Key Summary Points
To measure the effects of home exercises complemented with supervision on fall-related variables in older people.
AbstractSection FindingsSupervised home exercise seems superior only on functional mobility (TUGT).
AbstractSection MessageOlder individuals who do not have exercise habits should be motivated to exercise training in daily life.
Abstract
Purpose
The aim was to measure the effects of the home exercises supported with supervision on the fall-related variables in older people.
Methods
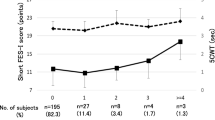
Seventy-five individuals over the age of 65 were enrolled. They were allocated to a “minimally supervised home exercise group” (group 1) or a “home exercise group” (group 2). Falls efficacy, fear of falling (FOF), fall risk, functional mobility, balance performance, and depression were assessed using the Falls Efficacy Scale International (FES-I), visual analog scale (VAS-FOF), the Elderly Falls Screening Test (EFST), the Timed Up and Go Test (TUGT), Tinetti’s Balance Performance Oriented Mobility Assessment (BPOMA), and the Geriatric Depression Scale Short Form (GDS-SF), respectively. Participants performed a four-day weekly exercise program for eight weeks. Group 1 was supervised one day per week on a group basis.
Results
Results are based on 75 subjects (group 1 n = 37, group 2 n = 38). Analysis of variance revealed significant interactions only for FES-I, VAS-FOF, TUGT, and BPOMA. The difference between groups was significant only for TUGT score; group 1 had better scores at 8 weeks and 6 months. FES-I, VAS-FOF, and BPOMA were significantly improved in both groups. EFST and GDS improved in the total sample but not at the group level.
Conclusion
Supervised home exercise seems to be superior only for functional mobility (TUGT). Further studies with a larger sample are needed to draw conclusions about depression and fall risk. The intervention was feasible and atendible.
Trial registration
ClinicalTrials.gov" NCT05337839. Retrospectively registered.

Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable requests.
References
Lacroix A, Kressig RW, Muehlbauer T, Gschwind YJ, Pfenninger B et al (2016) Effects of a supervised versus an unsupervised combined balance and strength training program on balance and muscle power in healthy older adults: a randomized controlled trial. Gerontology 62(3):275–288. https://doi.org/10.1159/000442087
Rubenstein LZ (2006) Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing 35(Suppl 2):ii37–ii41. https://doi.org/10.1093/ageing/afl084
Rapp K, Freiberger E, Todd C, Klenk J, Becker C et al (2014) Fall incidence in Germany: results of two population-based studies, and comparison of retrospective and prospective falls data collection methods. BMC Geriatr 14:105. https://doi.org/10.1186/1471-2318-14-105
Halil M, Ulger Z, Cankurtaran M, Shorbagi A, Yavuz BB et al (2006) Falls and the elderly: is there any difference in the developing world? A cross-sectional study from Turkey. Arch Gerontol Geriatr 43(3):351–359. https://doi.org/10.1016/j.archger.2005.12.005
Bjerk M, Brovold T, Skelton DA, Bergland A (2017) A falls prevention program to improve quality of life, physical function and falls efficacy in older people receiving home help services: study protocol for a randomised controlled trial. BMC Health Serv Res 17:559. https://doi.org/10.1186/s12913-017-2516-5
Gschwind YJ, Kressig RW, Lacroix A, Muehlbauer T, Pfenninger B et al (2013) A best practice fall prevention exercise program to improve balance, strength / power, and psychosocial health in older adults: study protocol for a randomized controlled trial. BMC Geriatr 13:105. https://doi.org/10.1186/1471-2318-13-105
Stel VS, Smit JH, Pluijm SM, Lips P (2003) Balance and mobility performance as treatable risk factors for recurrent falling in older persons. J Clin Epidemiol 56(7):659–668. https://doi.org/10.1016/s0895-4356(03)00082-9
Howe TE, Rochester L, Jackson A, Banks PMH, Blair VA (2000) Exercise for improving balance in older people. Cochrane Database of System Rev. https://doi.org/10.1002/14651858.CD004963.pub2
Laybourne AH, Biggs S, Martin FC (2008) Falls exercise interventions and reduced falls rate: Always in the patient’s interest? Age Ageing 37(1):10–13. https://doi.org/10.1093/ageing/afm190
