Abstract
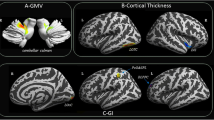
Several neuroimaging studies with advanced techniques have shown changes in gray and white matter in the brain of migraineurs. This narrative review highlights the structural and functional alterations and causality factors of migraine for the introduction of new treatment modalities. PubMed, Google Scholar, and Scopus were searched without any language restriction for the articles depicting gray and white matter changes in migraineurs. Using magnetic resonance imaging scans, multiple studies have demonstrated a reduction in white matter volume and presence of white matter hyperintensities and demyelinated white matter areas, especially in the frontal and parietal lobes. Similarly, voxel-based morphometry analysis has shown a greater reduction in gray matter in the frontal and cingulate cortex of chronic and episodic migraineurs. An overactivation of the frontal and cingulate cortex has been observed during the interictal period. These parts of gray matter are involved in cognitive, emotional, and autonomic aspects of nociception. Moreover, constituents of the limbic system, particularly the thalamus, hippocampus, amygdala, and cingulate gyrus, have also depicted predominant functional disturbances during migraine episodes. Recent studies highlighted a decrease in gray matter volume in the spinal trigeminal nucleus. These findings suggest that such changes might be the reason for dysfunction and pain regulation. Modern neuroimaging thus clearly helps in understanding the pathophysiology of migraine, which calls for novel therapeutic interventions in unresponsive or chronic migraineurs.

Similar content being viewed by others
References
Donnet A, Becker H, Allaf B, Lantéri-Minet M. Migraine and migraines of specialists: perceptions and management. Headache. 2010;50(7):1115–25. https://doi.org/10.1111/j.1526-4610.2010.01660.x.
Migraine - Symptoms and causes. Mayo Clinic. Published 2020. https://www.mayoclinic.org/diseases-conditions/migraine-headache/symptoms-causes/syc-20360201. Accessed August 23, 2020.
InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Migraine: Overview. 2012. [Updated 2018 May 30]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279373/
Burch RC, Loder S, Loder E, Smitherman TA. The prevalence and burden of migraine and severe headache in the United States: updated statistics from government health surveillance studies [published correction appears in Headache. 2015 Feb;55(2):356]. Headache. 2015;55(1):21–34. https://doi.org/10.1111/head.12482.
Lipton RB, Stewart WF, Diamond S, Diamond ML, Reed M. Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache. 2001;41(7):646–57. https://doi.org/10.1046/j.1526-4610.2001.041007646.x.
Merikangas KR. Contributions of epidemiology to our understanding of migraine. Headache. 2013;53(2):230–46. https://doi.org/10.1111/head.12038.
Wang SJ. Epidemiology of migraine and other types of headache in Asia. Curr Neurol Neurosci Rep. 2003;3(2):104–8. https://doi.org/10.1007/s11910-003-0060-7.
Jia Z, Yu S. Grey matter alterations in migraine: a systematic review and meta-analysis. Neuroimage Clin. 2017;14:130–40. Published 2017 Jan 19. https://doi.org/10.1016/j.nicl.2017.01.019.
Scher AI, Gudmundsson LS, Sigurdsson S, Ghambaryan A, Aspelund T, Eiriksdottir G, et al. Migraine headache in middle age and late-life brain infarcts. JAMA. 2009;301(24):2563–70. https://doi.org/10.1001/jama.2009.932.
Lipton RB, Pan J. Is migraine a progressive brain disease? JAMA. 2004;291(4):493–4. https://doi.org/10.1001/jama.291.4.493.
Bilgiç B, Kocaman G, Arslan AB, Noyan H, Sherifov R, Alkan A, et al. Volumetric differences suggest involvement of cerebellum and brainstem in chronic migraine. Cephalalgia. 2016;36(4):301–8. https://doi.org/10.1177/0333102415588328.
