass (left ventricular hypertrophy, LVH). LVH is considered an initially reversible and adaptive process to restore LV wall stress and maintain cardiac function, but may progress to irreversible changes with loss of function and, ultimately, death [6, 7]. This is explained by the fact that, in addition to an increase in myocyte cell size, LVH also entails deposition of collagen in the extracellular matrix, which is the hallmark of myocardial fibrosis [4, 5, 8, 9].
The genetic and molecular mechanisms governing cellular hypertrophy, collagen deposition, and the gross morphologic expression of cardiac remodeling remain poorly understood [10]. They have an insidious onset, which precede clinical manifestations and—when present—are associated with a dismal prognosis (heart failure, mortality) [6].
In general, the indication for aortic valve replacement (AVR) is primarily based upon the assessment of AoS severity in combination with global LV (dys)function and/or symptoms using binary cut-off criteria. Yet, the response of the heart to increased afterload occurs during the early phases of the disease (e.g., moderate AoS) when cardiac structure and function are normal and are presently not incorporated in treatment decision-making. It is conceivable that AVR in these intermediate phases safeguards the LV from future (irreversible) deterioration and may be beneficial from a patient and society perspective [11]. This premise has become particularly relevant with the advent and increased use of transcatheter aortic valve replacement (TAVR) that, at variance with surgical aortic valve replacement (SAVR), obviates the need of general anesthesia, large surgical access, cardiac arrest, and cardiopulmonary bypass although transcatheter valve durability is yet to be determined. In this article, we discuss the pathophysiological basis favoring early AVR in AoS and how the digital transformation of health care and novel analytical methods such as artificial intelligence (AI) may help improve treatment decision in a patient-centered approach.
Methods
In this state-of-the-art review, the authors used PubMed as the source of information to extract articles focusing on developments in detecting pathophysiological changes in cardiac function and morphology in response to AoS. Additionally, articles related to the digital transformation of health care and novel analytical methods to enhance treatment timing were analyzed. The abovementioned keywords and the following MeSH terms were used: left ventricular hypertrophy, remodeling, myocardial fibrosis, advanced imaging, echocardiography, cardiac ultrasound, cardiac magnetic resonance, computed tomography, biomarkers, left ventricular dysfunction, digital health, artificial intelligence, deep learning, transcatheter aortic valve replacement/implantation, and surgical aortic valve replacement. The quality and citations of individual manuscripts were reviewed and non-English papers were excluded. A total of 75 articles were published between 2010 and 2022; older articles (n = 23) were included because of their historical value related to the natural history and pathophysiological changes in AoS.
Cardiac Performance and Hemodynamics
The function of the heart is to offer and maintain sufficient output of blood to meet the metabolic demands of the peripheral tissues (and itself) for which it needs large quantities of oxygen and adenosine 5-triphosphate (ATP). In normal conditions, ATP is mainly generated via fatty acid oxidation [4, 12]. In case of stress (e.g., increased afterload), the heart switches to other energy substrates via the upregulation of glucose uptake and glycolysis while reducing fatty acid oxidation, thereby mimicking fetal cardiac metabolism, to maintain function [13,14,15].
Cardiac output depends on the complex interplay between cardiac filling (preload), contractility and arterial resistance (afterload), and the autonomic nervous system [16, 17]. In healthy conditions, LV filling is associated with small changes in diastolic pressure reflecting preserved diastolic function (i.e., myocardial relaxation). In illness such as AoS, the LV is exposed to an increase in afterload and intracardiac pressures and, thus, myocardial wall tension (Fig. 1a, b). The general view is that—in accordance with the law of Laplace [cardiac wall tension (T) = intracardiac pressure (P) × cardiac radius (r)/2 × wall thickness (h)]—the LV myocardium responds with “compensatory” hypertrophy to maintain wall tension within a normal range [7]. However, the concept that LVH is needed to maintain cardiac output is subject of debate as clinical observations reveal that not all patients with AoS have LVH on echocardiography upon presentation [18]. Also, longstanding experimental findings indicate that hypertrophy may not be needed for normalization of wall tension [10, 19].
Natural history of aortic valve stenosis. a Morphological features of progressive aortic valve stenosis. b Hemodynamic consequences for the left ventricle (increased left ventricular pressures). c Myocardial hypertrophy and cardiac remodeling. d Histologic hallmark of myocardial fibrosis. The drawing of the histologic hallmark, courtesy: de Boer et al., “Towards better definition, quantification and treatment of fibrosis in heart failure.” European Journal of Heart Failure (2019) 21, 272–285. e Clinical consequences of aortic valve stenosis. Early identification of patients at risk of unfavorable outcome may improve clinical outcomes by the use of minimally invasive therapies at an earlier disease stage. *The concept of providing a minimal invasive therapy (i.e., transcatheter aortic valve implantation) at earlier stages of disease and prior to the onset of symptoms and/or development of (irreversible) myocardial damage cannot be recommended until sound longevity data of transcatheter valves are available (expected in the next 5–10 years)
Myocardial Hypertrophy and Cardiac Remodeling
The heart responds to physiologic (e.g., exercise) and pathologic stress (e.g., AoS) by an increase in cardiomyocyte cell size (hypertrophy) and a change in cardiac morphology (remodeling). Interestingly, the heart has the ability to make the distinction between physiologic and pathologic stress as different molecular and cellular signaling pathways are activated [3, 10, 20]. In clinical practice, the increase in cardiomyocyte cell size cannot be measured. Yet, non-invasive imaging allows the measuring of myocardial thickness as a marker of mass as well as the global morphologic structure and changes (remodeling) of the heart [21].
The effects of myocardial hypertrophy on the ventricular cavity and hence global morphology vary. LVH may be associated with an increase, decrease, or no change in ventricular volume. To account for the proportionality between wall thickness and ventricular volume, distinction is made between three phenotypes of remodeling, namely concentric remodeling, concentric hypertrophy, and eccentric hypertrophy [3]. Concentric remodeling is defined by an increase in relative wall thickness (i.e., wall thickness relative to end-diastolic diameter) with normal cardiac mass (g/m2). Concentric hypertrophy is defined by an increase in relative LV wall thickness and cardiac mass with little or no change in LV volume due to the addition of sarcomeres in parallel and lateral growth of cardiomyocytes. Eccentric hypertrophy is defined by an increase in cardiac mass with increased LV volume (with normal, decreased, or increased relative wall thickness) due to the addition of sarcomeres in series and longitudinal cell growth. In short, concentric hypertrophy is characterized by an increase in mass with no or little changes in volume while eccentric hypertrophy is characterized by an increase in both mass and volume (Fig. 1c).
