Key summary points
To clarify the impact of the severity of worsening renal function during hospitalization on low physical function at discharge in older patients with heart failure and chronic kidney disease.
AbstractSection FindingsIn this retrospective study, severely worsening renal function (grade III) during hospitalization was associated with low physical function at discharge, but moderate-to-mild worsening renal function (grades II or I) showed no such association.
AbstractSection MessageLimiting the severity of worsening renal function (grade III) during hospitalization might positively affect the physical function at discharge of older patients with heart failure and chronic kidney disease.
Abstract
Background
The number of hospitalized older patients with chronic heart failure, chronic kidney disease, and worsening renal function is rising in Japan. This study aimed to clarify the impact of the severity of worsening renal function during hospitalization on low physical function at discharge of these patients.
Methods
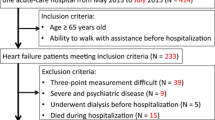
We included 573 consecutive heart failure patients who underwent phase I cardiac rehabilitation. Worsening renal function severity was defined according to elevation during hospitalization of baseline serum creatinine on admission: non-worsening renal function, serum creatinine < 0.2 mg/dL; worsening renal function II/I, serum creatinine ≥ 0.2 to < 0.5 mg/dL; worsening renal function III, and serum creatinine ≥ 0.5 mL/dL. Physical function was measured with the Short Performance Physical Battery. We compared background factors, clinical parameters, pre-hospitalization walking levels, Functional Independence Measure score, and physical function in the three renal function groups. Multiple regression analysis was performed with the Short Performance Physical Battery at discharge as the dependent variable.
Results
The final analysis included 196 patients (mean age 82.7 years, male 51.5%) categorized into three groups based on worsening renal function: worsening renal function grade III group (n = 55), worsening renal function grade II/I group (n = 36), and non-worsening renal function group (n = 105). There is no significant difference in walking levels before hospitalization between the three groups, but physical function at discharge was significantly lower in the worsening renal function III group. Moreover, worsening renal function III was an independent factor for low physical function at discharge.
Conclusion
Worsening of renal function during hospitalization in older patients with heart failure and chronic kidney disease was strongly associated with low physical function at discharge, even after adjusting for other potentially confounding factors, such as pre-hospitalization walking levels, walking start day, and Geriatric Nutrition Risk Index at discharge. Notably, worsening renal function of mild or moderate severity (grade II/I) did not show a significant association with low physical function.


Similar content being viewed by others
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Isobe M (2019) The heart failure “pandemic” in Japan: reconstruction of health care system in the highly aged society. JMAJ 2:103–112. https://doi.org/10.31662/jmaj.2018-0049
Hamaguchi S, Tsuchihashi-Makaya M, Kinugawa S, Yokota T, Ide T, Takeshita A, Tsutsui, JCARE-CARD Investigators (2009) Chronic kidney disease as an independent risk for long-term adverse outcomes in patients hospitalized with heart failure in Japan. Report from the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD). Circ J 73:1442–1447. https://doi.org/10.1253/circj.cj-09-0062