Palm-Meinders IH, Arkink EB, Koppen H, Amlal S, Terwindt GM, Launer LJ, et al. Volumetric brain changes in migraineurs from the general population. Neurology. 2017;89(20):2066–74. https://doi.org/10.1212/WNL.0000000000004640.
Xie H, Zhang Q, Huo K, et al. Association of white matter hyperintensities with migraine features and prognosis. BMC Neurol. 2018;18(1):93. Published 2018 Jul 2. https://doi.org/10.1186/s12883-018-1096-2.
Cheng CY, Cheng HM, Chen SP, Chung CP, Lin YY, Hu HH, et al. White matter hyperintensities in migraine: clinical significance and central pulsatile hemodynamic correlates. Cephalalgia. 2018;38(7):1225–36. https://doi.org/10.1177/0333102417728751.
Xie H, Bian Y, Jian Z, Huo K, Liu R, Zhu D, et al. Right-to-left shunt may be prone to affect the white matter integrity of posterior circulation in migraine without aura. Neurol Sci. 2018;39(1):119–25. https://doi.org/10.1007/s10072-017-3161-9.
Avci AY, Lakadamyali H, Arikan S, Benli US, Kilinc M. High sensitivity C-reactive protein and cerebral white matter hyperintensities on magnetic resonance imaging in migraine patients. J Headache Pain. 2015;16:9. https://doi.org/10.1186/1129-2377-16-9.
Postma IR, van Oosterhout WP, de Groot JC, Terwindt GM, Zeeman GG. The presence of brain white matter lesions in relation to preeclampsia and migraine. Cephalalgia. 2016;36(3):284–8. https://doi.org/10.1177/0333102415586065.
Zheng Z, Xiao Z, Shi X, Ding M, di W, Qi W, et al. White matter lesions in chronic migraine with medication overuse headache: a cross-sectional MRI study. J Neurol. 2014;261(4):784–90. https://doi.org/10.1007/s00415-014-7267-1.
Szabó N, Kincses ZT, Párdutz A, Tajti J, Szok D, Tuka B, et al. White matter microstructural alterations in migraine: a diffusion-weighted MRI study. Pain. 2012;153(3):651–6. https://doi.org/10.1016/j.pain.2011.11.029.
Rocca MA, Colombo B, Inglese M, Codella M, Comi G, Filippi M. A diffusion tensor magnetic resonance imaging study of brain tissue from patients with migraine. J Neurol Neurosurg Psychiatry. 2003;74(4):501–3. https://doi.org/10.1136/jnnp.74.4.501.
DaSilva AF, Granziera C, Tuch DS, Snyder J, Vincent M, Hadjikhani N. Interictal alterations of the trigeminal somatosensory pathway and periaqueductal gray matter in migraine. Neuroreport. 2007;18(4):301–5. https://doi.org/10.1097/WNR.0b013e32801776bb.
Tak AZA, Sengul Y, Bilak Ş. Evaluation of white matter hyperintensities and retinal fiber layer, ganglion cell layer, inner-plexiform layer, and choroidal layer in migraine patients. Neurol Sci. 2018;39(3):489–96. https://doi.org/10.1007/s10072-017-3234-9.
Tunç A, Güngen BD, Evliyaoğlu F, Aras YG, Tekeşin AK. Evaluation of retinal nerve fiber layer, ganglion cell layer and macular changes in patients with migraine. Acta Neurol Belg. 2017;117(1):121–9. https://doi.org/10.1007/s13760-016-0715-1.
Neeb L, Bastian K, Villringer K, Gits HC, Israel H, Reuter U, et al. No microstructural white matter alterations in chronic and episodic migraineurs: a case-control diffusion tensor magnetic resonance imaging study. Headache. 2015;55(2):241–51. https://doi.org/10.1111/head.12496.
Liu J, Lan L, Li G, Yan X, Nan J, Xiong S, et al. Migraine-related gray matter and white matter changes at a 1-year follow-up evaluation. J Pain. 2013;14(12):1703–8. https://doi.org/10.1016/j.jpain.2013.08.013.