The reason why one patient with AoS presents with one type of remodeling or the other and whether or not one precedes the other is unknown. Clinical observations indicate that in addition to the severity of valve stenosis, non-valve-related factors such as age [22], gender [23], and metabolic disorders (e.g., obesity [24], diabetes [25]) play a role in addition to ischemic heart disease [26] and arterial stiffening. For instance, it has been shown that the total amount of LV afterload in AoS (valvular plus arterial component or valvulo-arterial impedance) better correlates with LV wall thickness than AoS severity itself [27].
Myocardial Fibrosis
Cardiomyocytes are embedded within the myocardial extracellular matrix (ECM), which constitutes approximately 25% of the total cardiac mass (Fig. 1d). It is a collagen network produced by fibroblasts with a honeycomb structure surrounding the individual cardiomyocytes and myocardial blood vessels [28, 29]. The ECM provides structural integrity and supports myocardial function via the handling and transmission of mechanical forces during the cardiac cycle.
Upon pathologic stress, fibroblasts [30] and collagen-secreting bone marrow–derived cells [31] differentiate into secreting myofibroblasts, leading to excess collagen deposition within the ECM which is named myocardial interstitial fibrosis (MIF) [8, 32, 33]. In AoS, MIF is characterized by increased synthesis and deposition of collagen I more than III outweighing their degradation and removal [34]. MIF starts at the subendocardial layer and is initially diffuse and reversible [35]. The expansion of the ECM contributes to myocyte loss, stimulating replacement fibrosis (RF) that occurs at the site of eliminated myocytes and is focal and irreversible [4, 8, 32, 36] (Fig. 1d). According to cardiac magnetic resonance imaging studies in both symptomatic and asymptomatic AoS patients, RF may progress rapidly especially in association with advanced valve narrowing and established RF. Interestingly, upon the first sign of RF, further scarring accumulates as fast as 75% each year impairing myocardial performance and heralding a grim prognosis [9, 37,38,39,40,41]. Although RF seems equally prevalent in older (≥ 70 years) [18, 37, 40, 42, 43] and younger (< 70 years) [9, 38, 39] patients, age remains an important determinant of adverse outcome irrespective of RF [38, 44]. Presence or absence of bicuspid valve morphology seems unrelated to fibrosis development [38, 42].
An early functional or hemodynamic effect of myocardial fibrosis is stiffening of the left ventricle (LV) and, consequently, diastolic dysfunction [33]. The degree of stiffness depends on the amount of fibrosis and the mechanical properties of the collagen fibers. For instance, collagen type I that is more abundant in AoS exhibits greater stiffness due to altered cross-linking than collagen III [34, 45, 46]. In addition, realignment of collagen fibers affects the transmission of force generated by the cardiomyocytes and henceforth systolic function [47]. The varying degree of deposition and cross-linking offers the identification of MIF subphenotypes with different prognostic effects with patients exhibiting severe deposition and cross-linking faring the worst [33, 48]. In addition, myocardial stiffening is also explained by changes in the architecture of the cardiomyocyte cytoskeleton (protein isoforms), a response that varies from patient to patient [49, 50]. Regression of myocardial stiffening generally occurs after afterload correction but is indeterminate.
Myocardial Fibrosis Detection
The premise is that AVR may be beneficial in the early phase of disease to prevent myocardial deterioration, impairment of quality of life, heart failure, and death (Fig. 1e). It implies the tools to detect early (subclinical) changes of myocardial structure (fibrosis) and cardiac function and/or a more refined method of disease phenotyping elucidating which patients are at (increased) risk of LV deterioration or dismal prognosis [9, 42, 43].
Cardiovascular magnetic resonance (CMR) is currently the best tool for non-invasive detection of MIF and RF [51]. MIF can be detected by native (pre-contrast) T1 mapping as T1 times are prolonged in MIF due to the accumulation of water. Yet, clinical interpretation of T1 times is hindered by a significant overlap between diseased and healthy myocardium and dependence upon CMR settings such as field strength and sequence [52]. RF can be detected by the administration of gadolinium, an extracellular contrast agent that accumulates in areas affected by fibrosis reducing T1 times in comparison to regions of normal myocardium [51].
The combination of T1 mapping and late gadolinium enhancement (LGE) allows the calculation of the extracellular volume (ECV) fraction, which is the space occupied by the ECV relative to the cardiomyocyte tissue and reflects the total interstitial space. The relation between ECV and MIF is, however, equivocal [53, 54]. Also, an increase in ECV fraction is a non-specific marker as it is seen not only in AoS but also in myocardial inflammatory and infiltrative disease and ischemia [55, 56]. Interpretation of CMR images, hence, demands the integration of patient demographics (age, gender) and clinical context [57]. LGE and ECV assessments do not provide qualitative information of collagen fibers [54]. This may be achieved with diffusion tensor CMR (DF-CMR) by assessing cardiac microstructure at a cellular level but is currently in an experimental phase [58]. In addition to the need of robust clinical expertise (settings, interpretation), CMR is cumbersome (e.g., patients with cardiac devices and/or claustrophobia), expensive, and not bedside available. Whether cardiac computed tomography (CCT) with iodine-based contrast administration will replace CMR for 3D ECV quantification remains to be seen [59].
Myocardial Dysfunction Detection
At variance with CMR, echocardiography is broadly available, simpler to perform, and—similar to CMR—extensively validated. Accordingly, it is the ideal clinical tool for the detection of disease, its effects on cardiac function and morphology plus evolution. With respect to the evaluation of cardiac function, several markers are available with those of diastolic dysfunction preceding those of systolic dysfunction. They are sensitive but non-specific, thereby requiring incorporation of the past medical history, comorbidities, age, and gender for the proper interpretation of their relationship with disease.
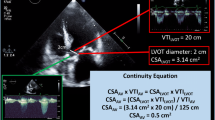
Currently, guidelines recommend LVEF < 50% as cut-point for AVR in some clinical scenarios (AoS with low flow or asymptomatic AoS) [60]. LVEF is a measure of the volumetric changes during the cardiac cycle and is defined by the end-diastolic minus end-systolic volume (EDV-ESV) relative to the EDV (EDV-ESV/EDV). As such, it is a crude proxy of global cardiac function that, moreover, is affected by the loading conditions of the heart at the moment of assessment (e.g., volume status/preload, blood pressure/afterload), inotropy (e.g., B-blockers), and associated valvular disease (e.g., mitral or aortic regurgitation/LV pre- and afterload) in addition to eventual morphologic changes due to the disease for which the patient is referred for examination (e.g., small cavity size due to LVH in AoS). Also, LVEF does not provide information on regional myocardial function.