Junho CVC, Trentin-Sonoda M, Panico K, Dos Santos RSN, Abrahao MV, Vernier ICT, Furstenau CR, Carneiro-Ramos, (2022) Cardiorenal syndrome: long road between kidney and heart. Heart Fail Rev 27:2137–2153. https://doi.org/10.1007/s10741-022-10218-w
Weng SC, Chen YC, Hsu CY, Lin CS, Tarng DC, Lin SY (2021) Impacts of heart failure and physical performance on long-term mortality in old patients with chronic kidney disease. Front Cardiovasc Med. 8:680098. https://doi.org/10.3389/fcvm.2021.680098
Saitoh M, Itoh H, Morotomi N, Ozawa T, Ishii N, Uewaki R, Hori K, Shiotani Y, Ando M, Nakashima S, Kawai K, Ohno A, Nagayama M (2014) Impact of chronic kidney disease and anemia on physical function in patients with chronic heart failure. Cardiorenal Med 4:73–81. https://doi.org/10.1159/000362252
Sato E, Mori T, Mishima E, Suzuki A, Sugawara S, Kurasawa N, Saigusa D, Miura D, Morikawa-Ichinose T, Saito R, Oba-Yabana I, Oe Y, Kisu K, Naganuma E, Koizumi K, Mokudai T, Niwano Y, Kudo T, Suzuki C, Takahashi N, Sato H, Abe T, Niwa T, Ito S (2016) Metabolic alterations by indoxyl sulfate in skeletal muscle induce uremic sarcopenia in chronic kidney disease. Sci Rep 6:36618
Damman K, Valenta MAE, Voors AA, O’Connor CM, Veldhuisen DV, Hillege HL (2014) Renal impairment, worsening renal function, and outcome in patients with heart failure: an updated meta-analysis. Eur Heart J 35:455–469. https://doi.org/10.1093/eurheartj/eht386
Palmer J, Friedman H, Waltman Johnson K, Navaratnam P, Gottied SS (2015) Association or persistent and transient worsening renal function with mortality risk, readmissions risk, length of stay, and costs in patients hospitalized with acute heart failure. Clinicoecon Outcomes Res 7:357–367. https://doi.org/10.2147/CEOR.S82267
Okabe T, Yakushiji T, Kido T, Oyama Y, Igawa W, Ono M, Ebara S, Yamashita K, Ymamoto MH, Saito S, Amemiya K, Isoura N, Araki H, Ochiai M (2017) Relationship between worsening renal function and long-term cardiovascular mortality in heart failure patients. Int J Cardiol 230:47–52. https://doi.org/10.1016/j.ijcard.2016.12.101
Maeder MT, Rickli H, Pfistere ME, Muzzarelli S, Amman P, Fehr T, Hack D, Weilenmann D, Dieterle T, Kiencke S, Estlinbaum RHPBL (2012) Incidence, clinical predictors, and prognostic impact of worsening renal function in elderly patients with chronic heart failure on intensive medical therapy. Am Heart J 163:407–414. https://doi.org/10.1016/j.ahj.2011.12.003
Smith GL, Vaccarino V, Kosiborod M, Lichtman JH, Cheng S, Watnic SG, Krumhol HM (2013) Worsening renal function: What is a clinically meaningful change in creatinine during hospitalization with heart failure? J Card Fail 9:26–28. https://doi.org/10.1054/jcaf.2003.3
Praught ML, Shlipak MG (2005) Are small changes in serum creatinine an important risk factor? Curr Opin Nephrol Hypertens 14(3):265–270. https://doi.org/10.1097/01.mnh.0000165894.90748.72
Guralnik JM, Ferrucci L, Simonsick EM, Salive WE, Wallace RB (1995) Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med 332:556–561. https://doi.org/10.1056/NEJM199503023320902
Yokota J, Takahashi R, Matsukawa Y, Matsushima K (2020) Examination of independent predictors of discharge disposition in acute phase hospitalized heart failure patients undergoing phase I cardiac rehabilitation. Eur J Phys Rehabil Med 56:780–786. https://doi.org/10.23736/S1973-9087.20.06347-9
Puthoff ML (2008) Outcome measures in cardiopulmonary physical therapy: short physical performance battery. Cardiopulm Phys Ther J 19:17–22
Kubo I, Izawa KP, Kajisa N, Ryu M, Akasaka H, Ogura A, Kanai M, Matsuzoe H, Matsumoto D (2021) Worsening renal function during hospitalization in elderly patients with heart failure: an independent factor of activities of daily living decline. Heart Vessels 36:76–84. https://doi.org/10.1007/s00380-020-01672-3
