Key summary points
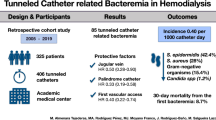
To compare clinical characteristics, microbiology, and outcomes of tunneled catheter-related bloodstream infections among old (aged ≥ 75) versus younger chronic hemodialysis patients.
AbstractSection FindingsThe clinical presentation among old versus younger patients’ groups was similar. However, the rate of resistant pathogens was considerably higher among older adults. Overall mortality rate (in-hospital and 90-day mortality) was high in both groups.
AbstractSection MessagePoor clinical outcome following an episode of catheter-related bloodstream infection among old hemodialysis patients suggests that the use of tunneled catheters as a permanent vascular access should be discouraged.
Abstract
Background
The use of a tunneled catheter as the primary vascular access among old hemodialysis patients is frequent. Catheter-related bloodstream infection (CRBSI) is a common complication, associated with increased mortality. Data regarding the clinical presentation and outcomes of CRBSI among old hemodialysis patients is limited.
Methods
All chronic hemodialysis patients hospitalized between 2010 and 2022 with CRBSI were included. Patients were classified into two groups: old adults (≥ 75) and younger patients. Clinical, microbiological, and outcome data were collected and analyzed.
Results
One hundred and fifty-four patients with CRBSI were identified. Fifty-seven were aged ≥ 75 years. Mean age in the older and younger groups was 81.2 ± 5 and 59.7 ± 12.7, respectively. Male gender was predominant (64%). Charlson comorbidity score and Pitt bacteremia score were comparable among both groups. Norton score < 14 was more common among old persons (n = 24, 67% versus n = 21, 31%, p < 0.001), as well as nursing-home residence. Gram-negative pathogens and Staphylococcus aureus were common in both groups. The frequency of inappropriate empirical antimicrobial treatment was higher among older persons. Overall, in-hospital and 90-day mortality was high (age ≥ 75, 36.8%, age < 75, 24.7%, p = 0.14). Age was not significantly associated with mortality after adjustment for low Norton score, residence, and inappropriate antimicrobial therapy as well as resistance patterns of bloodstream isolates [OR = 1.2 (95% CI 0.4–3.3), p = 0.76].
Conclusions
Clinical characteristics and outcomes of CRBSI were comparable among old and young hemodialysis patients. However, the high mortality rate in this cohort suggests that the use of tunneled catheters as a permanent vascular access should be discouraged in both patient groups.

Similar content being viewed by others
References
Powe NR, Jaar B, Furth SL, Hermann J, Briggs W (1999) Septicemia in dialysis patients: incidence, risk factors, and prognosis. Kidney Int 55:1081–1090
Skov Dalgaard L, Nørgaard M, Jespersen B, Jensen-Fangel S, Østergaard LJ, Schønheyder HC et al (2015) Risk and prognosis of bloodstream infections among patients on chronic hemodialysis: a population-based cohort study. PLoS ONE 10:e0124547
Vanholder R, Canaud B, Fluck R, Jadoul M, Labriola L, Marti-Monros A et al (2010) Diagnosis, prevention and treatment of haemodialysis catheter-related bloodstream infections (CRBSI): a position statement of European Renal Best Practice (ERBP). NDT Plus 3:234–246
Chan CT, Blankestijn PJ, Dember LM, Gallieni M, Harris DCH, Lok CE et al (2019) Dialysis initiation, modality choice, access, and prescription: conclusions from a kidney disease: improving global outcomes (KDIGO) controversies conference. Kidney Int 96:37–47
