Key summary points
To derive and validate a 90-day unplanned hospital readmission (UHR) score based on information readily available to non-hospital based care providers.
AbstractSection FindingsIndependent risk factors for 90-day UHR were: use of mobility aids, presence of dementia syndrome, history of recent hospitalisation, and discharge to domiciliary home. In the development cohort and in the validation cohort, the 90-day UHR rate increased significantly across risk groups.
AbstractSection MessageThe findings should enable targeted multidisciplinary interventions in order to limit UHR.
Abstract
Purpose
To derive and validate a 90-day unplanned hospital readmission (UHR) score based on information available to non-hospital based care providers.
Methods
Retrospective longitudinal study with cross-validation method. Participants were older adults (≥ 65 years) admitted to a geriatric short-stay department in a general hospital in France. Patients were split into a derivation cohort and a validation cohort. We recorded demographic information, medical history, and concurrent clinical characteristics. The main outcome was 90-day UHR. Data obtained from hospital discharge letters were used in a logistic regression model to construct a predictive score, and to identify risk groups for 90-day UHR.
Results
In total, 750 and 250 aged adults were included in both the derivation and the validation cohorts. Mean age was 87.2 ± 5.2 years, most were women (68.1%). Independent risk factors for 90-day UHR were: use of mobility aids (p = .02), presence of dementia syndrome (p = .02), history of recent hospitalisation (p = .03), and discharge to domiciliary home (p = .005). From these four risk factors, three groups were determined: low-risk group (score < 4), medium-risk group (score between 4 and 6), and high-risk group (score ≥ 6). In the derivation cohort the 90-day UHR rates increased significantly across risk groups (14%, 22%, and 30%, respectively). The 90-day UHR score had the same discriminant power in the derivation cohort (c-statistic = 0.63) as in the validation cohort (c-statistic = 0.63).
Conclusions
This score makes it possible to identify aged adults at risk of 90-day UHR and to target multidisciplinary interventions to limit UHR for patients discharged from a Geriatric Short-Stay Unit.
Similar content being viewed by others
Introduction
Unplanned hospital readmission (UHR) is frequent [1]. Risk factors for UHR vary according to the population studied or the time of re-admission considered [2]. In the population aged 65 years and over, the most frequent factors associated with UHR after a hospitalisation in medical or surgical ward are race/ethnicity [3, 4], socio-economic status [3, 5, 6], marital status [4, 6], old age [2, 7, 8], admission in the previous 2 years [7], male sex [9, 10], presence of comorbidity [11], and history of neurological disorder [12]. Meta-analysis failed to identify the most important associated factors except for age [2]. Older people seem to be re-admitted particularly often [1], and some of these UHR appear to be avoidable [13]. Limiting avoidable UHR is a major public health issue [14], since UHR are a significant cause of healthcare costs [10, 14,15,16], and are associated with poor outcomes [8, 14]. Some countries have experimented programs to reduce UHR based on collaboration between hospital-based and community care [17, 18]. The first step is to identify people at risk for UHR. General practitioners (GPs) are key players in identifying older people at risk of readmission. However, to do this, they need a simple and easy-to-use tool based on quickly accessible information. The aim of this study was to derive and validate a 90-day unplanned hospital readmission score based on information readily available to GPs.
Methods
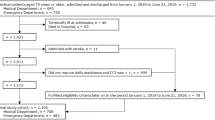
Study design and population
This was a retrospective cohort study, including patients aged 65 years or older, admitted to the geriatric short-stay department of the Hospital of Valenciennes (France), from 1 January to 31 December 2019. The geriatric short-stay services in France welcome polypathological aged patients at high risk of loss of functional autonomy (presence of frailty criteria, presence of cognitive disorders…). Patients are assessed and cared for by a multidisciplinary team trained in geriatrics, and benefit from an individualized medical and social evaluation, as well as a psychological and motor assessment. Rehabilitation sessions are set up according to the patient's needs. The average length of stay is about 10 days. Patients who died during their hospital stay, and those who were readmitted on a scheduled basis, were excluded from the study.
The cohort was randomly divided into two samples: 75% of the population served to derive the prediction model (derivation cohort), and 25% were used to validate it (validation cohort).
Variables studied
The following demographic characteristics were collected from the hospital discharge letter: age, sex, place of residence, living alone or not, children (yes/no), and presence of a caregiver. Concurrent clinical characteristics were noted, and included cognitive status (dementia, delirium), physical status (walking difficulties, dependence for activities of daily living), nutritional status, comorbidities, and polypharmacy (≥ 5 drugs/day). The aids used were recorded (home care nursing service, life assistant, mobility aids). The history of hospitalisation in the three months preceding the index hospitalisation, as well as the destination at discharge from hospital were also noted (domiciliary home, sheltered living, or nursing home).