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A, Collaborators developing the Japanese equation for estimated GNR (2009) Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 53:982–992. https://doi.org/10.1053/j.ajkd.2008.12.034
Eckardt K-U, Berns JS, Rocco MV, Kashiske BL (2009) Definition and classification of CKD: the debate should be about patient prognosis—a position statement from KDOQI and KDIGO. Am J Kidney Dis 53:915–920. https://doi.org/10.1053/j.ajkd.2009.04.001
Kubo I, Izawa KP, Kajisa N, Ogura A, Kanai M, Nishio R, Matsumoto D (2022) Relationship between physical function at discharge and hospital meal intake in elderly patients with heart failure. Heart Vessels 37:1740–1748. https://doi.org/10.1007/s00380-022-02077-0
Kinugasa Y, Kato M, Sugihara S, Hirai M, Yamada K, Yanagihara K, Yamamoto K (2013) Geriatric nutritional risk index predicts functional dependency and mortality in patients with heart failure with preserved ejection fraction. Circ J 77:705–711. https://doi.org/10.1253/circj.CJ-12-1091
JCS Joint Working Group (2023) Guidelines for treatment of acute heart failure (JCS 2011). Circ J 77:2157–2201. https://doi.org/10.1253/circj.cj-66-0068
Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC (1996) The reliability of the functional independence measure: a quantitative review. Arch Phys Med Rehabil 77:1226–1232. https://doi.org/10.1016/s0003-9993(96)90184-7
Suga H, Ichimura Y, Oda M, Saitoh H (2020) Different correlation between serum levels of indoxyl sulfate and estimated GFR in the elderly with or without dementia. BPB Rep 3(3):102–105. https://doi.org/10.1248/bpbreports.3.3_102
Ichimura Y, Takamatsu H, Ideuchi H, Oda M, Takeda K, Saitoh H (2026) Correlation between plasma levels of anionic uremic toxins and clinical parameters in hemodialysis patients. Yakugaku Zasshi 136(8):1177–1184. https://doi.org/10.1248/yakushi.15-00252
Vanholder R, Schepers E, Pletinck A, Nagler EV, Glorieux G (2014) The uremic toxicity of indoxyl sulfate and p-cresyl sulfate: a systematic review. J Am Soc Nephrol 25:1897–1907. https://doi.org/10.1681/ASN.2013101062
Wu IW, Hsu KH, Lee CC, Sun CY, Hsu HJ, Tsai CJ, Tzen CY, Wang YC, Lin CY, Wu MS (2011) p-Cresyl sulphate and indoxyl sulphate predict progression of chronic kidney disease. Nephrol Dial Transplant 26:938–947. https://doi.org/10.1093/ndt/gfq580
Ito S, Yoshida M (2014) Protein-bound uremic toxins: new culprits of cardiovascular events in chronic kidney disease patients. Toxins (Basel). 6:665–678. https://doi.org/10.3390/toxins6020665
Leong SC, Sirich TL (2016) Indoxyl sulfate–review of toxicity and therapeutic strategies. Toxins (Basel). 8:358. https://doi.org/10.3390/toxins8120358
Enoki Y, Watanabe H, Arake R, Sugimoto R, Imafuku T, Tominaga Y, Ishima Y, Kotani S, Nakajima M, Tanaka M, Matsushita K, Fukagawa M, Otagiri M, Maruyama T (2016) Indoxyl sulfate potentiates skeletal muscle atrophy by inducing the oxidative stress-mediated expression of myostatin and atrogin-1. Sci Rep 6:32084. https://doi.org/10.1038/srep32084
Sato E, Mori T, Mishima E, Suzuki A, Sugawara S, Kurasawa N, Saigusa D, Miura D, Morikawa-Ichinise T, Saito R, Oba-Yabana I, Oe Y, Kisu K, Naganuma E, Koizumi K, Mokudai T, Niwano Y, Kudo T, Suzuki C, Takahashi N, Sato H, Abe T, Niwa T, Ito S (2016) Metabolic alterations by indoxyl sulfate in skeletal muscle induce uremic sarcopenia in kidney disease. Sci Rep 6:36618. https://doi.org/10.1038/srep36618
Wang W, Hao G, Pan Y, Ma S, Yang T, Shi P, Zhu Q, Xie Y, Ma S, Zhang Q, Ruan H, Feng D (2019) Serum indoxyl sulfate is associated with mortality in hospital-acquired acute kidney injury: a prospective cohort study. BMC Nephrol 20:57. https://doi.org/10.1186/s12882-019-1238-9
