Abstract
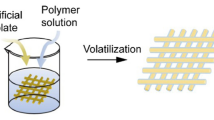
The application of three-dimensional printed polymer scaffolds in repairing bone defects is a promising strategy. Among them, polycaprolactone (PCL) scaffolds are widely studied due to their good processability and controlled degradation rate. However, as an alternative graft for repairing bone defects, PCL materials have poor hydrophilicity, which is not conducive to cell adhesion and growth. In addition, the poor mechanical properties of PCL materials cannot meet the strength required to repair bone defects. In this paper, nano-zirconium dioxide (ZrO2) powder is embedded in PCL material through a melt-mixing process, and a regular grid scaffold is constructed by 3D printing. The embedding of nanometer zirconium dioxide powder improves the hydrophilicity and water absorption of the composite scaffold, which is conducive to cell adhesion, proliferation and growth and is beneficial to the exchange of nutrients. Therefore, the PCL/ZrO2 composite scaffold showed better biological activity in vitro. At the same time, the PCL/ZrO2 composite material system significantly improves the mechanical properties of the scaffold. Among them, compared with the pure PCL scaffold, the Young’s modulus is increased by about 0.4 times, and the compressive strength is increased by about 0.5 times. In addition, the osteogenic differentiation results also showed that the PCL/ZrO2 composite scaffold group showed better ALP activity and more effective bone mineralization than the pure PCL group. We believe that the 3D printed PCL/ZrO2 composite scaffold has certain application prospects in repairing bone defects.







Similar content being viewed by others
References
Tang D, Tare RS, Yang LY et al (2016) Biofabrication of bone tissue: approaches, challenges and translation for bone regeneration. Biomaterials 83:363–382
Kang J, Yanen W, Qinghua W et al (2018) Application of 3D printing technology in bone tissue engineering. Bio-Des Manuf 1(3):203–210
Garrett B (2014) 3D printing: new economic paradigms and strategic shifts. Global Policy 5(1):70–75
He Y, Gu Z, Xie M et al (2020) Why choose 3D bioprinting? Part II: methods and bioprinters. Bio-Des Manuf 3(1):1–4
Gao Q, Niu X, Shao L et al (2019) 3D printing of complex GelMA-based scafolds with nanoclay. Biofabrication 11(3):035006
Ma L, Li Y, Wu Y et al (2020) 3D bioprintedhyaluronic acid-based cell-laden scafold forbrain microenvironment simulation. Bio-Des Manuf 3:164–174
Chia HN, Wu BM (2015) Recent advances in 3D printing of biomaterials. J Biol Eng 9(1):1–14
Xie C, Gao Q, Wang P, Shao L et al (2019) Structure-induced cell growth by 3D printing of heterogeneous scafolds with ultraine fibers. Mater Des 181:108092
Ma H, Chun F, Jiang C et al (2018) 3D-printed bioceramic scaffolds: from bone tissue engineering to tumor therapy. Acta Biomater 79:37–59
Shao L, Gao Q, Xie C et al (2020) Sacriicial microgel-laden bioink-enabled 3D bioprinting of mesoscale pore networks. Bio-Des Manuf 3:30–39
Bose S, Vahabzadeh S, Bandyopadhyay A (2013) Bone tissue engineering using 3D printing. Mater Today 16(12):496–504
Park J, Bauer S, von der Mark K et al (2007) Nanosize and vitality: TiO2 nanotube diameter directs cell fate. Nano Lett 7(6):1686–1691
Navarro M, Aparicio C, Charles-Harris M, et al (2006) Development of a biodegradable composite scaffold for bone tissue engineering: physicochemical, topographical, mechanical, degradation, and biological properties. Ordered Polym Nanostruct Surf
Bártolo Paulo, Bidanda B (2008) Bio-materials and prototyping applications in medicine. Springer, New York
Qu X, Xia P, He J et al (2016) Microscale electrohydrodynamic printing of biomimetic PCL/nHA composite scafolds for bone tissue engineering. Mater Lett 185:554–557
Huang B, Caetano G, Vyas C et al (2018) Polymer-ceramic composite scaffolds: the effect of hydroxyapatite and β-tri-calcium phosphate. Materials 11(1):129
