Abstract
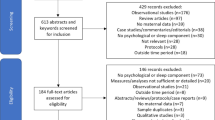
The purpose of this narrative review is to expand on a previous selective review and identify and categorize current research related to maternal postpartum sleep and the negative outcomes of sleep disturbances including its impact on maternal mental health. A literature search from 2008 to 2020 was conducted using the Cumulative Index of Allied Health Literature, Ovid MEDLINE, PsycINFO, and PubMed electronic databases in addition to reference lists from selected articles and other key references. Search terms included sleep, postpartum, sleep deprivation, sleep disturbance, hospital, mental health, postpartum depression, and anxiety. A critical review of all relevant articles from the data sources was conducted with specific focus on maternal sleep in the postpartum period. Literature was reviewed and organized into groups with similar characteristics. Although a clear link between maternal sleep and maternal mental health exists, a need remains to understand which of these occurs first as the primary problem. Other identified categories of interest included sleep quality during pregnancy, factors present in the hospital, birth method and outcomes, individual maternal characteristics, feeding method, and postpartum bonding. A lack of consistency in measurement and recommendations from the current state of research remains. Furthermore, scientifically-founded negative consequences to maternal postpartum sleep disturbances exist including impact on the mother-newborn dyad and maternal mental health. Further research is needed to determine recommendations to improve maternal postpartum sleep.
Similar content being viewed by others
Data Availability
Not applicable (narrative review)
Code Availability
Not applicable (narrative review)
References
Suplee PD, Janke J. AWHONN compendium of postpartum care. 3rd ed. Washington, DC: Association of Women’s Health, Obstetric and Neonatal Nurses; 2020.
Hunter LP, Rychnovsky JD, Yount SM. A selective review of maternal sleep characteristics in the postpartum period. J Obstet Gynecol Neonatal Nurs. 2009;38:60–8. https://doi.org/10.1111/j.1552-6909.2008.00309.x.
Pelayo R, Dement WC. History of sleep physiology and medicine. In: Kryger MH, Roth T, Dement WC, editors. Principles and practice of sleep medicine. 6th ed. Philadelphia: Elsevier Saunders; 2017.
Tempesta D, Socci V, De Gennaro L, Ferrara M. Sleep and emotional processing. Sleep Med Rev. 2018;40:183–95. https://doi.org/10.1016/j.smrv.2017.12.005.
National Sleep Foundation. How much sleep do we really need? 2020. http://www.sleepfoundation.org/article/how-sleep-works/how-much-sleep-do-we-really-need. Accessed 1 January 2021.
Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. J Clin Sleep Med. 2015. https://doi.org/10.5665/sleep.4716.
Banks S, Dinges DF. Behavioral and physiological consequences of sleep restriction. J Clin Sleep Med. 2007; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1978335/pdf/jcsm.3.5.519.pdf. Accessed 24 Jan 2021.
Hafner M, Stepanek M, Taylor J, Troxel WM, van Stolk C. Why sleep matters – the economic costs of insufficient sleep: a cross-country comparative analysis: Rand Corporation; 2017. https://www.rand.org/pubs/research_reports/RR1791.html. Accessed 24 Jan 2021
Humphries JD. Sleep disruption in hospitalized adults. Medsurg Nurs. 2008;17:391–5.
Benca RM, Quintas J. Sleep and host defenses: a review. Sleep. 1997. https://doi.org/10.1093/sleep/20.11.1027.
Johns Hopkins Medicine. The effects of sleep deprivation. Johns Hopkins Medicine. 2020; https://www.hopkinsmedicine.org/health/wellness-and-prevention/the-effects-of-sleep-deprivation. Accessed 24 Jan 2021.
Okun M. Sleep disturbances and modulations in inflammation: implications for pregnancy health. Soc Personal Psychol Compass. 2019;13:e12451. https://doi.org/10.1111/spc3.12451.
Richardson P. Sleep in pregnancy. In: Holistic Nursing Practice. 1996. http://journals.lww.com/hnpjournal. Accessed 15 October 2020
Adam K. Sleep as a restorative process and a theory to explain why. Prog Brain Res. 1980. https://doi.org/10.1016/S0079-6123(08)60070-9.
Adam K, Oswald I. Sleep is for tissue restoration. J Roy Coll Phycns. 1977; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5368747/pdf/jrcollphyslond90297-0074.pdf. Accessed 22 Jan 2021.
