Abstract
Background
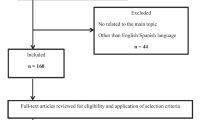
In this article, we present a case of neuroendocrine neoplasm of unknown primary origin (UPO NEN), which is a rare cause of ectopic Cushing’s syndrome (ECS) presenting numerous challenges, together with a literature review.
Case report
A 43-year-old male patient presented with clinical features consistent with Cushing’s syndrome (CS) and adrenocorticotropic hormone (ACTH)-dependent hypercortisolemia. Despite a suspicious lesion on pituitary MRI, the high-dose dexamethasone suppression test and bilateral inferior petrosal sinus sampling results were not compatible with Cushing’s disease. Bilateral non-homogeneous opacities were observed in the thorax CT of the patient, who also had a history of COVID-19 infection, but no tumoral lesion was detected. When 68Ga-SSTR PET/CT and 18FDG-PET/CT were performed, multiple metastatic foci were detected in mediastinal and hilar lymph nodes and the axial skeleton. Paratracheal-subcarinal lymph nodes were excised mediastinoscopically, and the diagnosis of NEN was made. Histopathological findings indicated that the possible origin was an atypical pulmonary carcinoid with a low Ki-67 labeling index. After controlling hypercortisolemia, a regimen of somatostatin analogs and capecitabine plus temozolomide was decided upon as treatment by a multidisciplinary council.
Conclusion
This is a challenging case of UPO NEN presenting with ECS and confounding factors, such as previous infection and incidental lesions, during the diagnosis process. The case in question highlighted the fact that atypical pulmonary carcinoid with a low proliferation index may cause visible metastases even when radiologically undetectable.
Similar content being viewed by others
Introduction
Ectopic Cushing’s syndrome (ECS) is a rare condition which can have serious consequences due to a number of hormonal and tumoral aspects. Approximately 4% of adrenocorticotropic hormone (ACTH)-dependent Cushing’s syndrome (CS) cases are composed of malignant neuroendocrine neoplasms (NENs) that secrete ectopic ACTH [1]. Although in the past the most common cause of ECS was considered to be small cell lung carcinoma, in recent years, thanks to increasing awareness, well-differentiated bronchial carcinoids have gained prominence in explaining the etiology [2]. Visible metastasis can be detected at the time of diagnosis in approximately 40–50% of all NEN cases. The primary origin cannot be determined in 13% of metastatic NEN cases [3]. Failure to determine the primary lesion in metastatic NEN patients with ACTH secretion makes the effort to control both the tumor and the symptoms associated with hypercortisolemia challenging.
In this article, we report a case of metastatic NEN of unknown primary origin, which is a rare cause of ECS and presents various difficulties in the diagnosis process and treatment decision.
Case presentation
A 43-year-old male patient presented at our clinic in November 2020 with complaints of muscle weakness in both legs, edema on the dorsum of the foot, and weight gain of 10 kg in the last 6 months. He had a 2-year history of hypertension, as well as obsessive-compulsive disorder and prediabetes for 1 year. In addition, 4 months before presentation, the patient had tested positive for coronavirus disease 2019 (COVID-19) infection in July, 2020. Physical examination revealed moon face, buffalo hump, oral candidiasis plaques, central obesity, purple striae over the abdomen, easy bruising, and bilateral pitting edema in the pretibial region and the dorsal region of the foot. There was no history of exogenous steroid use or alcohol consumption.
