Abstract
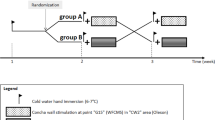
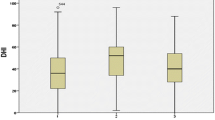
Arterial pressure (AP) and heart rate (HR) have not been continuously measured from the beginning of the caloric test. This study aimed to evaluate (1) the changes in AP and HR continuously during the test, and (2) the relationship between those changes and semicircular canal function. Airflow at 15 °C was applied to the left ear (Ear15) and the left tragus (Tragus15), and also airflow at 37 °C was applied to the left ear (Ear37) for 1 min per condition in healthy subjects. AP and HR were recorded and analyzed in time series. Additionally, cold airflow was applied to the right and left ears for 1 min in outpatient subjects experiencing vestibular dysfunction, and maximum changes in AP, HR, and slow phase velocity (SPV) of nystagmus were measured. HR immediately decreased during the Ear15 at the onset of the airflow, regardless AP change. Thus, the decrease in HR was not related to AP control. Neither AP nor HR changed during the Ear37 and Tragus15 stimulation. Thus, the decreases in HR were not induced by mechanical stimulation. The SPV significantly and positively correlated with changes in HR in outpatient subjects. Thus, patients with lower semicircular function showed a larger decrease in HR. Cold airflow applied to the ears immediately decreased HR, and the semicircular canals might be correcting the change.








Similar content being viewed by others
Data Availability
The datasets used and/or analyzed in the current study are available from the corresponding author on reasonable request.
Code Availability
Not applicable.
References
Hall JE. Cortical and brain stem control of motor function. In: Hall JE, editor. Textbook of medical physiology. Plhiladelphia: Elsevier; 2015. p. 707–19.
Yates BJ, Miller AD. Properties of sympathetic reflexes elicited by natural vestibular stimulation: implications for cardiovascular control. J Neurophysiol. 1994;71:2087–92.
Gotoh TM, Fujiki N, Matsuda T, Gao S, Morita H. Roles of baroreflex and vestibulosympathetic reflex in controlling arterial blood pressure during gravitational stress in conscious rats. Am J Physiol Regul Integr Comp Physiol. 2004;286:R25-30.
Tanaka K, Abe C, Awazu C, Morita H. Vestibular system plays a significant role in arterial pressure control during head-up tilt in young subjects. Auton Neurosci: Basic Clin. 2009;148:90–6. https://doi.org/10.1016/j.autneu.2009.03.007.
Tanaka K, Gotoh TM, Awazu C, Morita H. Roles of the vestibular system in controlling arterial pressure in conscious rats during a short period of microgravity. Neurosci Lett. 2006;397:40–3. https://doi.org/10.1016/j.neulet.2005.11.052.
Gentine A, Eichhorn JL, Kopp C, Conraux C. Modelling the action of caloric stimulation of vestibule. III. Caloric nystagmus induced by osmotic pressure variation. Acta otolaryngol. 1991;111:463–7.
Eviatar A. Severe bradycardia induced by caloric test in cardiac patients. Ann Otol Rhinol Laryngol. 1970;79:680–4. https://doi.org/10.1177/000348947007900332.
Costa F, Lavin P, Robertson D, Biaggioni I. Effect of neurovestibular stimulation on autonomic regulation. Clin Auton Res: Off J Clin Auton Res Soc. 1995;5:289–93.
Jauregui-Renaud K, Yarrow K, Oliver R, Gresty MA, Bronstein AM. Effects of caloric stimulation on respiratory frequency and heart rate and blood pressure variability. Brain Res Bull. 2000;53:17–23.
Ray CA, Hume KM, Steele SL. Sympathetic nerve activity during natural stimulation of horizontal semicircular canals in humans. Am J Physiol. 1998;275:R1274–8.
Wang J, Lewis RF. Contribution of intravestibular sensory conflict to motion sickness and dizziness in migraine disorders. J Neurophysiol. 2016;116:1586–91. https://doi.org/10.1152/jn.00345.2016.
Wang JQ, Qi RR, Pan LL, Zhou W, Zhang LL, Cai YL. Motion sickness and resting energy expenditure in Chinese male adults. Aerosp Med Hum Perform. 2016;87:360–6. https://doi.org/10.3357/AMHP.4438.2016.
Chen MM, Xu LH, Chang L, Yin P, Jiang ZL. Reduction of motion sickness through targeting histamine N-methyltransferase in the dorsal vagal complex of the brain. J Pharmacol Exp Ther. 2018;364:367–76. https://doi.org/10.1124/jpet.117.244475.
Lacount L, Napadow V, Kuo B, Park K, Kim J, Brown E, et al. Dynamic cardiovagal response to motion sickness: a point-process heart rate variability study. Comput Cardiol. 2009;36:49–52.
Sedda A, Tonin D, Salvato G, Gandola M, Bottini G. Left caloric vestibular stimulation as a tool to reveal implicit and explicit parameters of body representation. Conscious Cogn. 2016;41:1–9. https://doi.org/10.1016/j.concog.2016.01.012.
Kellogg DL Jr. In vivo mechanisms of cutaneous vasodilation and vasoconstriction in humans during thermoregulatory challenges. J Appl Physiol. 1985;2006(100):1709–18. https://doi.org/10.1152/japplphysiol.01071.2005.
Hall JE. Cardiac output, venous return, and their regulation. In: Hall JE, editor. Textbook of medical physiology. Plhiladelphia: W.B. Saunders Company; 2010. p. 229–42.