Lamb SE, Jørstad-Stein EC, Hauer K, Becker C (2005) Prevention of Falls Network Europe and Outcomes Consensus Group. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc. 53(9):1618–22. https://doi.org/10.1111/j.1532-5415.2005.53455.x
Vellas BJ, Wayne SJ, Romero LJ, Baumgartner RN, Garry PJ (1997) Fear of fall and restriction of mobility in elderly fallers. Age Ageing 26(3):189–193. https://doi.org/10.1093/ageing/26.3.189
Jung D, Lee J, Lee SMA (2009) meta-analysis of fear of falling treatment programs for the elderly. West J Nurs Res 31(1):6–16. https://doi.org/10.1177/0193945908320466
Scheffer AC, Schuurmans MJ, van Dijk N, van der Hooft T, de Rooij SE (2008) Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing 37(1):19–24. https://doi.org/10.1093/ageing/afm169
Cumming RG, Salkeld G, Thomas M, Szonyi G (2000) Prospective study of the impact of fear of falling on activities of daily living, SF-36 scores, and nursing home admission. J Gerontol Med Sci 55(5):M299-305. https://doi.org/10.1093/gerona/55.5.m299
Tinetti ME, Mendes de Leon CF, Doucette JT, Baker DI (1994) Fear of falling and fall-related efficacy in relationship to functioning among community-living elders. J Gerontol Med Sci 49(3): M140–7. https://doi.org/10.1093/geronj/49.3.m140
Schoenfelder DP, Rubenstein LM (2004) An exercise program to improve fall-related outcomes in elderly nursing home residents. Appl Nurs Res 17(1):21–31. https://doi.org/10.1016/j.apnr.2003.10.008
Thiamwong L, Suwanno J (2014) Effects of simple balance training on balance performance and fear of falling in rural older adults. Int J Gerontol 8(3):143–146. https://doi.org/10.1016/j.ijge.2013.08.011
Nelson ME, Layne JE, Bernstein MJ, Nuernberger A, Castaneda C et al (2004) The effects of multidimensional home-based exercise on functional performance in elderly people. J Gerontol A Biol Sci Med Sci 59(2):154–160. https://doi.org/10.1093/gerona/59.2.m154
Ng CACM, Fairhall N, Wallbank G et al (2019) Exercise for falls prevention in community-dwelling older adults: trial and participant characteristics, interventions and bias in clinical trials from a systematic review. BMJ Open Sport Exerc Med 5:e000663. https://doi.org/10.1136/bmjsem-2019-000663
Sjösten N, Vaapio S, Kivelä SL (2008) The effects of fall prevention trials on depressive symptoms and fear of falling among the aged: a systematic review. Aging Ment Health 12(1):30–46. https://doi.org/10.1080/13607860701366079
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3):189–198. https://doi.org/10.1016/0022-3956(75)90026-6
Tombaugh TN, McIntyre NJ (1992) The mini-mental state examination: a comprehensive review. J Am Geriatr Soc 40(9):922–935. https://doi.org/10.1111/j.1532-5415.1992.tb01992.x
Pollock ML, Gaesser GA, Butcher JD, Despres J-P, Dishman RK, Franklin B, Ewing Garber C (1998) American College of Sports Medicine Position Stand. The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc. 30(6):975–991. https://doi.org/10.1097/00005768-199806000-00032
Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C et al (2005) Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age Ageing 34(6):614–619. https://doi.org/10.1093/ageing/afi196
Alice C Scheffer, Marieke J Schuurmans, Nynke vanDijk, Truus van der Hooft, Sophia E de Rooij (2010) Reliability and validity of the visual analogue scale for fear of falling in older persons. J Am Geriatr Soc 58(11):2228–30. https://doi.org/10.1111/j.1532-5415.2010.03105.x.
Podsiadlo D, Richardson S (1991) The Timed “Up&Go”: A test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39(2):142–148. https://doi.org/10.1111/j.1532-5415.1991.tb01616.x
Tinetti ME (1986) Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc 34(2):119–126. https://doi.org/10.1111/j.1532-5415.1986.tb05480.x
Cwikel JG, Fried AV, Biderman A, Galinsky D (1998) Validation of a fall-risk screening test, the Elderly Fall Screening Test (EFST), for community-dwelling elderly. Disabil Rehabil 20(5):161–167. https://doi.org/10.3109/09638289809166077
Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, et al (1982-1983) Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 17(1):37–49. https://doi.org/10.1016/0022-3956(82)90033-4.