The patient history and physical examination findings were compatible with CS, and the overnight dexamethasone suppression test was 28.7 µg/dL (reference range < 1.8). Morning serum baseline cortisol was 27.3 µg/dL (reference range: 6.2–19.4), late-night serum cortisol was 26.0 µg/dL (reference range < 7.5), and 24-h urine free cortisol (UFC) was 773.59 µg/day (reference range: 4.2–60). Plasma ACTH levels were checked twice and were recorded as 481 and 365 pg/mL (reference range: 0–46). Serum cortisol levels were determined with CMIA (chemiluminescent microparticle immunoassay), plasma ACTH levels with ECLIA (enzyme-linked chemiluminescent immunosorbent assay), and 24-h UFC levels with LC-MS (lipid chromatography-mass spectrometry) methods. Hypercortisolemia was confirmed, and hypokalemia (K+: 3.18 mEq/L, reference range: 3.5–5.1) was also observed. Liver enzyme and kidney function tests were normal. The hormone panel showed the following: thyroid-stimulating hormone (TSH), 0.93 mIU/L (reference range: 0.27–4.2); free thyroxine (fT4), 0.72 ng/dL (reference range: 0.93–1.7); follicle-stimulating hormone (FSH), 0.86 IU/L (reference range: 1.5–12.4); luteinizing hormone (LH), < 0.3 IU/L (reference range: 1.7–8.6); and total testosterone, 55.8 ng/dL (reference range: 280–800). As an increase in TSH levels was not detected with the thyrotropin-releasing hormone (TRH) stimulation test, it was thought that the cause of hypothyroidism might be impaired TSH response to TRH secondary to hypercortisolemia (Table 1).
Magnetic resonance imaging (MRI) of the pituitary gland was performed, and a suspicious 2 mm microadenoma was observed on the right side of the pituitary gland in the sagittal planes of the T1-weighted sequence (Fig. 1). Serum cortisol and UFC levels were not suppressed after the high-dose dexamethasone suppression test (Table 1). In bilateral inferior petrosal sinus sampling (BIPSS), no gradient was detected between peripheral and central ACTH levels before and after corticotropin-releasing hormone (CRH) infusion (Table 1). In light of dynamic test results, it was speculated that the suspicious lesion in the pituitary gland might be incidental, and the main source could be an ectopic ACTH secretion. Chromogranin A level measured on high suspicion of NEN was found to be slightly elevated (237 ng/mL (reference range: 0–100)). In addition, genetic testing was not considered for multiple endocrine neoplasia type 1, since the patient had no family history, while his ionized calcium, intact parathormone, and prolactin levels were within normal limits.
A thin-slice whole-body CT was performed in order to detect the ectopic focus in November 2020. Bilateral peripheral non-homogeneous densities were detected on thorax CT (Fig. 2a, b), primarily associated with the recent COVID-19 infection, and no pathology was observed on cervical and abdominal CT. Six weeks after the first imaging, gallium-68 labeled somatostatin receptor PET/CT (68Ga-SSTR PET/CT) was performed, and increased activity uptake was observed in the paratracheal, subcarinal lymph nodes and in multiple sclerotic lesions in the axial skeleton (Fig. 3a–c). Bronchoscopy was also performed, but no tumor was detected in the trachea or bronchial lumen. 18FDG-PET/CT was also applied in order to identify the possible primary origin and to better determine the spread of the aggressive NEN. In 18FDG-PET/CT, as in 68Ga-SSTR PET/CT, increased 18FDG uptake was observed in the right paratracheal, right hilar, subcarinal lymph nodes, and axial skeleton, the largest being in the L5 vertebra (Fig. 3d–f). In addition, low-intensity 18FDG uptake was detected in the ribs, sternum, iliac bones, and both scapulae, consistent with metastatic disease.
68Ga-SSTR PET/CT scan revealed increased uptake in the paratracheal (a), subcarinal lymph nodes (b), and in diffuse sclerotic lesions of the axial skeleton (c) (yellow arrows). In the 18FDG-PET/CT scan, the highest 18FDG uptake was detected in the right paratracheal (SUVmax: 10.69) (d), right hilar and subcarinal lymph nodes (SUVmax: 9.52) (e), and L5 vertebra (black arrow) (SUVmax: 6.11) (f). SUVmax, maximum standardized uptake value
Surgical excision was performed in the right paratracheal and subcarinal lymph nodes using a mediastinoscopic approach. Pathological analyses performed with hematoxylin and eosin (H&E) staining revealed a tumor composed of monomorphic epithelial cells with round to oval nuclei with salt and pepper chromatin, inconspicuous nucleoli, and moderate to abundant eosinophilic cytoplasm forming nests and trabecular structures intermingled with sparse lymphoid cells (Fig. 4a). Immunohistochemical studies showed diffuse staining with chromogranin and TTF-1, moderate staining with synaptophysin, and sparse staining with CD56 in neoplastic cells (Fig. 4b–d). There was no staining for calcitonin, thyroglobulin, or CDX2. Extensive lymphovascular invasion and two mitoses in 2 mm2 were observed (Fig. 4e), but necrosis was not detected. The Ki-67 labeling index was low (5–8%) (Fig. 4f). Based on the microscopic and immunohistochemical findings, NEN metastasis was confirmed, and the possible origin of the tumor was presumed to be an atypical pulmonary carcinoid.
