Key summary points
To provide evidence-based medical evidence for Tai Chi exercise in improving the sleep quality of the older adults living in the community.
AbstractSection FindingTai Chi exercise has been found to notably enhance the sleep quality of older adults residing in the community, in comparison to engaging in routine activities.
AbstractSection MessageTai Chi exercise proves to be an excellent choice for older adults residing in the community in their later years, promoting their overall well-being and health.
Abstract
Purpose
While clinical research has shown that Tai Chi exercise may improve the sleep quality of older adults, there is a lack of robust evidence-based verification. Therefore, this study conducted a systematic review of published research on the effect of Tai Chi exercise on the sleep quality of community-dwelling older adults, aiming to provide solid evidence-based medicine to enhance their sleep quality.
Methods
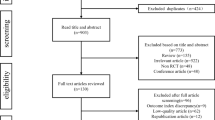
A systematic search was conducted on PubMed, Embase, Cochrane Library, Web of Science, CNKI, WanFang, VIP, and SinoMed databases from their inception to December 9, 2022. The Cochrane risk of bias assessment tool 2.0 was used to assess the risk of bias in the included studies.
Results
This systematic review included 12 original articles, involving a total of 1,058 community-dwelling older adults, with 553 in the Tai Chi group and 505 in the control group. The meta-analysis results revealed a significant improvement in the sleep quality of community-dwelling older adults who practiced Tai Chi compared to the control group [WMD = − 1.96 (95% CI: − 3.02 to − 0.90, z = 3.62, P < 0.001)]. Subgroup analysis showed that Tai Chi had significantly beneficial effects regardless of age, country/region, intervention time, and Tai Chi type.
Conclusions
Tai Chi exercise can serve as an effective non-medication approach for addressing sleep problems in this demographic. Among the various types of Tai Chi exercises, the 24-form Tai Chi exercise emerges as a preferred option. Moreover, Tai Chi exercise proves to be an excellent choice for older people in their later years, promoting their overall well-being and health.






Similar content being viewed by others
Data availability
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
Lee YH, Lee YH, Wu YH, Liu CT, Chang YC (2022) A 10-year trend of sleeping patterns, geographical, and community disparities among Chinese older adults. J Appl Gerontol 41:1301–1311. https://doi.org/10.1177/07334648211072549
Shi WH, Zhang HY, Zhang J, Lyu YB, Brasher MS, Yin ZX et al (2016) The status and associated factors of successful aging among older adults residing in longevity areas in China. Biomed Environ Sci 29:347–355. https://doi.org/10.3967/bes2016.045
Varrasse M, Li J, Gooneratne N (2015) Exercise and sleep in community-dwelling older adults. Curr Sleep Med Rep 1:232–240. https://doi.org/10.1007/s40675-015-0028-6
Han D, Cheng J, Qu J, Wen X, Liu X, Chen Y et al (2022) Effectiveness of Taijiquan in treating insomnia: A systematic review and meta-analysis of randomized controlled studies. Front Psychiatry 13:892453. https://doi.org/10.3389/fpsyt.2022.892453
Nowell PD, Mazumdar S, Buysse DJ, Dew MA, Reynolds CF 3rd, Kupfer DJ (1997) Benzodiazepines and zolpidem for chronic insomnia: a meta-analysis of treatment efficacy. JAMA 278:2170–2177
Lader M (2014) Benzodiazepine harm: how can it be reduced? Br J Clin Pharmacol 77:295–301. https://doi.org/10.1111/j.1365-2125.2012.04418.x
Holbrook AM, Crowther R, Lotter A, Cheng C, King D (2000) Meta-analysis of benzodiazepine use in the treatment of insomnia. CMAJ 162:225–233
Gooneratne NS, Vitiello MV (2014) Sleep in older adults: normative changes, sleep disorders, and treatment options. Clin Geriatr Med 30:591–627. https://doi.org/10.1016/j.cger.2014.04.007
Irwin MR, Cole JC, Nicassio PM (2006) Comparative meta-analysis of behavioral interventions for insomnia and their efficacy in middle-aged adults and in older adults 55+ years of age. Health Psychol 25:3–14. https://doi.org/10.1037/0278-6133.25.1.3