For that reason, myocardial strain analysis using speckle tracking echocardiography (STE) may be more helpful [61]. Strain analysis using speckle tracking is based upon the myocardium (speckle pattern) allowing the assessment of motion and deformation (i.e., strain) of different myocardial regions and, as such regional and global and myocardial (dys)function [62, 63]. Strain is the change in dimension of an object (e.g., tissue) from its reference or resting state when subjected to a load. STE offers a multidirectional evaluation of the myocardium in the radial, circumferential, and longitudinal axis obviating the need of beam alignment with the motion direction of the myocardium. Of all STE-derived measures, global longitudinal strain (GLS) is the most robust and reproducible parameter. It measures systolic shortening of the LV wall capable of unveiling functional changes when the LVEF is still normal [64,65,66]. Yet and similar to LVEF, GLS is a relative measure of global LV function that depends on the loading conditions of the heart (preload, afterload), contractility, heart rate, and morphologic changes (remodeling) of the heart. In addition, its value is automatically generated by vendor-specific software precluding comparison of values derived from different machines [67].
Instead of measuring deformation (strain), one can also assess the rate at which deformation occurs (strain rate). Strain rate is less dependent on loading conditions but is limited by insufficient reproducibility due to the need of correct alignment of the tissue Doppler signal with cardiac tissue (angle dependency) and spatial resolution[68]. Early findings indicate that the 3D ultrasound shear-wave elasticity imaging for the quantification of myocardial stiffness may help identify patients with AoS at different levels of risk [69, 70]. In the absence of a technique unmistakably elucidating the state and etiology of myocardial (dys)function, the integration of the information derived from various (and serial) imaging techniques (CMR, echocardiography) in combination with patient’s history and laboratory findings (below) may at present be the best approach for more refined prediction of symptom onset and outcome and, thus, the timing of AVR.
Blood Biomarkers of LV Wall Stress and Fibrosis
The simplest technique—from a patient and hospital management perspective—for the detection of early myocardial dysfunction and/or fibrosis undoubtedly is the assessment of molecular markers by blood analysis. The most obvious ones are natriuretic peptides that are known to increase in response to pressure overload and cardiomyocyte stretch [71, 72]. This has been documented in patients with asymptomatic AoS and normal LVEF [73, 74]. Elevation of natriuretic peptides in such patients may, hence, reflect an already more advanced state of disease (myocardial dysfunction/fibrosis) suggesting the need of detecting disease at more earlier stages (e.g., aortic sclerosis detected via auscultation during routine GP examination or general health care control programs) and/or the need of markers unveiling cardiac dysfunction at such a stage. Since myocardial fibrosis precedes LV dysfunction, biomarkers of fibrosis may be helpful. High-sensitivity troponin-I (hsTnI) concerns a highly specific marker of myocardial injury that is associated with LGE and impaired outcome (i.e., AVR and death) [75]. As such, hsTnI is used to identify patients at risk for LGE and who might benefit from early AVR in the Early Valve Replacement Guided by Biomarkers of Left Ventricular Decompensation in Asymptomatic AoS (EVOLVED) trial [76]. Other candidate markers are galectin-3 (Gal-3) and collagen biomarkers (e.g., procollagen type III amino terminal peptides), which have been shown to be associated with heart failure and death [53, 77,78,79]. Their role in the management of patients with AoS remains elusive. Gal-3 did not outperform GLS and NT-proBNP in the prediction of prognosis in patients with AoS, and the correlation of the collagen biomarkers with myocardial fibrosis is subject of debate. This also holds for many other candidate markers including suppression of tumorigenicity 2 (ST2), C-reactive protein (CRP), and growth and differentiation factor-15 (GDF-15) [80]. Similar to other diagnostic challenges in medicine, the diagnostic value of blood biomarkers increments when interpreted in relation with other (clinical) factors. Chin et al. [44] recently demonstrated that hsTnI combined with other routine variables independently predicts presence of myocardial fibrosis and adverse outcome. Based on these variables, they developed the Aortic Stenosis Risk Score with high-risk patients carrying a tenfold higher risk of adverse outcome (death, heart failure, or new symptoms) as compared to low-risk patients, with a median time to event of 1.5 years.
The Role of Digital Health in the Early Detection of AOS
Acknowledging that the early detection of (reversible) myocardial fibrosis will remain questionable also when using CMR, one may consider shifting care to the early detection of AoS and its effects on LV performance and upstream cardiac remodeling. Digital health technology (DH) has the potential to revolutionize the early diagnosis of AoS by converging information and communication technologies in health care systems and society [81, 82]. This has become a credible possibility thanks to innovations in the domain of (1) sensors or detection tools of biomedical signals (invasive, non-invasive, remote), (2) transfer and storage of data, (3) analytical methods (artificial intelligence (AI) and deep learning (DL) in particular), and (4) computer power (e.g., quantum computing) [83,84,85,86,87].
AI-enabled analysis of the 12-lead ECG and heart sounds are exemplar of how DH can be helpful for the purpose defined above (Fig. 2). Digitization of biomedical signals has namely opened a vast array of novel data engineering (feature extraction, input) and analysis techniques (relationship between input data, output) unveiling “hidden” patterns that remain undetected by the human brain [84,85,86]. Human ECG analysis is based upon a visual semi-quantitative interpretation (feature extraction plus relationship) whose accuracy is dictated by experience and expertise. Computer or AI-enabled ECG analysis is based upon a set of predefined rules and, hence, a truncated pattern or feature recognition and assessment of those features with other patient-derived biomedical data (e.g., echocardiography), which is fully automated and unbiased (no a priori hypothesis). A number of observations have now shown that AI-enabled ECG analysis using DL and convolutional neural networks (CNN) is capable to detect AoS. Moreover, this does not only hold for the detection of AoS but also a host of other cardiac conditions of importance for the management of patients with AoS such as the detection of LVH, LV systolic and diastolic dysfunction, mitral regurgitation, silent atrial fibrillation, pulmonary capillary pressure, and pulmonary hypertension [85,86,87,88,89,90,91].
Role of digital health in the early detection of aortic stenosis. Biomedical data are collected at different locations (at home, GP practice, hospital, etc.) using different tools or sensors. Subsequently, the data are transferred and analyzed to exploit the capacity of artificial intelligence to identify features within these data and their relation with structural heart changes which would normally remain unrecognized by clinical interpretation and/or regular statistical analysis
Yet, the performance of those models and, hence, clinical utility depend not only on the AI model and architecture but also on the quality and completeness of the input data as well as the specificities of the population from which the data stem from (age, gender, ethnicity, baseline demographics, antecedents and comorbidity, etc.). These models may in theory detect the measures of interest such as LV hypertrophy and function and markers of upstream remodeling such as atrial fibrillation and pulmonary hypertension in populations these models have been developed. It remains to be seen whether they perform similarly in patients who were not used for model development (e.g., seen for a different reason at a different time and region).
