Abstract
Purpose
Diabetic ketoacidosis (DKA) is a rare and life-threatening complication in patients with diabetes. Sodium–glucose co-transporter-2 inhibitors (SGLT2i) have rarely been associated with ketoacidosis. The aim of this retrospective study was to investigate DKA episodes occurring after SGLT2i treatment and to compare them to DKA episodes due to other causes.
Methods
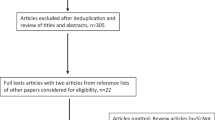
The medical records of the years 2018–2020 related to clinical and biochemical characteristics and to treatment of six patients with DKA due to SGLT2i were reviewed. They were compared to those of 12 patients with DKA due to other causes.
Results
On admission, the most common symptom was abdominal pain. Glucose levels (median, min–max) were lower in patients with SGLT2i-induced DKA compared to those with DKA due to other causes (229 (150–481) vs. 458.5 (332–695) mg/dl, p = 0.007), whereas no statistical difference was observed in HbA1c and in the severity of DKA (pH, HCO3, CO2, and anion gap). The duration of insulin infusion (41 (33–124) vs. 21.50 (11–32) h, p < 0.001) and the time required until DKA resolution (39 (31–120) vs. 19 (9–28) h, p < 0.001) were higher in patients with SGLT2i-induced DKA than those with DKA due to other causes. In addition, there were increased fluid requirements (14 (8–22.75) vs. 5.5 (2–24) L, p = 0.013) and longer hospitalization time (11 (6–22) vs. 5.5 (2–14) days, p = 0.024) in patients with SGLT2i-induced DKA. No statistically significant differences were observed in total intravenous insulin and potassium administration until DKA resolution.
Conclusions
Patients with SGLT2i-induced DKA had lower serum glucose levels on admission and required increased fluid administration and longer time to recover from acidosis compared to patients with DKA from other causes.

Similar content being viewed by others
References
Benoit SR, Zhang Y, Geiss LS, Gregg EW, Albright A (2018) Trends in diabetic ketoacidosis hospitalizations and in-hospital mortality - United States, 2000-2014. MMWR Morb Mortal Wkly Rep 67:362–365. https://doi.org/10.15585/mmwr.mm6712a3
Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN (2009) Hyperglycemic crises in adult patients with diabetes. Diabetes Care 32:1335–1343. https://doi.org/10.2337/dc09-9032
Garber AJ, Handelsman Y, Grunberger G et al (2020) Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm-2020 executive summary. Endocr Pract 26:107–139. https://doi.org/10.4158/CS-2019-0472
Fattah H, Vallon V (2018) The potential role of SGLT2 inhibitors in the treatment of type 1 diabetes mellitus. Drugs 78:717–726. https://doi.org/10.1007/s40265-018-0901-y
Zinman B, Wanner C, Lachin JM et al (2015) Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 373:2117–2212. https://doi.org/10.1056/NEJMoa1504720
Wanner C, Inzucchi SE, Lachin JM et al (2016) Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med 375:323–334. https://doi.org/10.1056/NEJMoa1515920
Neal B, Perkovic V, Mahaffey KW et al (2017) Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med 377:644–657. https://doi.org/10.1056/NEJMoa1611925
Wiviott SD, Raz I, Bonaca MP et al (2019) Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med 380:347–357. https://doi.org/10.1056/NEJMoa1812389
Taylor SI, Blau JE, Rother KI (2015) SGLT2 inhibitors may predispose to ketoacidosis. J Clin Endocrinol Metab 100:2849–2852. https://doi.org/10.1210/jc.2015-1884
Erondu N, Desai M, Ways K, Meininger G (2015) Diabetic ketoacidosis and related events in the canagliflozin type 2 diabetes clinical program. Diabetes Care 38:1680–1686. https://doi.org/10.2337/dc15-1251
Henry RR, Thakkar P, Tong C, Polidori D, Alba M (2015) Efficacy and safety of canagliflozin, a sodium-glucose cotransporter 2 inhibitor, as add-on to insulin in patients with type I diabetes. Diabetes Care 38:2258–2265. https://doi.org/10.2337/dc15-1730
Hamblin PS, Wong R, Ekinci EI et al (2019) SGLT2 inhibitors increase the risk of diabetic ketoacidosis developing in the community and during hospital admission. J Clin Endocrinol Metab 104:3077–3087. https://doi.org/10.1210/jc.2019-00139
Peters AL, Buschur EO, Buse JB, Cohan P, Diner JC, Hirsch IB (2015) Euglycemic diabetic ketoacidosis: a potential complication of treatment with sodium-glucose cotransporter2 inhibition. Diabetes Care 38:1687–1693. https://doi.org/10.2337/dc15-0843
Meyer EJ, Gabb G, Jesudason D (2018) SGLT2 inhibitor-associated euglycemic diabetic ketoacidosis: a South Australian clinical case series and Australian spontaneous adverse event notifications. Diabetes Care 41:e47–e49. https://doi.org/10.2337/dc17-1721
Ueda P, Svanström H, Melbye M et al (2018) Sodium glucose cotransporter 2 inhibitors and risk of serious adverse events: nationwide register based cohort study. BMJ 363:k4365. https://doi.org/10.1136/bmj.k4365