Yang PY, Ho KH, Chen HC, Chien MY (2012) Exercise training improves sleep quality in middle-aged and older adults with sleep problems: a systematic review. J Physiother 58:157–163. https://doi.org/10.1016/s1836-9553(12)70106-6
Fank F, Pereira FDS, Dos Santos L, de Mello MT, Mazo GZ (2022) Effects of exercise on sleep in older adults: an overview of systematic reviews and meta-analyses. J Aging Phys Act 30:1101–1117. https://doi.org/10.1123/japa.2021-0444
Tseng TH, Chen HC, Wang LY, Chien MY (2020) Effects of exercise training on sleep quality and heart rate variability in middle-aged and older adults with poor sleep quality: a randomized controlled trial. J Clin Sleep Med 16:1483–1492. https://doi.org/10.5664/jcsm.8560
Zhang W, Liu Y, Yu J, Li D, Jia Y, Zhang Q et al (2022) Exercise improves sleep quality in older adults: a protocol for a systematic review and meta-analysis. BMJ Open 12:e047555. https://doi.org/10.1136/bmjopen-2020-047555
Di Lorito C, Long A, Byrne A, Harwood RH, Gladman JRF, Schneider S et al (2021) Exercise interventions for older adults: a systematic review of meta-analyses. J Sport Health Sci 10:29–47. https://doi.org/10.1016/j.jshs.2020.06.003
Urquiza M, Echeverria I, Besga A, Amasene M, Labayen I, Rodriguez-Larrad A et al (2020) Determinants of participation in a post-hospitalization physical exercise program for older adults. BMC Geriatr 20:408. https://doi.org/10.1186/s12877-020-01821-3
Chen YM (2010) Perceived barriers to physical activity among older adults residing in long-term care institutions. J Clin Nurs 19:432–439. https://doi.org/10.1111/j.1365-2702.2009.02990.x
Guerin M, Mackintosh S, Fryer C (2008) Exercise class participation among residents in low-level residential aged care could be enhanced: a qualitative study. Aust J Physiother 54:111–117. https://doi.org/10.1016/s0004-9514(08)70044-8
Lan C, Lai JS, Chen SY (2002) Tai Chi Chuan: an ancient wisdom on exercise and health promotion. Sports Med 32:217–224. https://doi.org/10.2165/00007256-200232040-00001
Nyman SR (2022) Virtual Special Issue: Tai Chi. J Aging Phys Act, 30:745–746, doi:https://doi.org/10.1123/japa.2022-0248.
Wang F, Lee EK, Wu T, Benson H, Fricchione G, Wang W et al (2014) The effects of tai chi on depression, anxiety, and psychological well-being: a systematic review and meta-analysis. Int J Behav Med 21:605–617. https://doi.org/10.1007/s12529-013-9351-9
Li F, Harmer P, Fisher KJ, McAuley E, Chaumeton N, Eckstrom E et al (2005) Tai Chi and fall reductions in older adults: a randomized controlled trial. J Gerontol A Biol Sci Med Sci 60:187–194. https://doi.org/10.1093/gerona/60.2.187
You Y, Min L, Tang M, Chen Y, Ma X (2021) Bibliometric evaluation of global Tai Chi research from 1980–2020. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph18116150
Huang J, Wang D, Wang J (2021) Clinical evidence of Tai Chi exercise prescriptions: a systematic review. Evid Based Complement Alternat Med 2021:5558805. https://doi.org/10.1155/2021/5558805
Wang L, Zhang Y (2020) Tai Chi exercise behavior of the elderly and its effects on health. J Sports Res 34:79–85. https://doi.org/10.15877/j.cnki.nsic.20201229.001
Zhong D, Xiao Q, Xiao X, Li Y, Ye J, Xia L et al (2020) Tai Chi for improving balance and reducing falls: An overview of 14 systematic reviews. Ann Phys Rehabil Med 63:505–517. https://doi.org/10.1016/j.rehab.2019.12.008
Sherrington C, Fairhall NJ, Wallbank GK, Tiedemann A, Michaleff ZA, Howard K et al (2019) Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD012424.pub2
Du S, Dong J, Zhang H, Jin S, Xu G, Liu Z et al (2015) Taichi exercise for self-rated sleep quality in older people: a systematic review and meta-analysis. Int J Nurs Stud 52:368–379. https://doi.org/10.1016/j.ijnurstu.2014.05.009
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62:1006–1012. https://doi.org/10.1016/j.jclinepi.2009.06.005