Also, AoS is a disease with a relatively low prevalence. Consequently, when applied as an ambulatory screening tool in the general population (i.e., performed by general practitioners), the likelihood of a positive test will be low, of which a substantial number will be false positive. As such, the positive predictive value (PPV) will be low, and the negative predictive value (NPV) high. In other words, these models will serve well to exclude but not to confirm AoS. Unawareness of a high false-positive test rate may overwhelm the health care system by an inappropriate referral for echocardiography. This may be circumvented by the ambulatory AI-enabled heart sound analysis using the digital stethoscope (comparable to the expert cardiology heart sound analysis (Chorba et al., deep learning) to stratify patients for echocardiography and cardiology consultation in case a murmur is classified as AoS) (Fig. 2, [90, 92,93,94]). In the absence of such a murmur, patients with a false-positive test result might be followed more carefully since they are at a greater risk of developing AoS than those with true-negative test result [90].
As mentioned above, the current practice of the management of patients with AoS is guideline-based using cut-off values for treatment decision that in turn stem from survival data from populations in which all patients are considered similar based upon the presence of AoS. This is known to be a simplification of a complex reality. AI has been used to differentiate various subgroups of patients with a similar degree of AoS but with different prognoses or disease progressions. With respect to prognosis, three subgroups of patients with AoS were identified by cluster analysis: one with predominant cardiac dysfunction and high cardiovascular mortality, one comprising mostly elderly patients with prevalent comorbidities and increased cardiac and non-cardiac mortality, and a third subgroup of mainly “healthy” AoS patients with the best prognosis [95]. In high-risk patients with AoS such as those with concomitant pulmonary hypertension, cluster analyses identified subgroups with different prognoses based on alterations in left and right heart morphology [96]. With respect to disease progression, two pathways from mild-to-severe AoS have been uncovered by topological data analysis using cross-sectional echocardiographic data: one associated with preserved LV function and little LVH and the other with depressed LV function and increased LV mass [97]. Upstream adverse cardiac remodeling beyond the left ventricle (mitral valve apparatus, pulmonary circulation, tricuspid valve and right ventricle) is associated with impaired clinical outcomes [98]. These findings suggest that different molecular adaptive mechanisms may be involved in AoS progression and that different phenotypes are associated with different degrees of myocardial disease across the spectrum of AoS severity. AI may, thus, help refine treatment decision by offering AVR to those at risk of adverse events. In those with a benign prognosis, serial ECG assessment allows the creation of a patient-specific dashboard that helps expose a change in risk and, hence, timely treatment decision-making (Fig. 2). Whether an AI-enabled approach with its intrinsic limitations mentioned above and its complexity to execute will outperform regular echocardiographic follow-up remains to be determined.
In summary, we propose that adequateness of AoS treatment is based on specific individual characteristics and disease/patient interaction, thereby relying on the identification of those patients who will benefit the most from invasive treatment (utility vs. futility) as well as the appropriate time of intervention (early invasive vs. watchful waiting) in order to improve prognosis. In the foreseeable future, TAVR (relative to SAVR) may become the preferred therapy for AoS in lower risk patients at earlier stages of disease to prevent irreversible cardiac damage. In the absence of sound data on transcatheter valve durability, however, this cannot be recommended in contemporary practice yet. Identification and characterization of fibrosis in AoS patients may provide important prognostic clues, but adequate tools for this assessment are currently neither adequately validated nor ready for widespread use (availability, cost). Furthermore, although this information may shed some light in disease pathophysiology and progression, their implications in treatment (i.e., treatment/disease/patient interaction) are not clear and therefore, at the present time, treatment decisions should rely on the early detection of the disease through refined diagnostic tools such as the automatic ECG analysis together with automatic auscultation and accurate disease characterization and phenotyping. This, however, would implicate strict protocols that address appropriate referral for echocardiography to avoid overloading of the available resources. Given the likelihood of high sensitivity but low specificity of these diagnostic tools, it may be reasonable to combine both the automated ECG analysis and the smart stethoscope and refer for further testing only those with both tools pointing towards a high probability of severe AoS. Regardless, clinical expertise should always be above any AI tool and physicians should be aware that patients’ symptoms and clinical evaluation may warrant further investigation irrespective of screening results. Finally, the success of envisioned DH programs including the AI-enabled analysis of data collected by simple diagnostic tools to detect AoS at earlier stages will depend on the quality and robustness of such DH programs that will still need to demonstrate clinical benefit and cost-effectiveness and promote equity. In addition, the creation of awareness of VHD in the community and among physicians remains pivotal in the proper management of this health care problem in addition to research on pharmacological approaches to temper disease progression [99].
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study. Lancet. 2006;368:1005.
Eveborn GW, Schirmer H, Heggelund G, Lunde P, Rasmussen K. The evolving epidemiology of valvular aortic stenosis. the Tromso study. Heart. 2013;99:396.
Hill JA, Olson EN. Cardiac plasticity. N Engl J Med. 2008;358:1370.
Schiattarella GG, Hill JA. Inhibition of hypertrophy is a good therapeutic strategy in ventricular pressure overload. Circulation. 2015;131:1435.
Nakamura M, Sadoshima J. Mechanisms of physiological and pathological cardiac hypertrophy. Nat Rev Cardiol. 2018;15:387.
Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med. 1990;322:1561.
Meerson FZ. On the mechanism of compensatory hyperfunction and insufficiency of the heart. Cor Vasa. 1961;3:161.
Schelbert EB, Butler J, Diez J. Why clinicians should care about the cardiac interstitium. JACC Cardiovasc Imaging. 2019;12:2305.
Everett RJ, Tastet L, Clavel MA, Chin CWL, Capoulade R, Vassiliou VS, Kwiecinski J, Gomez M, van Beek EJR, White AC, Prasad SK, Larose E, Tuck C, Semple S, Newby DE, Pibarot P, Dweck MR. Progression of hypertrophy and myocardial fibrosis in aortic stenosis: a multicenter cardiac magnetic resonance study. Circ Cardiovasc Imaging. 2018;11:e007451.
Frey N, Katus HA, Olson EN, Hill JA. Hypertrophy of the heart: a new therapeutic target? Circulation. 2004;109:1580.
Baumgartner H, Iung B, Otto CM. Timing of intervention in asymptomatic patients with valvular heart disease. Eur Heart J. 2020;41:4349.