Tsutsui H, Ide T, Hayashidani S, Suematsu N, Shiomi T, Wen J, Nakamura K, Ichikawa K, Utsumi H, Takeshita A (2001) Enhanced generation of reactive oxygen species in the limb skeletal muscle a murine infract model of heart failure. Circulation 104:134–136. https://doi.org/10.1161/01.cir.104.2.134
Cowie MR, Komajda M, Murray-Thomas T, Underwood J, Ticho B (2026) Prevalence and impact of worsening renal function in patients hospitalized with decompensated heart failure: results of the prospective outcomes study in heart failure (POSH). Eur Heart J 27:1216–1222. https://doi.org/10.1093/eurheartj/ehi859
Sato S, Uno S, Kurita Y, Kim S, OPTION-HF Investigators (2022) Efficacy and safety of intravenous OPC-61815 compared with oral tolvaptan in patients with congestive heart failure. ESC Heart Fail. 9(5):3275–3286. https://doi.org/10.1002/ehf2.14021
Sasaoka T, Seya M, Hatano Y, Tao S, Sasaki T, Yoshikawa S, Majima Y, Kawabata M, Masahiko G, Ashikaga T, Hirao K, Isobe M (2014) Low dose carperitide (alpha-hANP) administration is effective for preventing worsening renal function (WRF) and long-term renal protection. J Card Fail 20(8):S96. https://doi.org/10.1016/j.cardfail.2014.06.270
van der Aart-van-der-Beek AB, de Boer RA, Heerspink HJL (2022) Kidney and heart failure outcomes associated with SGLT2 inhibitor use. Nat Rev Nephrol 18(5):294–306. https://doi.org/10.1038/s41581-022-00535-6
Kitzman DW, Whellan DJ, Duncan P, Pastva AM, Mentz R, Reeves GR, Nelson MB, Chen H, Upadhya B, Reed SD, Espeland MA, Hewston L (2021) Physical rehabilitation for older patients hospitalized for heart failure. N Engl J Med 385:203–216. https://doi.org/10.1056/NEJMoa2026141
Takara Y, Saitoh M, Morisawa T, Takahashi T, Yoshida N, Sakiyama M, Nakamura R, Tei I, Fujiwara T (2021) Clinical characteristics of older heart failure patients with hospital-acquired disability: a preliminary, single-center, observational study. Cardiol Res 12:293–301. https://doi.org/10.14740/cr1306
Kitamura M, Izawa PK, Taniue H, Miura Y, Imamura K, Nagashima H, Brubaker PH (2017) Relationship between activities of daily living and readmission within 90 days in hospitalized elderly patients with heart failure. Biomed Res Int 7420738:7. https://doi.org/10.1155/2017/7420738
Yamamoto H, Iwawaki T, Murota M, Yamamoto H, Iwawaki Y, Muroto M (2021) Literature of nursing to prevent readmission of patients with chronic heart failure. Bull School Nurs Kyoto Prefect Univ Med 31:1–14
Acknowledgements
The authors would like to thank all of the participating patients in Yodogawa Christian Hospital.
Funding
This work was supported by a grant from JSPS KAKENHI (No. JP22K11392). Neither the authors nor their associated institutions report any financial relationships with industry relevant to this study.
Author information
Authors and Affiliations
Contributions
Conceptualization IK and KPI. Formal analysis IK. Investigation IK, NK, HN, and KK. Data curation IK. Writing—original draft preparation IK, AO, MK, and AM. Writing—review and editing KPI, RN, and DM. Supervision KPI. Project administration KPI and DM. Funding acquisition KPI. All authors approved the manuscript for submission.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflicts of interest in relation to the work reported in this manuscript.
Ethical approval
All procedures performed in studies involving human and participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kubo, I., Izawa, K.P., Kajisa, N. et al. Association between worsening renal function severity during hospitalization and low physical function at discharge: a retrospective cohort study of older patients with heart failure and chronic kidney disease from Japan. Eur Geriatr Med 14, 869–878 (2023). https://doi.org/10.1007/s41999-023-00809-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-023-00809-7