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4:1. https://doi.org/10.1186/2046-4053-4-1
Devine EB, Hakim Z, Green J (2005) A systematic review of patient-reported outcome instruments measuring sleep dysfunction in adults. Pharmacoeconomics 23:889–912. https://doi.org/10.2165/00019053-200523090-00003
Fabbri M, Beracci A, Martoni M, Meneo D, Tonetti L, Natale V (2021) Measuring subjective sleep quality: a review. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph18031082
Li F, Fisher KJ, Harmer P, Shirai M (2003) A simpler eight-form easy tai chi for elderly adults. J Aging Phys Act 11:206–218
Wolf SL, Coogler C, Xu T (1997) Exploring the basis for Tai Chi Chuan as a therapeutic exercise approach. Arch Phys Med Rehabil 78:886–892. https://doi.org/10.1016/s0003-9993(97)90206-9
China Sports Editorial Board (1980) Simplified “taijiquan,” 1st edn. China Sports Editorial Board, Beijing
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898. https://doi.org/10.1136/bmj.l4898
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28:193–213. https://doi.org/10.1016/0165-1781(89)90047-4
Cudney LE, Frey BN, McCabe RE, Green SM (2022) Investigating the relationship between objective measures of sleep and self-report sleep quality in healthy adults: a review. J Clin Sleep Med 18:927–936. https://doi.org/10.5664/jcsm.9708
Liu R, Yao W (2010) Influence of 8-week shadowboxing exercise on the indexes for evaluating sleep behavior in elderly people. Chinese Journal of Geriatric Care 8:26–27
Taylor-Piliae RE, Hoke TM, Hepworth JT, Latt LD, Najafi B, Coull BM (2014) Effect of Tai Chi on physical function, fall rates and quality of life among older stroke survivors. Arch Phys Med Rehabil 95:816–824. https://doi.org/10.1016/j.apmr.2014.01.001
Nguyen MH, Kruse A (2012) A randomized controlled trial of Tai chi for balance, sleep quality and cognitive performance in elderly Vietnamese. Clin Interv Aging 7:185–190. https://doi.org/10.2147/cia.S32600
Yongwen F (2020) Experimental study on improving sleep quality of elderly people by Taichi Engineering and Technological Research.5:246-8. doi:https://doi.org/10.3969/j.issn.1671-3818.2020.10.114
Jie DH (2013) Effects of outdoor Tai Chi exercise combined with folk music on the mental health and sleep quality of elderly residents in the community. Chin J Gerontol 17:4229–4230
Siu PM, Yu AP, Tam BT, Chin EC, Yu DS, Chung KF et al (2021) Effects of Tai Chi or exercise on sleep in older adults with insomnia: a randomized clinical trial. JAMA Netw Open 4:e2037199. https://doi.org/10.1001/jamanetworkopen.2020.37199
Song J, Wei L, Cheng K, Lin Q, Xia P, Wang X et al (2022) The effect of modified Tai Chi exercises on the physical function and quality of life in elderly women with knee osteoarthritis. Front Aging Neurosci 14:860762. https://doi.org/10.3389/fnagi.2022.860762
Irwin MR, Olmstead R, Carrillo C, Sadeghi N, Breen EC, Witarama T et al (2014) Cognitive behavioral therapy vs. Tai Chi for late life insomnia and inflammatory risk: a randomized controlled comparative efficacy trial. Sleep 37:1543–1552. https://doi.org/10.5665/sleep.4008
Li F, Fisher KJ, Harmer P, Irbe D, Tearse RG, Weimer C (2004) Tai chi and self-rated quality of sleep and daytime sleepiness in older adults: a randomized controlled trial. J Am Geriatr Soc 52:892–900. https://doi.org/10.1111/j.1532-5415.2004.52255.x
Irwin MR, Olmstead R, Motivala SJ (2008) Improving sleep quality in older adults with moderate sleep complaints: A randomized controlled trial of Tai Chi Chih. Sleep 31:1001–1008
Lü J, Huang L, Wu X, Fu W, Liu Y (2017) Effect of Tai Ji Quan training on self-reported sleep quality in elderly Chinese women with knee osteoarthritis: a randomized controlled trail. Sleep Med 33:70–75. https://doi.org/10.1016/j.sleep.2016.12.024
Frye B, Scheinthal S, Kemarskaya T, Pruchno R (2007) Tai chi and low impact exercise: effects on the physical functioning and psychological well-being of older people. J Appl Gerontol 26:433–453