Patakfalvi L, Brazeau AS, Dasgupta K (2018) Physician experiences with sodium-glucose cotransporter (SGLT2) inhibitors, a new class of medications in type 2 diabetes, and adverse effects. Prim Health Care Res Dev 23:1–6. https://doi.org/10.1017/S1463423618000476
Blau JE, Tella SH, Taylor SI, Rother KI (2017) Ketoacidosis associated with SGLT2 inhibitor treatment: analysis of FAERS data. Diabetes Metab Res Rev 33(8). https://doi.org/10.1002/dmrr.2924
Hayami T, Kato Y, Kamiya H et al (2015) Case of ketoacidosis by a sodium-glucose cotransporter 2 inhibitor in a diabetic patient with a low-carbohydrate diet. J Diabetes Investig 6:587–590. https://doi.org/10.1111/jdi.12330
Hine J, Paterson H, Abrol E et al (2015) SGLT inhibition and euglycaemic diabetic ketoacidosis. Lancet Diabetes Endocrinol 3:503–504. https://doi.org/10.1016/S2213-8587(15)00204-1
Roach P, Skierczynski P (2016) Euglycemic diabetic ketoacidosis in a patient with type 2 diabetes after treatment with empagliflozin. Diabetes Care 39:e3. https://doi.org/10.2337/dc15-1797
Lucero P, Chapela S (2018) Euglycemic diabetic ketoacidosis in the ICU: 3 case reports and review of literature. Case Rep Crit Care 1747850. https://doi.org/10.1155/2018/1747850
Iqbal I, Hamid M, Khan MAA, Kainat A, Tariq S (2019) Dapagliflozin-induced late-onset euglycemic diabetic ketoacidosis. Cureus. 11:e6089. https://doi.org/10.7759/cureus.6089
Diaz-Ramos A, Eilbert W, Marquez D (2019) Euglycemic diabetic ketoacidosis associated with sodium-glucose cotransporter-2 inhibitor use: a case report and review of the literature. Int J Emerg Med 12:27. https://doi.org/10.1186/s12245-019-0240-0
McLachlan G, Keith C, Frauman A (2019) Diabetic ketoacidosis with sodium-glucose cotransporter type 2 inhibitors: a case series. Med J Aust 211:237–237.e1. https://doi.org/10.5694/mja2.50302
Dorcely B, Nitis J, Schwartzbard A et al (2020) A case report: euglycemic diabetic ketoacidosis presenting as chest pain in a patient on a low carbohydrate diet. Curr Diabetes Rev. https://doi.org/10.2174/1573399816666200316112709
Fioretto P, Zambon A, Rossato M, Busetto L, Vettor R (2016) SGLT2 inhibitors and the diabetic kidney. Diabetes Care 39(Suppl 2):S165–S171. https://doi.org/10.2337/dcS15-3006
Gerich JE (2010) Role of the kidney in normal glucose homeostasis and in the hyperglycaemia of diabetes mellitus: therapeutic implications. Diabet Med 27:136–142. https://doi.org/10.1111/j.1464-5491.2009.02894.x
Campbell JE, Drucker DJ (2015) Islet α cells and glucagon-critical regulators of energy homeostasis. Nat Rev Endocrinol 11:329–338. https://doi.org/10.1038/nrendo.2015.51
Umpierrez G, Freire AX (2002) Abdominal pain in patients with hyperglycemic crises. J Crit Care 17:63–67. https://doi.org/10.1053/jcrc.2002.33030
Jeon JY, Kim SK, Kim KS et al (2019) DKA Study Group of Gyeonin Branch of the Korean Diabetes Association Clinical characteristics of diabetic ketoacidosis in users and non-users of SGLT2 inhibitors. Diabetes Metab 45:453–457. https://doi.org/10.1016/j.diabet.2019.01.001
Goldenberg RM, Berard LD, Cheng AYY et al (2016) SGLT2 inhibitor-associated diabetic ketoacidosis: clinical review and recommendations for prevention and diagnosis. Clin Ther 38:2654–2664.e1. https://doi.org/10.1016/j.clinthera.2016.11.002
Handelsman Y, Henry RR, Bloomgarden ZT et al (2016) American Association of Clinical Endocrinologists and American College of Endocrinology position statement on the association of SGLT-2 inhibitors and diabetic ketoacidosis. Endocr Pract 22:753–762. https://doi.org/10.4158/EP161292.PS
Danne T, Garg S, Peters AL et al (2019) International consensus on risk management of diabetic ketoacidosis in patients with type 1 diabetes treated with sodium-glucose cotransporter (SGLT) inhibitors. Diabetes Care 42:1147–1154. https://doi.org/10.2337/dc18-2316
Rafey MF, Butt A, Coffey B et al (2019) Prolonged acidosis is a feature of SGLT2i-induced euglycaemic diabetic ketoacidosis. Endocrinol Diabetes Metab Case Rep 19-0087:EDM190087. https://doi.org/10.1530/EDM-19-0087
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The study protocol is approved from the Scientific Committee of the General Hospital of Athens ‘G Gennimatas’, Greece (reference number 15238/30.06.2020), and the reporting of the study conforms to the Guidelines for Good Clinical Practice, the Declaration of Helsinki.
Informed consent
Informed consent for research and scientific reasons is routinely collected from each patient admitted to the Endocrinology Unit.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Papanastasiou, L., Glycofridi, S., Gravvanis, C. et al. Diabetic ketoacidosis in patients treated with SGLT2 inhibitors: experience at a tertiary hospital. Hormones 20, 369–376 (2021). https://doi.org/10.1007/s42000-020-00256-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42000-020-00256-0