HoJun J, Minji L, Seokhwan Y et al (2019) Fabrication and characterization of 3D-printed biocomposite scaffolds based on PCL and silanated silica particles for bone tissue regeneration. Chem Eng J 360:519–530
Khoshroo K, Jafarzadeh Kashi TS, Moztarzadeh F et al (2017) Development of 3D PCL microsphere/TiO2 nanotube composite scaffolds for bone tissue engineering. Mater Sci Eng C Mater Biol Appl 70(Pt 1):586–598
Yeo MG, Kim GH (2012) Preparation and characterization of 3D composite Scaffolds based on rapid-prototyped PCL/β-TCP struts and electrospun PCL coated with collagen and HA for bone regeneration. Chem Mater 24(5):903–913
Sousa I, Mendes A, Pereira RF et al (2014) Collagen surface modified poly(ε-caprolactone) scaffolds with improved hydrophilicity and cell adhesion properties. Mater Lett 134(1):263–267
Pang RZ, Li X, Li JS et al (2013) In situ preparation and antifouling performance of ZrO2/PVDF hybrid membrane. Acta Physico-Chim Sin 29(12):2592–2598
Li HC, Wang DG, Chen CZ (2015) Effect of zinc oxide and zirconia on structure, degradability and in vitro bioactivity of wollastonite. Ceram Int 41(8):10160–10169
Catauro Michelina R, Mariagrazia A et al (2008) Sol-gel processing of drug delivery zirconia/polycaprolactone hybrid materials. J Mater Sci Mater Med 19(2):531–540
Catauro M, Bollino F, Papale F et al (2014) Biological response of human mesenchymal stromal cells to titanium grade 4 implants coated with PCL/ZrO2 hybrid materials synthesized by sol-gel route: in vitro evaluation. Mater Sci Eng C 45:395–401
Kim GH, Yoon H (2008) Effect of an auxiliary electrode on the crystalline morphology of electrospun nanofibers. Appl Physicslett 93(2):310–312
Wang YW, Wu Q, Chen GQ (2003) Reduced mouse fibroblast cell growth by increased hydrophilicity of microbial polyhydroxyalkanoates via hyaluronan coating. Biomaterials 24(25):4621–4629
Terriza A, Vilches-Pérez J et al (2014) Osteoconductive potential of barrier nanoSiO2 PLGA membranes functionalized by plasma enhanced chemical vapour deposition. Biomed Res Int 2014:253590
Gotz HE, Muller M, Emmel A et al (2004) Effect of surface finish on the osseointegration of laser-treated titanium alloy implants. Biomaterials 25(18):4057–4064
Tsuruga E, Takita H, Itoh H et al (1997) Pore size of porous hydroxyapatite as the cell-substratum controls bmp-induced osteogenesis. J Biochem 121(2):317–324
Karageorgiou V, Kaplan D (2005) Porosity of 3D biomaterial scaffolds and osteogenesis. Biomaterials 26(27):5474–5491
Carson Thomas H, Joel Collier H, Charles Sfeir S et al (2002) Engineering gene expression and protein synthesis by modulating nuclear shape. Proc Natl Acad Sci USA 99:1972–1977
Lee KY, Alsberg E, Hsiong S et al (2004) Nanoscale adhesion ligand organization regulates osteoblast proliferation and differentiation. Nano Lett 4(8):1501–1506
Golub EE, Boesze-Battaglia K (2007) The role of alkaline phosphatase in mineralization. Curr Opin Orthop 18(5):444–448
Author information
Authors and Affiliations
Contributions
QW, ZM and YW participated in the study design, data analysis, writing and editing of the manuscript. QW, LZ and WX performed the experimental research and data analysis. All authors have read and approved the final manuscript and, therefore, have full access to all the data in the study and take responsibility for the integrity and security of the data.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study does not contain any studies with human or animal subjects performed by any of the authors.
Rights and permissions
About this article
Cite this article
Wang, Q., Ma, Z., Wang, Y. et al. Fabrication and characterization of 3D printed biocomposite scaffolds based on PCL and zirconia nanoparticles. Bio-des. Manuf. 4, 60–71 (2021). https://doi.org/10.1007/s42242-020-00095-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42242-020-00095-3