Easwaran K, Gopalasingam Y, Green DD, Lach V, Melnyk JA, Wan C et al (2021) Effectiveness of Tai Chi for health promotion for adults with health conditions: a scoping review of Meta-analyses. Disabil Rehabil 43:2978–2989. https://doi.org/10.1080/09638288.2020.1725916
Wang C, Schmid CH, Fielding RA, Harvey WF, Reid KF, Price LL et al (2018) Effect of tai chi versus aerobic exercise for fibromyalgia: comparative effectiveness randomized controlled trial. BMJ 360:k851. https://doi.org/10.1136/bmj.k851
Chao M, Wang C, Dong X, Ding M (2018) The effects of Tai Chi on type 2 diabetes mellitus: a meta-analysis. J Diabetes Res 2018:7350567. https://doi.org/10.1155/2018/7350567
Huston P, McFarlane B (2016) Health benefits of tai chi: What is the evidence? Can Fam Physician 62:881–890
Niño A, Villa-Vicente JG, P SC, (2022) Functional capacity of Tai Chi-practicing elderly people. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph19042178
Song R, Ahn S, So H, Lee EH, Chung Y, Park M (2015) Effects of Tai Chi on balance: a population-based meta-analysis. J Altern Complement Med 21:141–151. https://doi.org/10.1089/acm.2014.0056
Zhang Y, Han P, Yin N, Huang Y, Li C, Lian H et al (2021) The effects of long-term Tai-Chi practice on blood pressure under normal conditions. Am J Med Sci 361:598–606. https://doi.org/10.1016/j.amjms.2020.11.008
Li H, Chen J, Xu G, Duan Y, Huang D, Tang C et al (2020) The effect of Tai Chi for improving sleep quality: a systematic review and meta-analysis. J Affect Disord 274:1102–1112. https://doi.org/10.1016/j.jad.2020.05.076
Yaremchuk K (2018) Sleep disorders in the elderly. Clin Geriatr Med 34:205–216. https://doi.org/10.1016/j.cger.2018.01.008
Asplund R (1999) Sleep disorders in the elderly. Drugs Aging 14:91–103. https://doi.org/10.2165/00002512-199914020-00002
Wu WW, Kwong E, Lan XY, Jiang XY (2015) The effect of a meditative movement intervention on quality of sleep in the elderly: a systematic review and meta-analysis. J Altern Complement Med 21:509–519. https://doi.org/10.1089/acm.2014.0251
Wang X, Li P, Pan C, Dai L, Wu Y, Deng Y (2019) The effect of mind-body therapies on insomnia: a systematic review and meta-analysis. Evid Based Complement Alternat Med 2019:9359807. https://doi.org/10.1155/2019/9359807
Raman G, Zhang Y, Minichiello VJ, D’Ambrosio CM, Wang C (2013) Tai Chi improves sleep quality in healthy adults and patients with chronic conditions: a systematic review and meta-analysis. J Sleep Disord Ther. https://doi.org/10.4172/2167-0277.1000141
Si Y, Wang C, Yin H, Zheng J, Guo Y, Xu G et al (2020) Tai Chi Chuan for subjective sleep quality: a systematic review and meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med 2020:4710527. https://doi.org/10.1155/2020/4710527
Wang CC, Li K, Gaylord AS (2022) Trends and characteristics of Tai Chi and Qi Gong use among U.S. adults: Results from the 2007–2017 National Health Interview Survey. Complement Ther Med 71:102890. https://doi.org/10.1016/j.ctim.2022.102890
Vanderlinden J, Boen F, van Uffelen JGZ (2020) Effects of physical activity programs on sleep outcomes in older adults: a systematic review. Int J Behav Nutr Phys Act 17:11. https://doi.org/10.1186/s12966-020-0913-3
Acknowledgements
Not applicable.
Funding
The authors declare that they did not receive any funding from any source.
Author information
Authors and Affiliations
Contributions
Conception and design: LL, Administrative support: LL, Provision of study materials or patients: LL and YL, Collection and assembly of data: LL, YL, JS, Data analysis and interpretation: LL, XF, OE, Manuscript writing: LL, YL, XF, JS, OE, Final approval of manuscript: LL.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lyu, L., Li, Y., Fan, X. et al. The effect of Tai Chi exercise intervention on sleep quality in community residing older adults: a systematic review and meta-analysis. Eur Geriatr Med 15, 381–396 (2024). https://doi.org/10.1007/s41999-023-00923-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-023-00923-6