Maheu M, Houde MS, Landry SP, Champoux F. The effects of aging on clinical vestibular evaluations. Front Neurol. 2015;6:205. https://doi.org/10.3389/fneur.2015.00205.
Ford CR, Stockwell CW. Reliabilities of air and water caloric responses. Arch Otolaryngol. 1978;104:380–2.
Zangemeister WH, Bock O. Air versus water caloric test. Clin Otolaryngol Allied Sci. 1980;5:379–87.
Kageyama Y, Hata Y, Okuno T, Fukaya T. Re-evaluation of the simple cold caloric test by use of an air caloric stimulator. Equilibrium Res. 1998;57:504–9. https://doi.org/10.1016/j.neulet.2005.11.052.
Kato M, Teranishi M, Katayama N, Sone M, Naganawa S, Nakashima T. Association between endolymphatic hydrops as revealed by magnetic resonance imaging and caloric response. Otol Neurotol. 2011;32:1480–5. https://doi.org/10.1097/MAO.0b013e318235568d.
Levy MN, Yang T, Wallick DW. Assessment of beat-by-beat control of heart rate by the autonomic nervous system: molecular biology technique are necessary, but not sufficient. J Cardiovasc Electrophysiol. 1993;4:183–93.
Kawada T, Ikeda Y, Sugimachi M, Shishido T, Kawaguchi O, Yamazaki T, et al. Bidirectional augmentation of heart rate regulation by autonomic nervous system in rabbits. Am J Physiol. 1996;271:H288–95. https://doi.org/10.1152/ajpheart.1996.271.1.H288.
Iwase M, Aoki T, Maeda M, Yokota M, Hayashi H. Relationship between beat to beat interval and left ventricular function in patients with atrial fibrillation. Int J Card Imaging. 1988;3:217–26.
Butt MF, Albusoda A, Farmer AD, Aziz Q. The anatomical basis for transcutaneous auricular vagus nerve stimulation. J Anat. 2020;236:588–611. https://doi.org/10.1111/joa.13122.
Janis JE, Hatef DA, Ducic I, Ahmad J, Wong C, Hoxworth RE, et al. Anatomy of the auriculotemporal nerve: variations in its relationship to the superficial temporal artery and implications for the treatment of migraine headaches. Plast Reconstr Surg. 2010;125:1422–8. https://doi.org/10.1097/PRS.0b013e3181d4fb05.
Badran BW, Mithoefer OJ, Summer CE, LaBate NT, Glusman CE, Badran AW, et al. Short trains of transcutaneous auricular vagus nerve stimulation (taVNS) have parameter-specific effects on heart rate. Brain Stimul. 2018;11:699–708. https://doi.org/10.1016/j.brs.2018.04.004.
Andreas M, Arzl P, Mitterbauer A, Ballarini NM, Kainz FM, Kocher A, et al. Electrical stimulation of the greater auricular nerve to reduce postoperative atrial fibrillation. Circ Arrhythm Electrophysiol. 2019;12:e007711. https://doi.org/10.1161/CIRCEP.119.007711.
Stavrakis S, Stoner JA, Humphrey MB, Morris L, Filiberti A, Reynolds JC, et al. TREAT AF (transcutaneous electrical vagus nerve stimulation to suppress atrial fibrillation): a randomized clinical trial. JACC Clin Electrophysiol. 2020;6:282–91. https://doi.org/10.1016/j.jacep.2019.11.008.
Bittar RSM, Sato ES, Silva-Ribeiro DJ, Oiticica J, Mezzalira R, Tsuji RK, et al. Caloric test and video head impulse test sensitivity as vestibular impairment predictors before cochlear implant surgery. Clinics (Sao Paulo). 2019;74:e786. https://doi.org/10.6061/clinics/2019/e786.
Banchi CA, Beattie RC. Effects of stimulus duration on air caloric slow phase velocity. J Am Acad Audiol. 1991;2:246–52.
Jitsukawa S, Takano K, Ito F, Tsubomatsu C, Himi T. Influence of age on caloric response. Adv Otorhinolaryngol. 2016;77:17–22. https://doi.org/10.1159/000441864.
Rah YC, Park JH, Park JH, Choi BY, Koo JW. Dizziness and vestibular function before and after cochlear implantation. Eur Arch Otorhinolaryngol. 2016;273:3615–21. https://doi.org/10.1007/s00405-016-3988-3.
Acknowledgements
The authors thank the staff at the Osaka branch of Unique Medical for their technical assistance and encouragement. The authors thank Emma Longworth-Mills, PhD, from Edanz Group (https://en-author-services.edanz.com/ac) for editing a draft of this manuscript. The authors thank professors Minai and Sei for their statistical advice. This work was supported by JSPS KAKENHI Grant Number 18K06451.
Funding
This work was supported by JSPS KAKENHI Grant Number 18K06451.
Author information
Authors and Affiliations
Contributions
KT conceived and designed the experiments. KK, AS, SE, and MN collected the data. KT and KK interpreted the data. KT wrote the manuscript. KK and SI revised the manuscript critically. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This study was approved by the ethics committee of Gifu University of Medical Science for protocol 1 (30–7) and protocol 2 (2019–7), and Nagoya City University for protocol 2 (60–19-0100).
Consent to Participate
Written informed consent was obtained from all participants.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tanaka, K., Kabaya, K., Sugiura, A. et al. Cold Airflow Applied to the Ear Decreases Heart Rate. SN Compr. Clin. Med. 4, 131 (2022). https://doi.org/10.1007/s42399-022-01216-y
Accepted:
Published:
DOI: https://doi.org/10.1007/s42399-022-01216-y