Facco FL, Kramer J, Ho KH, Zee PC, Grobman WA. Sleep disturbances in pregnancy. Obstet Gynecol. 2010;115:77–83. https://doi.org/10.1097/AOG.0b013e3181c4f8ec.
National Sleep Foundation. Pregnancy and sleep. 2011. http://www.sleepfoundation.org/article/sleep-topics/pregnancy-and-sleep. Accessed 10 November 2020.
Christian LM, Carroll JE, Porter K, Hall MH. Sleep quality across pregnancy and postpartum: effects of parity and race. Sleep Health. 2019;5:327–34. https://doi.org/10.1016/j.sleh.2019.03.005.
Auckley D. Poor sleep in the hospital: contributing factors and interventions. UpToDate. 2020. https://www.uptodate.com/contents/poor-sleep-in-thehospital-contributing-factors-and-interventions#H877505830. Accessed 2 Dec 2020.
Delaney LJ, Currie MJ, Huang HCC, Lopez V, Van Haren F. “They can rest at home”: an observational study of patients’ quality of sleep in an Australian hospital. BMC Health Serv Res. 2018. https://doi.org/10.1186/s12913-018-3201-z.
Adati S, Law S, Haggerty J. Room for improvement: noise on a maternity ward. BMC Health Serv Res. 2014; http://www.biomedcentral.com/1472-6963/14/604. Accessed 22 Jan 2021.
Berglund B, Lindvall T, Schwela DH. Guidelines for community noise. World Health Organization. 1995; https://www.nh.gov/osi/energy/programs/documents/sb99-who-guidelines-community-noise.pdf. Accessed 24 Jan 2021.
Morrison B, Ludington-Hoe S, Anderson GC. Interruptions to breastfeeding dyads on postpartum day 1 in a university hospital. J Obstet Gynecol Neonatal Nurs. 2006;35:709–16. https://doi.org/10.1111/j.1552-6909.2006.00095.x.
Dennis CL, Ross L. Relationships among infant sleep patterns, maternal fatigue, and development of depressive symptomology. Birth. 2005;32:187–93. https://doi.org/10.1111/j.0730-7659.2005.00368.x.
Doan T, Gardiner A, Gay CL, Lee KA. Breastfeeding increases sleep duration of new parents. J Perinat Neonatal Nurs. 2007;21:200–6. https://doi.org/10.1097/01.JPN.0000285809.36398.1b.
Horiuhi S, Nishihara K. Analyses of mothers’ sleep logs in postpartum periods. Psychiatry Clin Neurosci. 1999;53:137–9. https://doi.org/10.1046/j.1440-1819.1999.00519.x.
Shinkoda H, Matsumoto K, Park YM. Changes in sleep-wake cycle during the period from late pregnancy to puerperium identified from the wrist actigraph and sleep logs. Psychiatry Clin Neurosci. 1999;53:133–5. https://doi.org/10.1046/j.1440-1819.1999.00518.x.
Thomas KA, Foreman SW. Infant sleep and feeding pattern: effects on maternal sleep. J Midwifery Women’s Health. 2005;50:399–404. https://doi.org/10.1016/j.jmwh.2005.04.010.
Gay CL, Lee KA, Yee SY. Sleep patterns and fatigue in new mothers and fathers. Biol Res Nurs. 2004;5:311–8. https://doi.org/10.1177/1099800403262142.
Goyal D, Gay CL, Lee KA. Patterns of sleep disruption and depressive symptoms in new mothers. J Perinat Neonatal Nurs. 2007. https://doi.org/10.1097/01.JPN.0000270629.58746.96.
Karacan I, Williams RL, Hursch CJ, McCaulley M, Heine MW. Some implications of the sleep patterns of pregnancy for postpartum emotional disturbances. Br J Psychiatry. 1969;115:929–35. https://doi.org/10.1192/bjp.115.525.929.
Kennedy HP, Gardiner A, Gay C, Lee KA. Negotiating sleep: a qualitative study of new mothers. J Perinat Neonatal Nurs. 2007;21:114–22. https://doi.org/10.1097/01.JPN.0000270628.51122.1d.
Lee KA, Zaffke ME, McEnany G. Parity and sleep patterns during and after pregnancy. Obstet Gynecol. 2000;95:14–8. https://doi.org/10.1016/S0029-7844(99)00486-X.