Faragó P, Tóth E, Kocsis K, et al. Altered resting state functional activity and microstructure of the white matter in migraine with aura. Front Neurol. 2019;10:1039. Published 2019 Oct 1. https://doi.org/10.3389/fneur.2019.01039.
Jia Z, Tang W, Zhao D, Hu G, Li R, Yu S. Volumetric abnormalities of the brain in a rat model of recurrent headache. Mol Pain. 2018;14:1744806918756466. https://doi.org/10.1177/1744806918756466.
Qin Z, He XW, Zhang J, et al. Structural changes of cerebellum and brainstem in migraine without aura. J Headache Pain. 2019;20(1):93. Published 2019 Sep 2. https://doi.org/10.1186/s10194-019-1045-5.
Bashir A, Lipton RB, Ashina S, Ashina M. Migraine and structural changes in the brain: a systematic review and meta-analysis. Neurology. 2013;81(14):1260–8. https://doi.org/10.1212/WNL.0b013e3182a6cb32.
Coppola G, Petolicchio B, Di Renzo A, et al. Cerebral gray matter volume in patients with chronic migraine: correlations with clinical features. J Headache Pain. 2017;18(1):115. Published 2017 Dec 8. https://doi.org/10.1186/s10194-017-0825-z.
Rocca MA, Ceccarelli A, Falini A, Colombo B, Tortorella P, Bernasconi L, et al. Brain gray matter changes in migraine patients with T2-visible lesions: a 3-T MRI study. Stroke. 2006;37(7):1765–70. https://doi.org/10.1161/01.STR.0000226589.00599.4d.
Kim JH, Suh SI, Seol HY, Oh K, Seo WK, Yu SW, et al. Regional grey matter changes in patients with migraine: a voxel-based morphometry study. Cephalalgia. 2008;28(6):598–604. https://doi.org/10.1111/j.1468-2982.2008.01550.x.
Schmidt-Wilcke T, Gänssbauer S, Neuner T, Bogdahn U, May A. Subtle grey matter changes between migraine patients and healthy controls. Cephalalgia. 2008;28(1):1–4. https://doi.org/10.1111/j.1468-2982.2007.01428.x.
Valfrè W, Rainero I, Bergui M, Pinessi L. Voxel-based morphometry reveals gray matter abnormalities in migraine. Headache. 2008;48(1):109–17. https://doi.org/10.1111/j.1526-4610.2007.00723.x.
Jin C, Yuan K, Zhao L, Zhao L, Yu D, von Deneen KM, et al. Structural and functional abnormalities in migraine patients without aura. NMR Biomed. 2013;26(1):58–64. https://doi.org/10.1002/nbm.2819.
Celle S, Créac’h C, Boutet C, et al. Elderly patients with ongoing migraine show reduced gray matter volume in second somatosensory cortex. J Oral Facial Pain Headache. 2018;32(1):67–74. https://doi.org/10.11607/ofph.1866.
Messina R, Rocca MA, Colombo B, Pagani E, Falini A, Goadsby PJ, et al. Gray matter volume modifications in migraine: a cross-sectional and longitudinal study. Neurology. 2018;91(3):e280–92. https://doi.org/10.1212/WNL.0000000000005819.
Zhang J, Wu YL, Su J, Yao Q, Wang M, Li GF, et al. Assessment of gray and white matter structural alterations in migraineurs without aura. J Headache Pain. 2017;18(1):74. https://doi.org/10.1186/s10194-017-0783-5.
Maleki N, Becerra L, Brawn J, Bigal M, Burstein R, Borsook D. Concurrent functional and structural cortical alterations in migraine. Cephalalgia. 2012;32(8):607–20. https://doi.org/10.1177/0333102412445622.
Schmitz N, Admiraal-Behloul F, Arkink EB, Kruit MC, Schoonman GG, Ferrari MD, et al. Attack frequency and disease duration as indicators for brain damage in migraine. Headache. 2008;48(7):1044–55. https://doi.org/10.1111/j.1526-4610.2008.01133.x.