Lopaschuk GD, Ussher JR, Folmes CD, Jaswal JS, Stanley WC. Myocardial fatty acid metabolism in health and disease. Physiol Rev. 2010;90:207.
Wang ZV, Ferdous A, Hill JA. Cardiomyocyte autophagy: metabolic profit and loss. Heart Fail Rev. 2013;18:585.
Allard MF. Energy substrate metabolism in cardiac hypertrophy. Curr Hypertens Rep. 2004;6:430.
Sambandam N, Lopaschuk GD, Brownsey RW, Allard MF. Energy metabolism in the hypertrophied heart. Heart Fail Rev. 2002;7:161.
Guyton AC. Determination of cardiac output by equating venous return curves with cardiac response curves. Physiol Rev. 1955;35:123.
Starling EH, Visscher MB. The regulation of the energy output of the heart. J Physiol. 1927;62:243.
Gonzales H, Douglas PS, Pibarot P, Hahn RT, Khalique OK, Jaber WA, Cremer P, Weissman NJ, Asch FM, Zhang Y, Gertz ZM, Elmariah S, Clavel MA, Thourani VH, Daubert M, Alu MC, Leon MB, Lindman BR. Left ventricular hypertrophy and clinical outcomes over 5 years after TAVR: an analysis of the PARTNER trials and registries. JACC Cardiovasc Interv. 2020;13:1329.
Hill JA, Karimi M, Kutschke W, Davisson RL, Zimmerman K, Wang Z, Kerber RE, Weiss RM. Cardiac hypertrophy is not a required compensatory response to short-term pressure overload. Circulation. 2000;101:2863.
Vega RB, Konhilas JP, Kelly DP, Leinwand LA. Molecular mechanisms underlying cardiac adaptation to exercise. Cell Metab. 2017;25:1012.
Fulton N, Rajiah P. Utility of magnetic resonance imaging in the evaluation of left ventricular thickening. Insights Imaging. 2017;8:279.
Salcedo EE, Korzick DH, Currie PJ, Stewart WJ, Lever HM, Goormastic M. Determinants of left ventricular hypertrophy in patients with aortic stenosis. Cleve Clin J Med. 1989;56:590.
Carroll JD, Carroll EP, Feldman T, Ward DM, Lang RM, McGaughey D, Karp RB. Sex-associated differences in left ventricular function in aortic stenosis of the elderly. Circulation. 1992;86:1099.
Lavie CJ, Milani RV, Patel D, Artham SM, Ventura HO. Disparate effects of obesity and left ventricular geometry on mortality in 8088 elderly patients with preserved systolic function. Postgrad Med. 2009;121:119.
Lindman BR, Arnold SV, Madrazo JA, Zajarias A, Johnson SN, Perez JE, Mann DL. The adverse impact of diabetes mellitus on left ventricular remodeling and function in patients with severe aortic stenosis. Circ Heart Fail. 2011;4:286.
Dweck MR, Boon NA, Newby DE. Calcific aortic stenosis: a disease of the valve and the myocardium. J Am Coll Cardiol. 2012;60:1854.
Jang JY, Seo JS, Sun BJ, Kim DH, Song JM, Kang DH, Song JK. Impact of valvuloarterial impedance on concentric remodeling in aortic stenosis and its regression after valve replacement. J Cardiovasc Ultrasound. 2016;24:201.
Saremi F, Sanchez-Quintana D, Mori S, Muresian H, Spicer DE, Hassani C, Anderson RH. Fibrous skeleton of the heart: anatomic overview and evaluation of pathologic conditions with CT and MR imaging. Radiographics. 2017;37:1330.
Goldsmith EC, Bradshaw AD, Zile MR, Spinale FG. Myocardial fibroblast-matrix interactions and potential therapeutic targets. J Mol Cell Cardiol. 2014;70:92.
Quan TE, Cowper S, Wu SP, Bockenstedt LK, Bucala R. Circulating fibrocytes: collagen-secreting cells of the peripheral blood. Int J Biochem Cell Biol. 2004;36:598.
Haudek SB, Xia Y, Huebener P, Lee JM, Carlson S, Crawford JR, Pilling D, Gomer RH, Trial J, Frangogiannis NG, Entman ML. Bone marrow-derived fibroblast precursors mediate ischemic cardiomyopathy in mice. Proc Natl Acad Sci U S A. 2006;103:18284.
Schelbert EB, Fonarow GC, Bonow RO, Butler J, Gheorghiade M. Therapeutic targets in heart failure: refocusing on the myocardial interstitium. J Am Coll Cardiol. 2014;63:2188.
Diez J, Gonzalez A, Kovacic JC. Myocardial interstitial fibrosis in nonischemic heart disease, part 3/4: JACC Focus Seminar. J Am Coll Cardiol. 2020;75:2204.
Echegaray K, Andreu I, Lazkano A, Villanueva I, Saenz A, Elizalde MR, Echeverria T, Lopez B, Garro A, Gonzalez A, Zubillaga E, Solla I, Sanz I, Gonzalez J, Elosegui-Artola A, Roca-Cusachs P, Diez J, Ravassa S, Querejeta R. Role of myocardial collagen in severe aortic stenosis with preserved ejection fraction and symptoms of heart failure. Rev Esp Cardiol (Engl Ed). 2017;70:832.
Heymans S, Schroen B, Vermeersch P, Milting H, Gao F, Kassner A, Gillijns H, Herijgers P, Flameng W, Carmeliet P, Van de Werf F, Pinto YM, Janssens S. Increased cardiac expression of tissue inhibitor of metalloproteinase-1 and tissue inhibitor of metalloproteinase-2 is related to cardiac fibrosis and dysfunction in the chronic pressure-overloaded human heart. Circulation. 2005;112:1136.
Mewton N, Liu CY, Croisille P, Bluemke D, Lima JA. Assessment of myocardial fibrosis with cardiovascular magnetic resonance. J Am Coll Cardiol. 2011;57:891.
Weidemann F, Herrmann S, Stork S, Niemann M, Frantz S, Lange V, Beer M, Gattenlohner S, Voelker W, Ertl G, Strotmann JM. Impact of myocardial fibrosis in patients with symptomatic severe aortic stenosis. Circulation. 2009;120:577.
Azevedo CF, Nigri M, Higuchi ML, Pomerantzeff PM, Spina GS, Sampaio RO, Tarasoutchi F, Grinberg M, Rochitte CE. Prognostic significance of myocardial fibrosis quantification by histopathology and magnetic resonance imaging in patients with severe aortic valve disease. J Am Coll Cardiol. 2010;56:278.