Halvarsson A, Franzén E, Ståhle A (2013) Assessing the relative and absolute reliability of the Falls Efficacy Scale-International questionnaire in elderly individuals with increased fall risk and the questionnaire’s convergent validity in elderly women with osteoporosis. Osteoporos Int 24(6):1853–1858. https://doi.org/10.1007/s00198-012-2197-1
Ulus Y, Durmus D, Akyol Y et al (2012) Reliability and validity of the Turkish version of the Falls Efficacy Scale International (FES-I) in community-dwelling older persons. Arch Gerontol Geriatr 54:429–433
Girden ER (1992) ANOVA: repeated measures. Newbury Park: CA: Sage Publications. https://doi.org/10.4135/9781412983419
Cohen J (1988) Statistical Power Analysis for the Behavioral Sciences, 2nd edn. Lawrence Erlbaum Associates, Publishers, Hillsdale, NJ
Kumar A, Delbaere K, Zijlstra GA, Carpenter H, Iliffe S et al (2016) Exercise for reducing fear of falling in older people living in the community: Cochrane systematic review and meta-analysis. Age Ageing 45:345–352. https://doi.org/10.1093/ageing/afw036
Schott N, Tietjens M (2019) Exploring the mediating role of social support and fall efficacy on the association of falls on physical activity: A cross-sectional study in an assisted-living population. J Aging Phys Act 27(1):53–60. https://doi.org/10.1123/japa.2017-0378
Brouwer BJ, Walker C, Rydahl SJ, Culham EG (2003) Reducing fear of falling in seniors through education and activity programs: a randomized trial. J Am Geriatr Soc 51(6):829–834. https://doi.org/10.1046/j.1365-2389.2003.51265.x
Youssef EF, Shanb AA (2016) Supervised versus home exercise training programs on functional balance in older subjects. Malays J Med Sci 23(6):83–93. https://doi.org/10.21315/mjms2016.23.6.9
King LA, Wilhelm J, Chen Y, Blehm R, Nutt J, Chen Z, Serdar A (2015) Does group, individual or home exercise best improve mobility for people with Parkinson’s disease? J Neurol Phys Ther. 39(4):204–212. https://doi.org/10.1097/NPT.0000000000000101
Feng C, Adebero T, DePaul VG, Vafaei A, Norman KE, Auais M (2022) A systematic review and meta-analysis of exercise interventions and use of exercise principles to reduce fear of falling in community-dwelling older adults. Phys Ther 102(1):236
Weber M, Belala N, Clemson L, Boulton E, Hawley-Hague H, Becker C, Schwenk M (2018) Feasibility and effectiveness of intervention programmes integrating functional exercise into daily life of older adults: a systematic review. Gerontology 64(2):172–187. https://doi.org/10.1159/000479965
Hróbjartsson A, Gøtzsche PC (2001) Is the placebo powerless? N Engl J Med 344(21):1594–1602. https://doi.org/10.1056/nejm200105243442106
Acknowledgements
There is no acknowledgment.
Funding
No funding was received for conducting this study. The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by Ayca Avci Trakyali, Taciser Kaya, and Bugra Ince. Statistical analysis were performed by Bugra Ince. The manuscript was written by Taciser Kaya and Bugra Ince, and all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval and informed consent
This study was performed in accordance with the ethical standards as laid down in the Declaration of Helsinki. Approval was granted by the Ethics Committee of Izmir Bozyaka Training and Research Hospital (Date: 17 Nov, 2011, Meeting no: 02, Decision No: 03). This study was approved by the local ethics committee of our hospital. All the participants gave signed written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Avci Trakyali, A., Kaya, T. & Ince, B. Effects of an exercise program combining unsupervised home exercises and supervised group-based exercises on fall-related variables in older adults: a randomized controlled trial. Eur Geriatr Med 14, 59–67 (2023). https://doi.org/10.1007/s41999-022-00724-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-022-00724-3