Monomorphic epithelial tumor cells forming nests and trabecular structures in the right paratracheal lymph node (H&E, × 200) (a), and immunohistochemically (IHC), diffuse chromogranin staining (IHC, × 100) (b), moderate synaptophysin staining (IHC, × 200) (c), diffuse nuclear TTF-1 staining (IHC, × 100) (d) in the tumor cells. Mitotic figure (black arrow) (H&E, × 1000) (e) and the low Ki-67 labeling index (IHC, × 400) (f) of the neuroendocrine neoplasm are also demonstrated
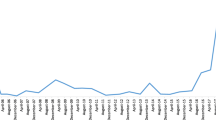
Enoxaparin for thromboprophylaxis and trimethoprim/sulfamethoxazole for prophylaxis of Pneumocystis jirovecii pneumonia were initiated immediately after hospitalization of the patient. To control hypertension and hypokalemia, in addition to ramipril 5 mg treatment, spironolactone 50 mg was given, and oral potassium replacement was administered as needed. Metyrapone was started in order to control hypercortisolemia before second-line imaging methods were used. The initial dose was 1500 mg/day; however, because of an increase in gastrointestinal complaints and the presence of adrenal insufficiency symptoms, the dose was reduced to 500 mg/day, and 20 mg/day hydrocortisone was added to the treatment. UFC levels decreased to 0.59 µg/day (reference range 4.2–60) and remained within the normal range during the 7-month follow-up (Fig. 5). After controlling the hypercortisolemia, thyroid function tests and total testosterone levels were normalized in 2 weeks. Considering that the primary origin of the metastatic disease might be a pulmonary atypical carcinoid (AC), a multidisciplinary council decided to start a regimen of temozolomide plus capecitabine (CAPTEM) with lanreotide 90 mg/month. The CAPTEM regimen consisting of temozolomide 360 mg/day for 5 days and capecitabine 4500 mg/day for 14 days each cycle was initiated, and meanwhile, the metyrapone treatment was continued. In addition to normalized serum cortisol and UFC levels after the metyrapone treatment, ACTH levels also tended to decrease after the CAPTEM regimen (Fig. 5). Ten cycles of radiotherapy and 4 mg of zoledronic acid were administered due to extensive symptomatic vertebral metastases. Although the 18FDG-PET/CT scan was repeated 9 months after the first imaging and 4 months after the initiation of the cytotoxic treatment, the primary focus was still not detected, but a significant decrease was observed in the number, size, and metabolic activity uptake of metastatic foci. Hypercortisolemia and related comorbidities were observed to be under control during this period, and there was no cytotoxic treatment-related toxicity.
Discussion
Herein, we describe a 43-year-old male patient with metastatic neuroendocrine neoplasm of unknown primary origin (UPO NEN). ECS is a challenging area of endocrine practice that may require lengthy diagnostic journeys to establish the location of the primary lesion.
Although the actual incidence and prevalence of ECS are not known, it constitutes 9–18% of ACTH-dependent CS cases [1, 2]. It has been reported that ECS occurs in 3.2–6% of NENs, and the tumor is often localized in the lung or thyroid in cases with ECS [4,5,6]. In UPO NENs, which constitute 13% of metastatic NENs, the most common cause of the functional syndrome is carcinoid syndrome; ACTH secretion can also be seen occasionally [3, 7]. Surgical series have reported that metastases often exist in the liver and peritoneal region, and the primary origin that can be detected intraoperatively is mostly in the small intestine [8,9,10].