Dweck MR, Joshi S, Murigu T, Alpendurada F, Jabbour A, Melina G, Banya W, Gulati A, Roussin I, Raza S, Prasad NA, Wage R, Quarto C, Angeloni E, Refice S, Sheppard M, Cook SA, Kilner PJ, Pennell DJ, Newby DE, Mohiaddin RH, Pepper J, Prasad SK. Midwall fibrosis is an independent predictor of mortality in patients with aortic stenosis. J Am Coll Cardiol. 2011;58:1271.
Barone-Rochette G, Pierard S, Meester De, de Ravenstein C, Seldrum S, Melchior J, Maes F, Pouleur AC, Vancraeynest D, Pasquet A, Vanoverschelde JL, Gerber BL. Prognostic significance of LGE by CMR in aortic stenosis patients undergoing valve replacement. J Am Coll Cardiol. 2014;64:144.
Hein S, Arnon E, Kostin S, Schonburg M, Elsasser A, Polyakova V, Bauer EP, Klovekorn WP, Schaper J. Progression from compensated hypertrophy to failure in the pressure-overloaded human heart: structural deterioration and compensatory mechanisms. Circulation. 2003;107:984.
Musa TA, Treibel TA, Vassiliou VS, Captur G, Singh A, Chin C, Dobson LE, Pica S, Loudon M, Malley T, Rigolli M, Foley JRJ, Bijsterveld P, Law GR, Dweck MR, Myerson SG, McCann GP, Prasad SK, Moon JC, Greenwood JP. Myocardial scar and mortality in severe aortic stenosis. Circulation. 2018;138:1935.
Everett RJ, Treibel TA, Fukui M, Lee H, Rigolli M, Singh A, Bijsterveld P, Tastet L, Musa TA, Dobson L, Chin C, Captur G, Om SY, Wiesemann S, Ferreira VM, Piechnik SK, Schulz-Menger J, Schelbert EB, Clavel MA, Newby DE, Myerson SG, Pibarot P, Lee S, Cavalcante JL, Lee SP, McCann GP, Greenwood JP, Moon JC, Dweck MR. Extracellular myocardial volume in patients with aortic stenosis. J Am Coll Cardiol. 2020;75:304.
Chin CW, Messika-Zeitoun D, Shah AS, Lefevre G, Bailleul S, Yeung EN, Koo M, Mirsadraee S, Mathieu T, Semple SI, Mills NL, Vahanian A, Newby DE, Dweck MR. A clinical risk score of myocardial fibrosis predicts adverse outcomes in aortic stenosis. Eur Heart J. 2016;37:713.
Kasner M, Westermann D, Lopez B, Gaub R, Escher F, Kuhl U, Schultheiss HP, Tschope C. Diastolic tissue Doppler indexes correlate with the degree of collagen expression and cross-linking in heart failure and normal ejection fraction. J Am Coll Cardiol. 2011;57:977.
Beaumont J, Lopez B, Ravassa S, Hermida N, San Jose G, Gallego I, Valencia F, Gomez-Doblas JJ, de Teresa E, Diez J, Gonzalez A. MicroRNA-19b is a potential biomarker of increased myocardial collagen cross-linking in patients with aortic stenosis and heart failure. Sci Rep. 2017;7:40696.
Villari B, Campbell SE, Hess OM, Mall G, Vassalli G, Weber KT, Krayenbuehl HP. Influence of collagen network on left ventricular systolic and diastolic function in aortic valve disease. J Am Coll Cardiol. 1993;22:1477.
Ravassa S, Lopez B, Querejeta R, Echegaray K, San Jose G, Moreno MU, Beaumont FJ, Gonzalez A, Diez J. Phenotyping of myocardial fibrosis in hypertensive patients with heart failure. Influence on clinical outcome. J Hypertens. 2017;35:853.
Williams L, Howell N, Pagano D, Andreka P, Vertesaljai M, Pecor T, Frenneaux M, Granzier H. Titin isoform expression in aortic stenosis. Clin Sci (Lond). 2009;117:237.
Gotzmann M, Grabbe S, Schone D, von Frieling-Salewsky M, Dos Remedios CG, Strauch J, Bechtel M, Dietrich JW, Tannapfel A, Mugge A, Linke WA. Alterations in titin properties and myocardial fibrosis correlate with clinical phenotypes in hemodynamic subgroups of severe aortic stenosis. JACC Basic Transl Sci. 2018;3:335.
Karamitsos TD, Arvanitaki A, Karvounis H, Neubauer S, Ferreira VM. Myocardial tissue characterization and fibrosis by imaging. JACC Cardiovasc Imaging. 2020;13:1221.
Doris MK, Everett RJ, Shun-Shin M, Clavel MA, Dweck MR. The role of imaging in measuring disease progression and assessing novel therapies in aortic stenosis. JACC Cardiovasc Imaging. 2019;12:185.
Flett AS, Hayward MP, Ashworth MT, Hansen MS, Taylor AM, Elliott PM, McGregor C, Moon JC. Equilibrium contrast cardiovascular magnetic resonance for the measurement of diffuse myocardial fibrosis: preliminary validation in humans. Circulation. 2010;122:138.
Treibel TA, Lopez B, Gonzalez A, Menacho K, Schofield RS, Ravassa S, Fontana M, White SK, DiSalvo C, Roberts N, Ashworth MT, Diez J, Moon JC. Reappraising myocardial fibrosis in severe aortic stenosis: an invasive and non-invasive study in 133 patients. Eur Heart J. 2018;39:699.
Duca F, Kammerlander AA, Panzenbock A, Binder C, Aschauer S, Loewe C, Agis H, Kain R, Hengstenberg C, Bonderman D, Mascherbauer J. Cardiac magnetic resonance T1 mapping in cardiac amyloidosis. JACC Cardiovasc Imaging. 2018;11:1924.
Lurz JA, Luecke C, Lang D, Besler C, Rommel KP, Klingel K, Kandolf R, Adams V, Schone K, Hindricks G, Schuler G, Linke A, Thiele H, Gutberlet M, Lurz P. CMR-derived extracellular volume fraction as a marker for myocardial fibrosis: the importance of coexisting myocardial inflammation. JACC Cardiovasc Imaging. 2018;11:38.
Liu CY, Liu YC, Wu C, Armstrong A, Volpe GJ, van der Geest RJ, Liu Y, Hundley WG, Gomes AS, Liu S, Nacif M, Bluemke DA, Lima JAC. Evaluation of age-related interstitial myocardial fibrosis with cardiac magnetic resonance contrast-enhanced T1 mapping: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol. 2013;62:1280.