Ethics aspects
The study was performed in accordance of the Declaration of Helsinki and French law relating to biomedical research involving human subjects. It was approved by the ethics committee of the General Hospital of Valenciennes (under the number 2021/001).
Statistical analyses
The main outcome was 90-day UHR. It was defined as the first episode of unplanned readmission occurring within the 90 days following hospital discharge.
Descriptive analysis of patients’ characteristics was performed. Quantitative variables are described as mean ± standard deviation (m ± SD), and categorical variables as number and percentage (n, %). Bivariable relationships between each risk factor and 90-day unplanned hospital readmission in the derivation cohort were assessed using logistic regression. For multivariable analysis, a logistic regression model was built using stepwise selection. Results are presented as odds ratios (OR) and 95% Confidence Interval (CI).
A 90-Day UHR score was constructed. Point values were assigned to each risk factor according to the odds ratio in the final model. The point values were equal to the corresponding odds ratios, rounded to the nearest integer. According to number of risk factors present for each patient, three risk groups were defined.
Bootstrap analysis was performed to calculate the c-statistic (representing the area under the Receiver Operating Characteristic (ROC) curves) to assess the accuracy of the UHR score. Replication on 500 different samples drawn with replacement was performed using the bootstrap method.
Statistical analyses were performed using SAS software release 9.4, (SAS Institute, Inc., Cary, NC). Tests were considered as significant for p-values less than 0.05.
Results
In total, 1000 patients were included (750 in the derivation cohort, and 250 in the validation cohort). Over two-thirds were women (68.1%), and mean age was 87.2 ± 5.2 years (87.5 ± 4.9 years in the derivation cohort, vs 87.1 ± 5.3 years in the validation cohort). Other characteristics for the derivation and validation cohorts are described in Table 1.
The independent predictive factors for 90-day UHR identified in the derivation cohort were (Table 2): use of mobility aids (p = 0.02), presence of a dementia syndrome (p = 0.02), history of hospitalisation within the preceding three months (p = 0.03), and the fact of being discharged to domiciliary home or sheltered living (p = 0.005). None of the reasons of hospitalisation taken was significantly associated to 90-day UHR.
Point values were determined for each of the four risk factors, and summed for each patient (Table 3). Three risk groups were determined according to number of risk factors: low-risk group (0 or 1 risk factor), medium-risk group (2 risk factors), and high-risk group (3 or 4 risk factors).
In the derivation cohort, the 90-day UHR rate increased significantly (p = 0.0003) across risk groups. Similar results were observed in the validation cohort (p = 0.03). The 90-day UHR score had the same discriminant power in the derivation cohort (c-statistic = 0.63) as in the validation cohort (c-statistic = 0.63).
Discussion
In our study, 90-day UHR occurred in 23% of cases, which is in line with rates described in the literature for the aged population [1]. The factors significantly associated with 90-day UHR were: presence of dementia syndrome, use of mobility aids, hospitalisation within the preceding three months, and being discharged to domiciliary home. Dementia or a history of neurological disorders has previously been reported by other authors as being associated with early or late UHR after surgery [8, 13, 15, 19]. Some studies have suggested that patients with dementia have an increased rate of frailty and urgent hospitalization [20,21,22]. It is possible that patients with cognitive or neurological disorders are more likely to decompensate for a chronic condition or represent an acute condition following an initial acute event. Several authors have observed that two or more admissions during the previous year was associated with 6-month UHR [7, 23]. In our study, hospitalisation within the preceding three months was found to be a significant risk factor for UHR. This observation could reflect the absence of intervention to correct the risk of readmission, and the difficulty in identifying patients at risk. Heins et al. showed that patients with multiple comorbidities, and with high care needs, do not necessarily have the same profile as patients who tend to have UHR [24]. There is thus a compelling need to develop tools to help screen for aged patients who are at high risk of UHR, with a view to implementing concrete preventive actions. “Several scores exist in the literature [25,26,27]. Their discriminating performances are poor [25]. Some authors suggest that frailty scores could be used to identify older subjects at risk for re-hospitalisation [28]. General practitioners need a rapid screening tool that allows them to schedule specific management for at-risk patients based on available resources”. In their systematic review of interventions aimed at preventing UHR, Coffey et al. showed that the successful interventions pre- and post-discharge for preventing UHR were those leveraging integrated systems between hospital-based and community care, with multidisciplinary service provision, individualization of services, and specialist follow-up [18]. Identifying patients at risk of UHR before, or at the time of discharge from hospital