Pituitary MRI is an important guide in the differential diagnosis of CD and ECS, but false-positive or false-negative imaging may be experienced, as in the present case [11]. CRH administration combined with BIPSS is still the “gold standard” method to differentiate ECS from CD [12]. Thin-slice whole-body CT is recommended as the first-line imaging method to detect the tumor focus [13, 14]. Although it is a very effective method for detecting overt tumors, pulmonary embolism and infections can mask small NENs on CT [2]. In the current case, the recent history of COVID-19 infection and the presence of multiple non-homogeneous opacities in the lungs may have limited the detection of a possible pulmonary carcinoid at presentation. However, functional imaging performed 2 months later revealed that previously observed non-homogeneous densities had mostly disappeared (Fig. 2c, d).
The superiority of 68Ga-SSTR PET/CT over octreoscan in detecting NEN has been demonstrated, while its sensitivity in detecting the primary tumor in occult NEN cases has been reported as 57% [2, 15]. Though 18FDG-PET/CT is effective in revealing NENs with aggressive behavior, it has limited benefit in defining slow-growing, well-differentiated NENs [13, 16, 17]. In the present case, both functional imaging methods were compatible with metastatic disease, and bone metastases were more extensive in 18FDG-PET/CT than 68Ga-SSTR PET/CT scan; however, the primary tumor could not be determined with either imaging method.
In the literature review, 35 cases of UPO NEN secreting ACTH have been previously reported [4, 18,19,20,21,22,23,24,25,26]. The female to male ratio of the 23 patients with available data was 13:10, and the age range of 10 of these patients was 30–55 years [18,19,20,21, 25]. The metastases were in the liver and abdominal cavity in the six cases whose metastatic sites were mentioned [4, 18, 19, 25]. However, in our case, the lesions confirming the diagnosis of NEN were in the mediastinal lymph nodes and bones. The absence of hepatic involvement may be attributed to the early presentation of the current case, whose primary source is probably not the gastroenteropancreatic region. In addition, bone metastases are more prevalent in pulmonary carcinoids, unlike digestive NENs [27].
In line with the recommendations of the European Neuroendocrine Tumor Society (ENETS) consensus report, in the context of metastatic presentation as in the current case, diffuse staining with TTF-1 and negative staining with CDX2, thyroglobulin, and calcitonin; the low Ki-67 labeling index; and the presence of two mitoses in 2 mm2 indicated that the origin was almost certainly an AC [3, 27, 28]. Locoregional and/or distant metastasis can be seen at the time of diagnosis in 15% of typical carcinoids and in about half of ACs with visible primaries [27]. The present case demonstrates that even ACs that cannot be visualized may present with metastatic disease.
While hormonal risk is dominant in occult tumors secreting ACTH, tumoral risk is prominent in UPO NENs. However, in all cases, it is recommended to control hypercortisolemia and treat related comorbidities first and then perform a diagnostic evaluation. Moreover, thromboprophylaxis and Pneumocystis jirovecii pneumonia prophylaxis should be started [2]. The effectiveness of metyrapone (ranging from 500 to 3750 mg/day) in controlling hypercortisolemia in both the short and the long term has been demonstrated in a retrospective analysis involving both CD and ECS patients [29]. In the current case, UFC levels were reduced to the normal range with the lowest dose of metyrapone (500 mg/day). When the symptoms of adrenal insufficiency appeared, hydrocortisone was added, and a “block and replace” regimen was applied as recommended [30]. In the 7-month follow-up period of our case, there was no additional problem other than controllable hypokalemia associated with metyrapone.
In the ENETS consensus report, it was emphasized that the treatment decision in UPO NEN cases should be made according to the tumor grade, functionality, somatostatin receptor (SSTR) status, spread of the tumor, and hepatic tumor burden [3]. In the current case, an advanced AC with a low proliferation index was hypothesized, and somatostatin analog (SSA) treatment and the CAPTEM regimen were initiated. In addition to the cytotoxic therapy, bone-specific treatments, including radiotherapy and anti-resorptive therapy, were applied due to the high tumor burden in the bones rather than because of the negative effects of CS.