Khalique Z, Ferreira PF, Scott AD, Nielles-Vallespin S, Wage R, Firmin DN, Pennell DJ. Diffusion tensor cardiovascular magnetic resonance of microstructural recovery in dilated cardiomyopathy. JACC Cardiovasc Imaging. 2018;11:1548.
Tamarappoo B, Han D, Tyler J, Chakravarty T, Otaki Y, Miller R, Eisenberg E, Singh S, Shiota T, Siegel R, Stegic J, Salseth T, Cheng W, Dey D, Thomson L, Berman D, Friedman J, Makkar R. Prognostic value of computed tomography-derived extracellular volume in TAVR patients with low-flow low-gradient aortic stenosis. JACC Cardiovasc Imaging. 2020;13:2591.
Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, Capodanno D, Conradi L, De Bonis M, De Paulis R, Delgado V, Freemantle N, Gilard M, Haugaa KH, Jeppsson A, Juni P, Pierard L, Prendergast BD, Sadaba JR, Tribouilloy C, Wojakowski W, Group EESD. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2021.
Halliday BP, Senior R, Pennell DJ. Assessing left ventricular systolic function: from ejection fraction to strain analysis. Eur Heart J. 2020.
Mor-Avi V, Lang RM, Badano LP, Belohlavek M, Cardim NM, Derumeaux G, Galderisi M, Marwick T, Nagueh SF, Sengupta PP, Sicari R, Smiseth OA, Smulevitz B, Takeuchi M, Thomas JD, Vannan M, Voigt JU, Zamorano JL. Current and evolving echocardiographic techniques for the quantitative evaluation of cardiac mechanics: ASE/EAE consensus statement on methodology and indications endorsed by the Japanese Society of Echocardiography. J Am Soc Echocardiogr. 2011;24:277.
Voigt JU, Cvijic M. 2- and 3-dimensional myocardial strain in cardiac health and disease. JACC Cardiovasc Imaging. 2019;12:1849.
Dahl JS, Magne J, Pellikka PA, Donal E, Marwick TH. Assessment of subclinical left ventricular dysfunction in aortic stenosis. JACC Cardiovasc Imaging. 2019;12:163.
Ng AC, Delgado V, Bertini M, Antoni ML, van Bommel RJ, van Rijnsoever EP, van der Kley F, Ewe SH, Witkowski T, Auger D, Nucifora G, Schuijf JD, Poldermans D, Leung DY, Schalij MJ, Bax JJ. Alterations in multidirectional myocardial functions in patients with aortic stenosis and preserved ejection fraction: a two-dimensional speckle tracking analysis. Eur Heart J. 2011;32:1542.
Magne J, Cosyns B, Popescu BA, Carstensen HG, Dahl J, Desai MY, Kearney L, Lancellotti P, Marwick TH, Sato K, Takeuchi M, Zito C, Casalta AC, Mohty D, Pierard L, Habib G, Donal E. Distribution and prognostic significance of left ventricular global longitudinal strain in asymptomatic significant aortic stenosis: an individual participant data meta-analysis. JACC Cardiovasc Imaging. 2019;12:84.
Unlu S, Mirea O, Duchenne J, Pagourelias ED, Bezy S, Thomas JD, Badano LP, Voigt JU. Comparison of feasibility, accuracy, and reproducibility of layer-specific global longitudinal strain measurements among five different vendors: a report from the EACVI-ASE Strain Standardization Task Force. J Am Soc Echocardiogr. 2018;31:374.
Yip G, Abraham T, Belohlavek M, Khandheria BK. Clinical applications of strain rate imaging. J Am Soc Echocardiogr. 2003;16:1334.
Salles S, Espeland T, Molares A, Aase SA, Hammer TA, Stoylen A, Aakhus S, Lovstakken L, Torp H. 3D myocardial mechanical wave measurements: toward in vivo 3D myocardial elasticity mapping. JACC Cardiovasc Imaging. 2020.
Villemain O, Correia M, Mousseaux E, Baranger J, Zarka S, Podetti I, Soulat G, Damy T, Hagege A, Tanter M, Pernot M, Messas E. Myocardial stiffness evaluation using noninvasive shear wave imaging in healthy and hypertrophic cardiomyopathic adults. JACC Cardiovasc Imaging. 2019;12:1135.
Ibrahim N, Januzzi JL. The potential role of natriuretic peptides and other biomarkers in heart failure diagnosis, prognosis and management. Expert Rev Cardiovasc Ther. 2015;13:1017.
Yasue H, Yoshimura M, Sumida H, Kikuta K, Kugiyama K, Jougasaki M, Ogawa H, Okumura K, Mukoyama M, Nakao K. Localization and mechanism of secretion of B-type natriuretic peptide in comparison with those of A-type natriuretic peptide in normal subjects and patients with heart failure. Circulation. 1994;90:195.
Lancellotti P, Moonen M, Magne J, O’Connor K, Cosyns B, Attena E, Donal E, Pierard L. Prognostic effect of long-axis left ventricular dysfunction and B-type natriuretic peptide levels in asymptomatic aortic stenosis. Am J Cardiol. 2010;105:383.
Clavel MA, Malouf J, Michelena HI, Suri RM, Jaffe AS, Mahoney DW, Enriquez-Sarano M. B-type natriuretic peptide clinical activation in aortic stenosis: impact on long-term survival. J Am Coll Cardiol. 2014;63:2016.
Chin CW, Shah AS, McAllister DA, Joanna Cowell S, Alam S, Langrish JP, Strachan FE, Hunter AL, Maria Choy A, Lang CC, Walker S, Boon NA, Newby DE, Mills NL, Dweck MR. High-sensitivity troponin I concentrations are a marker of an advanced hypertrophic response and adverse outcomes in patients with aortic stenosis. Eur Heart J. 2014;35:2312.
Bing R, Everett RJ, Tuck C, Semple S, Lewis S, Harkess R, Mills NL, Treibel TA, Prasad S, Greenwood JP, McCann GP, Newby DE, Dweck MR. Rationale and design of the randomized, controlled Early Valve Replacement Guided by Biomarkers of Left Ventricular Decompensation in Asymptomatic Patients with Severe Aortic Stenosis (EVOLVED) trial. Am Heart J. 2019;212:91.
Imran TF, Shin HJ, Mathenge N, Wang F, Kim B, Joseph J, Gaziano JM, Djousse L. Meta-analysis of the usefulness of plasma galectin-3 to predict the risk of mortality in patients with heart failure and in the general population. Am J Cardiol. 2017;119:57.
Krum H, Elsik M, Schneider HG, Ptaszynska A, Black M, Carson PE, Komajda M, Massie BM, McKelvie RS, McMurray JJ, Zile MR, Anand IS. Relation of peripheral collagen markers to death and hospitalization in patients with heart failure and preserved ejection fraction: results of the I-PRESERVE collagen substudy. Circ Heart Fail. 2011;4:561.