Matsumoto K, Shinkoda H, Kang MJ, Seo YJ. Longitudinal study of mothers’ sleep-wake behaviors and circadian time patterns from late pregnancy to postpartum – monitoring of wrist actigraphy and sleep logs. Biol Rhythm Res. 2003;34:265–78. https://doi.org/10.1076/brhm.34.3.265.18812.
Signal TL, Gander PH, Sangalli MR, Travier N, Firestone RT, Tuohy JF. Sleep duration and quality in healthy nulliparous and multiparous women across pregnancy and postpartum. Australian N Z J Obstetr Gynaecol. 2007;47:16–22. https://doi.org/10.1111/j.1479-828X.2006.00672.x.
Swain AM, O’Hara MW, Starr KR, Gorman LL. A prospective study of sleep, mood, and cognitive function in postpartum and nonpostpartum women. Obstet Gynecol. 1997;90:381–6. https://doi.org/10.1016/s0029-7844(97)89252-6.
Chin EG, Vincent C, Wilkie D. A comprehensive description of postpartum pain after cesarean delivery. J Obstet Gynecol Neonatal Nurs. 2014;43:729–41. https://doi.org/10.1111/1552-6909.12483.
Gilsenan I. Nursing interventions to alleviate insomnia. Nurs Older People. 2012;24:14–8. https://doi.org/10.7748/nop2012.05.24.4.14.c9068.
Valizadeh L, Avazeh M, Hosseini MB, Jafarabad MA. Comparison of clustered care with three and four procedures on physiological responses of preterm infants: randomized crossover clinical trial. J Caring Sci. 2014. https://doi.org/10.5681/jcs.2014.001.
Benahmed N, San Miguel L, Devos C, Fairon N, Christiaens W. Vaginal delivery: how does early hospital discharge affect mother and child outcomes? A systematic literature review. BMC Pregnancy and Childbirth. 2017;17:289. https://doi.org/10.1186/s12884-017-1465-7.
Tsuchiya M, Mori E, Iwata H, Sakajo A, Maehara K, Ozawa H, et al. Fragmented sleep and fatigue during postpartum hospitalization in older primiparous women. Nurs Health Sci. 2015;17:71–6. https://doi.org/10.1111/nhs.12157.
Lee S, Lee KA. Early postpartum sleep and fatigue for mothers after cesarean delivery compared with vaginal delivery: an exploratory study. J Perinat Neonatal Nurs. 2007;21:109–13. https://doi.org/10.1097/01.JPN.0000270627.73993.b0.
Blomqvist YT, Nyqvist KH, Rubertsson C, Funkquist E. Parents need support to find ways to optimize their own sleep without seeing their preterm infant’s sleeping patterns as a problem. Acta Paediatr. 2017;106:223–8. https://doi.org/10.1111/apa.13660.
Doering JJ, Szabo A, Goyal D, Babler E. Sleep quality and quantity in low-income postpartum women. MCN Am J Matern Child Nurs. 2017;42:166–72. https://doi.org/10.1097/NMC.0000000000000323.
Mori E, Tsuchiya M, Maehara K, Iwata H, Sakajo A, Tamakoshi K. Fatigue, depression, maternal confidence, and maternal satisfaction during the first month postpartum: a comparison of Japanese mothers by age and parity. Int J Nurs Pract. 2017;23. https://doi.org/10.1111/ijn.12508.
Mersky JP, Lee CP, Gilbert RM, Goyal D. Prevalence and correlates of maternal and infant sleep problems in a low-income US sample. Matern Child Health J. 2019;24:196–203. https://doi.org/10.1007/s10995-019-02852-y.
Rudzik AEF, Ball HL. Exploring maternal perceptions of infant sleep and feeding method among mothers in the United Kingdom: a qualitative focus group study. Matern Child Health J. 2016;20:33–40. https://doi.org/10.1007/s10995-015-1798-7.
Hughes O, Mohamad MM, Doyle P, Burke G. The significance of breastfeeding on sleep patterns during the first 48 hours postpartum for first time mothers. J Obstet Gynaecol. 2018;38:316–20. https://doi.org/10.1080/01443615.2017.1353594.
Maehara K, Mori E, Iwata H, Sakajo A, Aoki K, Morita A. Postpartum maternal function and parenting stress: comparison by feeding methods. Int J Nurs Pract. 2017;23. https://doi.org/10.1111/ijn.12549.