SSA is recommended as first-line treatment in low proliferation index ACs with positive SSTR, but there is no clear consensus on the initial dose [27]. Randomized, placebo-controlled trials conducted in digestive NENs showed positive effects of octreotide LAR 30 mg and lanreotide 120 mg in tumor control [31, 32]. In the present case, after continued stabilization of hypercortisolemia and no disease progression detected on sequential imaging, SSA treatment was continued with an initial dose of 90 mg/month of lanreotide.
Although it is stated in the ENETS consensus report that the overall response rate is below 30% with current regimens in advanced ACs, it is recommended to administer cisplatin-based chemotherapy regimens in high proliferation index disease, and temozolomide alone or in combination or streptozotocin-based chemotherapy regimens in low proliferation index disease. mTOR inhibitors such as everolimus are recommended in advanced ACs after the failure of other treatments [27]. In a recent study, Al-Toubah et al. reported that by applying the CAPTEM regimen in 19 patients with advanced lung NENs, a partial response was obtained in 30% of the patients and stable disease in 55%, while some patients had a tolerable toxicity profile, although adverse reactions were experienced [33]. In the present case, significant regression in metastatic lesions was observed 4 months after the initiation of cytotoxic treatment without any adverse reaction.
In conclusion, ECS is a rare entity that requires rapid management of hypercortisolemia because it may lead to fatal consequences and often involves long diagnostic processes. Past or active infections and incidental lesions may cause confusion and lead to many additional examinations. As in the present case, even radiologically invisible NENs with a relatively low Ki-67 labeling index and low mitosis count can be revealed with distant metastases at the time of diagnosis. After controlling hypercortisolemia in UPO NEN cases, it is important to characterize the possible primary origin to arrive at a treatment decision. Although the benefit of current chemotherapy regimens in metastatic disease is limited, cytotoxic treatment regimens combined with surgery and/or radiotherapy when necessary should be applied using a patient-based approach.
References
Lacroix A, Feelders RA, Stratakis CA, Nieman LK (2015) Cushing’s syndrome. Lancet 386:913–927. https://doi.org/10.1016/S0140-6736(14)61375-1
Young J, Haissaguerre M, Viera-Pinto O, Chabre O, Baudin E, Tabarin A (2020) Management of endocrine disease: Cushing’s syndrome due to ectopic ACTH secretion: an expert operational opinion. Eur J Endocrinol 182:R29–R58. https://doi.org/10.1530/EJE-19-0877
Pavel M, Costa F, Capdevila J, Gross D, Kianmanesh R, Krenning E et al (2016) ENETS consensus guidelines update for the management of distant metastatic disease of intestinal, pancreatic, bronchial neuroendocrine neoplasms (NEN) and NEN of unknown primary site. Neuroendocrinology 103:172–185. https://doi.org/10.1159/000443167
Lase I, Strele I, Grönberg M, Kozlovacki G, Welin S, Janson ET (2020) Multiple hormone secretion may indicate worse prognosis in patients with ectopic Cushing’s syndrome. Hormones (Athens) 19:351–360. https://doi.org/10.1007/s42000-019-00163-z
Kamp K, Alwani RA, Korpershoek E, Franssen GJH, de Herder WW, Feelders RA (2016) Prevalence and clinical features of the ectopic ACTH syndrome in patients with gastroenteropancreatic and thoracic neuroendocrine tumors. Eur J Endocrinol 174:271–280. https://doi.org/10.1530/EJE-15-0968