Lopez B, Querejeta R, Varo N, Gonzalez A, Larman M, Martinez Ubago JL, Diez J. Usefulness of serum carboxy-terminal propeptide of procollagen type I in assessment of the cardioreparative ability of antihypertensive treatment in hypertensive patients. Circulation. 2001;104:286.
Hara A, Niwa M, Kanayama T, Noguchi K, Niwa A, Matsuo M, Kuroda T, Hatano Y, Okada H, Tomita H. Galectin-3: a potential prognostic and diagnostic marker for heart disease and detection of early stage pathology. Biomolecules. 2020;10.
Whitelaw S, Pellegrini DM, Mamas MA, Cowie M, Van Spall HGC. Barriers and facilitators of the uptake of digital health technology in cardiovascular care: a systematic scoping review. Eur Heart J Digit Health. 2021;2:62.
Asteggiano R CM, Richter D, Christodorescu R, Guasti L, Ferrini M. Survey on e-health knowledge and usage in general cardiology of the Council of Cardiology Practice and the Digital Health Committee European Heart Journal - Digital Health 2021;342.
V. D. AI — the people and places that make, use and manage it. Nature. 2021;499.
de Jaegere PPT LJ, Bruining N. The 12-lead surface electrocardiogram: a sheet of paper or a realm of concealed information asking for Deep Learning analysis. Eur Heart J Digit Health 2021;356.
Attia ZI, Harmon DM, Behr ER, Friedman PA. Application of artificial intelligence to the electrocardiogram. Eur Heart J. 2021;42:4717.
Siontis KC, Noseworthy PA, Attia ZI, Friedman PA. Artificial intelligence-enhanced electrocardiography in cardiovascular disease management. Nat Rev Cardiol. 2021;18:465.
Reichlin T, Abacherli R, Twerenbold R, Kuhne M, Schaer B, Muller C, Sticherling C, Osswald S. Advanced ECG in 2016: is there more than just a tracing? Swiss Med Wkly. 2016;146:w14303.
Kwon JM, Jo YY, Lee SY, Kim KH. Artificial intelligence using electrocardiography: strengths and pitfalls. Eur Heart J. 2021;42:2896.
Kwon JM, Lee SY, Jeon KH, Lee Y, Kim KH, Park J, Oh BH, Lee MM. Deep learning-based algorithm for detecting aortic stenosis using electrocardiography. J Am Heart Assoc. 2020;9:e014717.
Cohen-Shelly M, Attia ZI, Friedman PA, Ito S, Essayagh BA, Ko WY, Murphree DH, Michelena HI, Enriquez-Sarano M, Carter RE, Johnson PW, Noseworthy PA, Lopez-Jimenez F, Oh JK. Electrocardiogram screening for aortic valve stenosis using artificial intelligence. Eur Heart J. 2021;42:2885.
Schlessinger DE DN, Raghu A, Reinertsten E, Young K, Batra P,Pomerantsev E, Stultz EM. A deep learning model for inferring elevated pulmonary capillary wedge pressures from the 12-lead electrocardiogram. 2022.
Gladding PA, Hewitt W, Schlegel TT. Going deep with ECG and aortic stenosis: touchdown or incomplete pass? J Am Heart Assoc. 2020;9:e016193.
Lee SH, Kim YS, Yeo WH. Advances in microsensors and wearable bioelectronics for digital stethoscopes in health monitoring and disease diagnosis. Adv Healthc Mater. 2021;10:e2101400.
Chorba JS, Shapiro AM, Le L, Maidens J, Prince J, Pham S, Kanzawa MM, Barbosa DN, Currie C, Brooks C, White BE, Huskin A, Paek J, Geocaris J, Elnathan D, Ronquillo R, Kim R, Alam ZH, Mahadevan VS, Fuller SG, Stalker GW, Bravo SA, Jean D, Lee JJ, Gjergjindreaj M, Mihos CG, Forman ST, Venkatraman S, McCarthy PM, Thomas JD. Deep learning algorithm for automated cardiac murmur detection via a digital stethoscope platform. J Am Heart Assoc. 2021;10:e019905.
Kwak S, Lee Y, Ko T, Yang S, Hwang IC, Park JB, Yoon YE, Kim HL, Kim HK, Kim YJ, Cho GY, Sohn DW, Won S, Lee SP. Unsupervised cluster analysis of patients with aortic stenosis reveals distinct population with different phenotypes and outcomes. Circ Cardiovasc Imaging. 2020;13:e009707.
Lachmann M, Rippen E, Schuster T, Xhepa E, von Scheidt M, Pellegrini C, Trenkwalder T, Rheude T, Stundl A, Thalmann R, Harmsen G, Yuasa S, Schunkert H, Kastrati A, Laugwitz KL, Kupatt C, Joner M. Subphenotyping of patients with aortic stenosis by unsupervised agglomerative clustering of echocardiographic and hemodynamic data. JACC Cardiovasc Interv. 2021;14:2127.
Casaclang-Verzosa G, Shrestha S, Khalil MJ, Cho JS, Tokodi M, Balla S, Alkhouli M, Badhwar V, Narula J, Miller JD, Sengupta PP. Network tomography for understanding phenotypic presentations in aortic stenosis. JACC Cardiovasc Imaging. 2019;12:236.
Genereux P, Pibarot P, Redfors B, Mack MJ, Makkar RR, Jaber WA, Svensson LG, Kapadia S, Tuzcu EM, Thourani VH, Babaliaros V, Herrmann HC, Szeto WY, Cohen DJ, Lindman BR, McAndrew T, Alu MC, Douglas PS, Hahn RT, Kodali SK, Smith CR, Miller DC, Webb JG, Leon MB. Staging classification of aortic stenosis based on the extent of cardiac damage. Eur Heart J. 2017;38:3351.
Kraler S, Blaser MC, Aikawa E, Camici GG, Luscher TF. Calcific aortic valve disease: from molecular and cellular mechanisms to medical therapy. Eur Heart J. 2022;43:683.
Author information
Authors and Affiliations
Contributions
All authors met the following three criteria: (1) substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content; and (3) final approval of the version to be published.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
All authors consented for publication of the manuscript.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nuis, RJ., Ribeiro, J.M., Lopez-Jimenez, F. et al. Treatment Decision in Aortic Stenosis—Look at the Valve but Do Not Forget the Ventricle. SN Compr. Clin. Med. 5, 101 (2023). https://doi.org/10.1007/s42399-023-01438-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-023-01438-8