Lai TH, Chou KH, Fuh JL, Lee PL, Kung YC, Lin CP, et al. Gray matter changes related to medication overuse in patients with chronic migraine. Cephalalgia. 2016;36(14):1324–33. https://doi.org/10.1177/0333102416630593.
Schmidt-Wilcke T, Leinisch E, Gänssbauer S, et al. Affective components and intensity of pain correlate with structural differences in gray matter in chronic back pain patients. Pain. 2006;125(1–2):89–97. https://doi.org/10.1016/j.pain.2006.05.004.
Draganski B, Moser T, Lummel N, Gänssbauer S, Bogdahn U, Haas F, et al. Decrease of thalamic gray matter following limb amputation. Neuroimage. 2006;31(3):951–7. https://doi.org/10.1016/j.neuroimage.2006.01.018.
Schmidt-Wilcke T, Leinisch E, Straube A, Kämpfe N, Draganski B, Diener HC, et al. Gray matter decrease in patients with chronic tension type headache. Neurology. 2005;65(9):1483–6. https://doi.org/10.1212/01.wnl.0000183067.94400.80.
Moulton EA, Becerra L, Maleki N, Pendse G, Tully S, Hargreaves R, et al. Painful heat reveals hyperexcitability of the temporal pole in interictal and ictal migraine states. Cereb Cortex. 2011;21(2):435–48. https://doi.org/10.1093/cercor/bhq109.
Stankewitz A, Aderjan D, Eippert F, May A. Trigeminal nociceptive transmission in migraineurs predicts migraine attacks. J Neurosci. 2011;31(6):1937–43. https://doi.org/10.1523/JNEUROSCI.4496-10.2011.
Russo A, Tessitore A, Esposito F, Marcuccio L, Giordano A, Conforti R, et al. Pain processing in patients with migraine: an event-related fMRI study during trigeminal nociceptive stimulation. J Neurol. 2012;259(9):1903–12. https://doi.org/10.1007/s00415-012-6438-1.
Meylakh N, Marciszewski KK, Di Pietro F, Macefield VG, Macey PM, Henderson LA. Deep in the brain: changes in subcortical function immediately preceding a migraine attack. Hum Brain Mapp. 2018;39(6):2651–63. https://doi.org/10.1002/hbm.24030.
Marciszewski KK, Meylakh N, Di Pietro F, et al. Changes in brainstem pain modulation circuitry function over the migraine cycle. J Neurosci. 2018;38(49):10479–88. https://doi.org/10.1523/JNEUROSCI.1088-18.2018.
Schwedt TJ, Chong CD, Chiang CC, Baxter L, Schlaggar BL, Dodick DW. Enhanced pain-induced activity of pain-processing regions in a case-control study of episodic migraine. Cephalalgia. 2014;34(12):947–58. https://doi.org/10.1177/0333102414526069.
Author information
Authors and Affiliations
Contributions
All authors (Hania Hasan, HH; Rafia Irfan Waheed, RIW; Taha Bin Arif, TBA; Sidra Saleem, SS; Arsalan Anwar, AA) had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Concept and design of study: HH
Acquisition of data: HH and RIW
Interpretation of data: HH, RIW, and TBA
Drafting of the manuscript: HH, RIW, and TBA
Critical revision for important intellectual content: SS and AA
All authors have approved and proof read the manuscript and gone through the tables. All authors accept that all material in the manuscript is correct to the best of their knowledge.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not require ethical approval.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Imaging
Rights and permissions
About this article
Cite this article
Hasan, H., Irfan Waheed, R., Bin Arif, T. et al. Gray and White Matter Changes in Migraineurs: a Review of Literature. SN Compr. Clin. Med. 2, 2185–2196 (2020). https://doi.org/10.1007/s42399-020-00576-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-020-00576-7