Doan T, Gay CL, Kennedy HP, Newman J, Lee KA. Nighttime breastfeeding behavior is associated with more nocturnal sleep among first-time mothers at one month postpartum. J Clin Sleep Med. 2014;10:313–9. https://doi.org/10.5664/jcsm.3538.
Leema SR, Mittal S, Shobha, Jindal VL, Kumar A, Lalit. Psychological assessment of primiparous women during the ante and postnatal period a longitudinal study of 3 years. Indian J Public Health Res Dev. 2013;4:170–5.
Silverman ME, Reichenberg A, Savitz DA, Cnattingius S, Lichtenstein P, Hultman DA, et al. The risk factors for postpartum depression: a population-based study. Depress Anxiety. 2017;34:178–87. https://doi.org/10.1002/da.22597.
Swanson LM, Hamilton L, Muzik M. The role of childhood trauma and PTSD on postpartum sleep disturbance. J Trauma Stress. 2014;27:689–94. https://doi.org/10.1002/jts.21965.
Parfitt Y, Ayers S. Transition to parenthood and mental health in first-time parents. Infant Ment Health J. 2014;35:263–73. https://doi.org/10.1002/imhj.21443.
Bhati S, Richards K. A systematic review of the relationships between postpartum disturbance and postpartum depression. J Obstet Gynecol Neonatal Nurs. 2015;44:350–7. https://doi.org/10.1111/1552-6909.12562.
McEvoy KM, Rayapati D, Cole KOW, Erdly C, Payne JL, Osborne LM. Poor postpartum sleep quality predicts subsequent postpartum depressive symptoms in a high-risk sample. J Clin Sleep Med. 2019;15:1303–10. https://doi.org/10.5664/jcsm.7924.
Park EM, Metlzer-Brody S, Stickgold R. Poor sleep maintenance and subjective sleep quality are associated with postpartum maternal depression symptom severity. Arch Women’s Ment Health. 2013;16:539–47. https://doi.org/10.1007/s00737-013-0356-9.
Lewis BA, Gjerdingen D, Schuver K, Avery M, Marcus BH. The effect of sleep pattern changes on postpartum depressive symptoms. BMC Womens Health. 2018;18:12. https://doi.org/10.1186/s12905-017-0496-6.
Okun ML, Mancuso RA, Hobel CJ, Schetter CD, Coussons-Read M. Poor sleep quality increases symptoms of depression and anxiety in postpartum women. J Behav Med. 2018. https://doi.org/10.1007/s10865-018-9950-7.
Saxbe DE, Schetter CD, Guardino CM, Ramey SL, Shalowitz ME, Thorp J, et al. Sleep quality predicts persistence of parental postpartum depressive symptoms and transmission of depressive symptoms from mothers to fathers. Ann Behav Med. 2016;50:862–75. https://doi.org/10.1007/s12160-016-9815-7.
Dorheim SK, Bjorvatn B, Eberhard-Gran M. Can insomnia in pregnancy predict postpartum depression? A longitudinal, population-based study. PLoS ONE. 2014;9:e94674. https://doi.org/10.1371/journal.pone.0094674.
Sedov ID, Cameron EE, Madigan S, Tomfohr-Madsen LM. Sleep quality during pregnancy: a meta-analysis. Sleep Med Rev. 2018;38:168–76. https://doi.org/10.1016/j.smrv.2017.06.005.
Wang G, Deng Y, Jiang Y, Lin Q, Dong S, Song Y, et al. Trajectories of sleep quality from late pregnancy to 36 months postpartum and association with maternal mood disturbances: a longitudinal and prospective cohort study. SLEEP. 2018;41. https://doi.org/10.1093/sleep/zsy179.
Osnes RS, Eberhard-Gran M, Follestad T, Kallestad H, Morken G, Roaldset JO. Mid-pregnancy insomnia and its association with perinatal depressive symptoms: a prospective cohort study. Behav Sleep Med. 2020:1–18. https://doi.org/10.1080/15402002.2020.1743705.
Volkovich E, Tikotzky L, Manber R. Objective and subjective sleep during pregnancy: links with depressive and anxiety symptoms. Arch Women’s Ment Health. 2016;19:173–81. https://doi.org/10.1007/s00737-015-0554-8.
Coo S, Milgrom J, Kuppens P, Cox P, Trinder J. Exploring the association between maternal mood and self-reports of sleep during the perinatal period. J Obstet Gynecol Neonatal Nurs. 2014;43:465–77. https://doi.org/10.1111/1552-6909.12464.