Lok CE, Huber TS, Lee T, Shenoy S, Yevzlin AS, Abreo K, National Kidney Foundation et al (2020) KDOQI Clinical practice guideline for vascular access: 2019 update. Am J Kidney Dis 75:S1–S164
Almenara-Tejederas M, Rodríguez-Pérez MA, Moyano-Franco MJ, de Cueto-López M, Rodríguez-Baño J, Salgueira-Lazo M (2023) Tunneled catheter-related bacteremia in hemodialysis patients: incidence, risk factors and outcomes. A 14-year observational study. J Nephrol 36:203–212
Allon M (2004) Dialysis catheter-related bacteremia: treatment and prophylaxis. Am J Kidney Dis 44:779–791
Kurella M, Covinsky KE, Collins AJ, Chertow GM (2007) Octogenarians and nonagenarians starting dialysis in the United States. Ann Intern Med 146:177–183
Choi HS, Han KD, Oh TR, Suh SH, Kim M, Kim CS et al (2021) Trends in the incidence and prevalence of end-stage renal disease with hemodialysis in entire Korean population: a nationwide population-based study. Medicine (Baltimore) 100:e25293
Pisoni RL, Zepel L, Port FK, Robinson BM (2015) Trends in US vascular access use, patient preferences, and related practices: an update from the US DOPPS practice monitor with international comparisons. Am J Kidney Dis 65:905–915
Mendelssohn DC, Ethier J, Elder SJ, Saran R, Port FK, Pisoni RL (2006) Haemodialysis vascular access problems in Canada: results from the dialysis outcomes and practice patterns study (DOPPS II). Nephrol Dial Transplant 21:721–728
Lazarides MK, Georgiadis GS, Antoniou GA, Staramos DN (2007) A meta-analysis of dialysis access outcome in elderly patients. J Vasc Surg 45:420–426
Richardson AI, Leake A, Schmieder GC, Biuckians A, Stokes GK, Panneton JM et al (2009) Should fistulas really be first in the elderly patient? J Vasc Access 10:199–202
Murea M, James KM, Russell GB, Byrum GV 3rd, Yates JE, Tuttle NS, Bleyer AJ, Burkart JM, Freedman BI (2014) Risk of catheter-related bloodstream infection in elderly patients on hemodialysis. Clin J Am Soc Nephrol 9:764–770
Poinen K, Quinn RR, Clarke A, Ravani P, Hiremath S, Miller LM et al (2019) Complications from tunneled hemodialysis catheters: a canadian observational cohort study. Am J Kidney Dis 73:467–475
Zanoni F, Pavone L, Binda V, Tripepi G, D’Arrigo G, Scalamogna A et al (2021) Catheter-related bloodstream infections in a nephrology unit: analysis of patient- and catheter-associated risk factors. J Vasc Access 22:337–343
Vascular Access Work Group (2006) Clinical practice guidelines for vascular access. Am J Kidney Dis 48:S248–S273. https://doi.org/10.1053/j.ajkd.2006.04.040
Boenink R, Astley ME, Huijben JA, Stel VS, Kerschbaum J, Ots-Rosenberg M, Åsberg AA et al (2021) The ERA registry annual report 2019: summary and age comparisons. Clin Kidney J 15(3):452–472. https://doi.org/10.1093/ckj/sfab273.PMID:35211303;PMCID:PMC8862051
Collins AJ, Foley RN, Herzog C, Chavers B, Gilbertson D, Ishani A et al (2009) United States renal data system 2008 annual data report. Am J Kidney Dis 53:S1-374. https://doi.org/10.1053/j.ajkd.2008.10.005
Dalrymple LS, Johansen KL, Chertow GM, Cheng SC, Grimes B, Gold EB et al (2010) Infection-related hospitalizations in older patients with ESRD. Am J Kidney Dis 56:522–530. https://doi.org/10.1053/j.ajkd.2010.04.016
Yernard C, Breining A, Duc S, Kobeh D, Dubos M, Prevel R et al (2019) Presentation of bacteremia in older patients is a risk factor for death. Am J Med 132:1344–1352
Al-Solaiman Y, Estrada E, Allon M (2011) The spectrum of infections in catheter-dependent hemodialysis patients. Clin J Am Soc Nephrol 6:2247–2252. https://doi.org/10.2215/CJN.03900411