Kaltsas GA, Besser GM, Grossman AB (2004) The diagnosis and medical management of advanced neuroendocrine tumors. Endocr Rev 25:458–511. https://doi.org/10.1210/er.2003-0014
Alexandraki K, Angelousi A, Boutzios G, Kyriakopoulos G, Rontogianni D, Kaltsas G (2017) Management of neuroendocrine tumors of unknown primary. Rev Endocr Metab Disord 18:423–431. https://doi.org/10.1007/s11154-017-9437-9
Wang Y-Z, Chauhan A, Rau J, Diebold AE, Opoku-Boateng A, Ramcharan T et al (2016) Neuroendocrine tumors (NETs) of unknown primary: is early surgical exploration and aggressive debulking justifiable? Chin Clin Oncol 5:4. https://doi.org/10.3978/j.issn.2304-3865.2016.02.03
Wang SC, Parekh JR, Zuraek MB et al (2010) Identification of unknown primary tumors in patients with neuroendocrine liver metastases. Arch Surg 145:276–280. https://doi.org/10.1001/archsurg.2010.10
Bhosale P, Shah A, Wei W et al (2013) Carcinoid tumours: predicting the location of the primary neoplasm based on the sites of metastases. Eur Radiol 23:400–407. https://doi.org/10.1007/s00330-012-2615-y
Trott MJ, Farah G, Stokes VJ, Wang LM, Grossman AB (2016) A thymic neuroendocrine tumour in a young female: a rare cause of relapsing and remitting Cushing’s syndrome. Endocrinol Diabetes Metab Case Rep 2016:160018. https://doi.org/10.1530/EDM-16-0018
Oldfield EH, Doppman JL, Nieman LK et al (1991) Petrosal sinus sampling with and without corticotropin-releasing hormone for the differential diagnosis of Cushing’s syndrome. N Engl J Med 325:897–905. https://doi.org/10.1056/NEJM199109263251301
Sookur PA, Sahdev A, Rockall AG et al (2009) Imaging in covert ectopic ACTH secretion: a CT pictorial review. Eur Radiol 19:1069–1078. https://doi.org/10.1007/s00330-008-1274-5
Zemskova MS, Gundabolu B, Sinaii N et al (2010) Utility of various functional and anatomic imaging modalities for detection of ectopic adrenocorticotropin-secreting tumors. J Clin Endocrinol Metab 95:1207–1219. https://doi.org/10.1210/jc.2009-2282
Gabriel S, Garrigue P, Dahan L et al (2018) Prospective evaluation of 68Ga-DOTATATE PET/CT in limited disease neuroendocrine tumours and/or elevated serum neuroendocrine biomarkers. Clin Endocrinol (Oxf) 89:155–163. https://doi.org/10.1111/cen.13745
Moore W, Freiberg E, Bishawi M et al (2013) FDG-PET imaging in patients with pulmonary carcinoid tumor. Clin Nucl Med 38:501–505. https://doi.org/10.1097/RLU.0b013e318279f0f5
Panagiotidis E, Alshammari A, Michopoulou S et al (2017) Comparison of the impact of 68Ga-DOTATATE and 18F-FDG PET/CT on clinical management in patients with neuroendocrine tumors. J Nucl Med 58:91–96. https://doi.org/10.2967/jnumed.116.178095
Kornely E, Schlaghecke R, Horster FA (1991) Palliative therapy of an ectopic cushing’s syndrome due to a metastatic carcinoid tumor. Klin Wochenschr 69:173–176. https://doi.org/10.1007/BF01665863
Takami H, Ogino Y, Tanaka K, Kubo A (1998) Somatostatin-receptor-negative carcinoid tumour responsible for Cushing’s syndrome. Eur J Surg Oncol 24:337–338. https://doi.org/10.1016/s0748-7983(98)80022-x
Aniszewski JP, Young WF Jr, Thompson GB, Grant CS, van Heerden JA (2001) Cushing syndrome doe to ectopic adrenocorticotropic hormone secretion. World J Surg 25:934–940. https://doi.org/10.1007/s00268-001-0032-5
Ilias I, Torpy DJ, Pacak K, Mullen N, Wesley RA, Nieman LK (2005) Cushing’s syndrome due to ectopic corticotropin secretion: twenty years’ experience at the National Institutes of Health. J Clin Endocrinol Metab 90:4955–4962. https://doi.org/10.1210/jc.2004-2527
Isidori AM, Kaltsas GA, Pozza C et al (2006) The ectopic adrenocorticotropin syndrome: clinical features, diagnosis, management, and long-term follow-up. J Clin Endocrinol Metab 91:371–377. https://doi.org/10.1210/jc.2005-1542