Zambrano DN, Mindell JA, Reyes NR, Hart CN, Herring SJ. “It’s not all about my baby’s sleep”: a qualitative study of factors influencing low-income African American mothers’ sleep quality. Behav Sleep Med. 2016. https://doi.org/10.1080/15402002.2015.1028063.
Albanese AM, Geller PA, Steinkamp JM, Barkin JL. In their own words: a qualitative investigation of the factors influencing maternal postpartum functioning in the United States. Int J Environ Res Public Health. 2020;17. https://doi.org/10.3390/ijerph17176021.
King LS, Rangel E, Simpson N, Tikotzky L, Manber R. Mothers’ postpartum sleep disturbance is associated with the ability to sustain sensitivity toward infants. Sleep Med. 2020;65:74–83. https://doi.org/10.1016/j.sleep.2019.07.017.
Goyal D, Gay C, Lee KA. How much does low socioeconomic status increase the risk of prenatal and postpartum depressive symptoms in first time mothers? Womens Health Issues. 2010;20:96–104. https://doi.org/10.1016/j.whi.2009.11.003.
Okun ML, Tolge M, Hall M. Low socioeconomic status negatively affects sleep in pregnant women. J Obstet Gynecol Neonatal Nurs. 2014;43:160–7. https://doi.org/10.1111/1552-6909.12295.
Dias FM, Junior CSD, Franco GC, Teixeria AL, Ribeiro AM. Pregnancy is associated with psychiatric symptoms in a low-income countryside community of Brazil. Neuropsychiatr Dis Treat. 2011. https://doi.org/10.2147/NDT.S26588.
Baby-Friendly USA. (n.d.-a) About us: the baby-friendly hospital initiative. Baby-Friendly USA. 2012-2020. https://www.babyfriendlyusa.org/about/. Accessed 22 Jan 2021.
Baby-Friendly USA. (n.d.-b) 10 steps & international code. Baby-Friendly USA. 2012-2020. https://www.babyfriendlyusa.org/for-facilities/practice-guidelines/10-steps-and-international-code/. Accessed 22 Jan 2021.
Coalition for Improving Maternity Services. (n.d.) Mother-friendly childbirth initiative. ImprovingBirth. 2016; http://www.motherfriendly.org/MFCI/. Accessed 24 Jan 2021.
Lai YL, Hung CH, Stocker J, Chan TF, Liu Y. Postpartum fatigue, baby-care activities, and maternal-infant attachment of vaginal and cesarean births following rooming in. Appl Nurs Res. 2015;28:116–20. https://doi.org/10.1016/j.apnr.2014.08.002.
Burke A. Rest and sleep: NCLEX-RN. RegisteredNursing.org. 2020; https://www.registerednursing.org/nclex/rest-sleep/#applying-knowledge-clients-pathophysiology-rest-sleep-interventions. Accessed 24 Jan 2021.
Gellerstedt L, Medin J, Kumlin M, Rydell KM. Nursing care and management of patients’ sleep during hospitalization: a cross-sectional study. J Clin Nurs. 2019;28:3400–7. https://doi.org/10.1111/jocn.14915.
Mindell JA, Sadeh A, Kohyama J, How TH. Parental behaviors and sleep outcomes in infants and toddlers: a cross-cultural comparison. Sleep Med. 2010;11:393–9. https://doi.org/10.1016/j.sleep.2009.11.011.
Rogojanski J, Carney CE, Monson CM. Interpersonal factors in insomnia: a model for integrating bed partners into cognitive behavioral therapy for insomnia. Sleep Med Rev. 2013;17:55–64. https://doi.org/10.1016/j.smrv.2012.02.003.
Author information
Authors and Affiliations
Contributions
AS and LS contributed equally to the literature search, summation of the literature, and revisions of the manuscript. All the authors read and approved the final version of this revised manuscript.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable (narrative review)
Consent to Participate
Not applicable (narrative review)
Consent for Publication
Not applicable (narrative review)
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine
Rights and permissions
About this article
Cite this article
Smith, A.M., Saleh, L. A Narrative Review of Maternal Sleep Issues with a Focus on Mental Health in the Postpartum Period. SN Compr. Clin. Med. 3, 1165–1176 (2021). https://doi.org/10.1007/s42399-021-00840-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-021-00840-4