Sychev D, Maya ID, Allon M (2011) Clinical management of dialysis catheter-related bacteremia with concurrent exit-site infection. Semin Dial 24:239–241. https://doi.org/10.1111/j.1525-139X.2011.00869.x.PMID:21517993;PMCID:PMC4017937
Alexandraki I, Sullivan R, Zaiden R, Bailey C, McCarter Y, Khan A et al (2008) Blood culture isolates in hemodialysis vascular catheter-related bacteremia. Am J Med Sci 336:297–302
Farrington CA, Allon M (2019) Complications of hemodialysis catheter bloodstream infections: impact of infecting organism. Am J Nephrol 50:126–132
Lberman-Itskovich S, Elukbi Y, Weinberg Sibony R, Shapiro M, Zelnik Yovel D et al (2022) The epidemiology of multidrug-resistant sepsis among chronic hemodialysis patients. Antibiotics (Basel) 11:1255
Dhingra RK, Young EW, Hulbert-Shearon TE, Leavey SF, Port FK (2001) Type of vascular access and mortality in US hemodialysis patients. Kidney Int 60:1443–1451
Oliver MJ, Rothwell DM, Fung K, Hux JE, Lok CE (2004) Late creation of vascular access for hemodialysis and increased risk of sepsis. J Am Soc Nephrol 15:1936–1942
Shahar S, Mustafar R, Kamaruzaman L, Periyasamy P, Pau KB, Ramli R (2021) Catheter-related bloodstream infections and catheter colonization among haemodialysis patients: prevalence, risk factors, and outcomes. Int J Nephrol 2021:5562690
Murray EC, Marek A, Thomson PC, Coia JE (2015) Gram-negative bacteraemia in haemodialysis. Nephrol Dial Transplant 30(7):1202–1208. https://doi.org/10.1093/ndt/gfv205
Sinclair MR, Souli M, Ruffin F, Park LP, Dagher M, Eichenberger EM et al (2022) Staphylococcus aureus bacteremia among patients receiving maintenance hemodialysis: trends in clinical characteristics and outcomes. Am J Kidney Dis 79:393-403.e1. https://doi.org/10.1053/j.ajkd.2021.06.018
Saran R, Bragg-Gresham JL, Rayner HC, Goodkin DA, Keen ML, Van Dijk PC et al (2003) Nonadherence in hemodialysis: associations with mortality, hospitalization, and practice patterns in the DOPPS. Kidney Int 64:254–262
Allon M (2019) Vascular access for hemodialysis patients: new data should guide decision making. Clin J Am Soc Nephrol 14:954–961
Forauer AR, McNulty NJ, Kaneko TM (2009) Tunneled hemodialysis catheter outcomes in elderly patients. J Vasc Interv Radiol 20:467–471
Lok CE, Allon M, Moist L, Oliver MJ, Shah H, Zimmerman D (2006) Risk equation determining unsuccessful cannulation events and failure to maturation in arteriovenous fistulas (REDUCE FTM I). J Am Soc Nephrol 17:3204–3212
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
The study was approved by SZMC institutional review board (approval number: 0180-22-SZMC).
Informed consent
For this type of retrospective study, no informed consent was required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.

41999_2023_861_MOESM1_ESM.jpg
Supplementary file1 Resistance patterns of bloodstream isolates in the study groups. The overall rate of drug-resistant pathogens was significantly higher among older patients [37/57 (64.9%) versus 41/97 (42.3%), p=0.008]. AmpC beta lactamsaes; ESBL, extended spectrum beta lactamases; MDR, multi-drug resistant; MRSA, methicillin-resistant Staphylococcus aureus; CRAB, carbapenem resistant Acinetobacter baumannii. Three cases of candidemia were excluded (JPG 58 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bnaya, A., Schwartz, Y., Wolfovitz Barchad, O. et al. Clinical presentation and outcome of hemodialysis tunneled catheter-related bloodstream infection in older persons. Eur Geriatr Med 15, 235–242 (2024). https://doi.org/10.1007/s41999-023-00861-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-023-00861-3