Ejaz S, Vassilopoulou-Sellin R, Busaidy NL et al (2011) Cushing syndrome secondary to ectopic adrenocorticotropic hormone secretion: the University of Texas MD Anderson Cancer Center Experience. Cancer 117:4381–4389. https://doi.org/10.1002/cncr.26029
Daskalakis K, Chatzelis E, Tsoli M et al (2019) Endocrine paraneoplastic syndromes in patients with neuroendocrine neoplasms. Endocrine 64:384–392. https://doi.org/10.1007/s12020-018-1773-3
Albani A, Berr CM, Beuschlein F et al (2019) A pitfall of bilateral inferior petrosal sinus sampling in cyclic Cushing’s syndrome. BMC Endocr Disord 19:105. https://doi.org/10.1186/s12902-019-0433-9
Wannachalee T, Turcu AF, Bancos I et al (2019) The clinical impact of [68Ga]-DOTATATE PET/CT for the diagnosis and management of ectopic adrenocorticotropic hormone–secreting tumours. Clin Endocrinol (Oxf) 91:288–294. https://doi.org/10.1111/cen.14008
Caplin ME, Baudin E, Ferolla P et al (2015) Pulmonary neuroendocrine (carcinoid) tumors: European Neuroendocrine Tumor Society expert consensus and recommendations for best practice for typical and atypical pulmonary carcinoids. Ann Oncol 26:1604–1620. https://doi.org/10.1093/annonc/mdv041
Kim JY, Hong S-M, Ro JY (2017) Recent updates on grading and classification of neuroendocrine tumors. Ann Diagn Pathol 29:11–16. https://doi.org/10.1016/j.anndiagpath.2017.04.00
Daniel E, Aylwin S, Mustafa O et al (2015) Effectiveness of metyrapone in treating Cushing’s syndrome: a retrospective multicenter study in 195 patients. J Clin Endocrinol Metab 100:4146–4154. https://doi.org/10.1210/jc.2015-2616
Corcuff J-B, Young J, Masquefa-Giraud P, Chanson P, Baudin E, Tabarin A (2015) Rapid control of severe neoplastic hypercortisolism with metyrapone and ketoconazole. Eur J Endocrinol 172:473–481. https://doi.org/10.1530/EJE-14-0913
Rinke A, Muller HH, Schade-Brittinger C et al (2009) Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID Study Group. J Clin Oncol 27:4656–4663. https://doi.org/10.1200/JCO.2009.22.8510
Caplin ME, Pavel M, Ćwikła JB et al (2016) Anti-tumour effects of lanreotide for pancreatic and intestinal neuroendocrine tumours: the CLARINET open-label extension study. Endocr Relat Cancer 23:191–199. https://doi.org/10.1530/ERC-15-0490
Al-Toubah T, Morse B, Strosberg J (2020) Capecitabine and temozolomide in advanced lung neuroendocrine neoplasms. Oncologist 25:e48–e52. https://doi.org/10.1634/theoncologist.2019-0361
Author information
Authors and Affiliations
Contributions
H.B., H.D., and P.A. designed the article. H.B., H.D., P.A., M.C., T.T.T., A.K.E., and S.A.D. performed the assays and collected and interpreted the data. H.B. and H.D. wrote the initial manuscript. T.T.T., M.K., M.E.S., B.U., M.O., and E.C. reviewed the manuscript critically. All authors approved the final version of the manuscript and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Informed consent
Written informed consent was obtained from the patient before the study.
Conflict of interest
The authors declare no competing interests.
Consent to publish
Written informed consent was provided from the patient for publication of this case report and accompanying images.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bostan, H., Duger, H., Akhanli, P. et al. Cushing’s syndrome due to adrenocorticotropic hormone-secreting metastatic neuroendocrine tumor of unknown primary origin: a case report and literature review. Hormones 21, 147–154 (2022). https://doi.org/10.1007/s42000-021-00316-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42000-021-00316-z