therefore seems essential to initiating appropriates services in a timely manner to help avoid future re-admissions in this population. In our study, we found that being discharged to domiciliary home was associated with a higher risk of UHR. This seems logical, since people discharged to a rehabilitation centre or nursing home are closely monitored and medically supervised, thus limiting the risk of UHR. UHR is increasingly being used as an indicator of the quality of care [29]. However, it would be wrong to consider all UHR as avoidable. In a study of post-surgical readmissions, Jencks et al. observed that 70.5% of patients readmitted within 30 days after surgical discharge were rehospitalized for a medical condition [16]. However, the authors surmised that some of these readmissions could likely be replaced by outpatient care or scheduled hospitalisation [16]. Indeed, UHRs are longer [16], more costly [16], and associated with poor outcome [8, 14]. Graves et al. showed that a comprehensive intervention among older adults (> 65 years) with at least one risk factor for readmission was cost-effective, and improved health outcomes (quality-adjusted life years) [30]. There is evidence that interventions of this type are beneficial, suggesting that they should be promoted and implemented. Mathew et al. performed a systematic review and meta-analysis of factors associated with readmissions in older adults following fragility fractures [2]. Age was the only factor for which pooling of data across studies was possible, and age was shown to be significantly associated with re-presentation to the emergency department both within 30 days (OR 1.27; 95% CI 1.14–1.43) and beyond 30 days (OR 1.23; 95% CI 1.01–1.50) [2]. In our study, advanced age was not associated with an increased risk of UHR. However, the population of our study was composed solely of patients initially admitted to a short-stay unit for medical reasons. The clinical profile of the patients was therefore likely different, with a higher mean age and a higher level of frailty in our population.
Our work has several strengths. Most studies focus on readmissions after surgical discharge. This is the first score to predict 90-day UHR in a population aged 65 years or more, and the score was successfully crossed-validated in a validation cohort. Its accuracy is similar to those developed by other authors [1]. The score uses information that is easy to collect from the hospital discharge letter. This makes it relevant and helpful for GPs, but also useful for other front-line practitioners outside the hospital setting. The identification of older persons at high risk of rehospitalisation would make it possible to implement targeted interventions to reduce the risk. Our study also has some limitations. All the patients included were initially admitted to a geriatric short-stay unit, and therefore, the study population comprises patients who are frail, polymedicated, with low autonomy. Nevertheless, comorbidities, autonomy and polypharmacy were not found to be associated with the risk of UHR. Second, the data required to calculate the UHR score are given in the hospital discharge report. In France, geriatrics units systematically perform multidimensional, comprehensive geriatric assessment, and specifically report, for example, the presence of cognitive disorders or walking aids. This information may therefore be absent from discharge reports issued by other hospital wards. Nevertheless, the score components remain simple to collect by asking the patient or entourage if not mentioned in the hospital communication. This score was constructed on the basis of data from before the COVID-19 epidemic. Therefore, we cannot generalize its metrological properties in an epidemic situation.
In summary, we developed and validated a score to identify older adults at high risk of 90-day UHR after a stay in a short-stay geriatrics ward for medical reasons. Identifying patients at risk of UHR should help to guide the selection and implementation of comprehensive multidisciplinary and individualized services to limit UHR and improve quality of life in these older adults.
References
Kansagara D, Englander H, Salanitro A, Kagen D, Theobald C, Freeman M et al (2011) Risk prediction models for hospital readmission: a systematic review. JAMA 306:1688–1698. https://doi.org/10.1001/jama.2011.1515
Mathew SA, Gane E, Heesch KC, McPhail SM (2016) Risk factors for hospital re-presentation among older adults following fragility fractures: a systematic review and meta-analysis. BMC Med 14:136. https://doi.org/10.1186/s12916-016-0671-x
Damiani G, Salvatori E, Silvestrini G, Ivanova I, Bojovic L, Iodice L et al (2015) Influence of socioeconomic factors on hospital readmissions for heart failure and acute myocardial infarction in patients 65 years and older: evidence from a systematic review. Clin Interv Aging 2015(10):237–245. https://doi.org/10.2147/CIA.S71165.eCollection
Howie-Esquivel J, Spicer JG (2012) Association of partner status and disposition with rehospitalization in heart failure patients. Am J Crit care 21:e65-73. https://doi.org/10.4037/ajcc2012382
Schwarz KA, Elman CS (2003) Identification of factors predictive of hospital readmissions for patients with heart failure. Heart Lung 32:88–99. https://doi.org/10.1067/mhl.2003.15
Roe-Prior P (2007) Sociodemographic variables predicting poor post-discharge outcomes for hospitalized elders with heart failure. Medsurg Nurs 16:317–321
Lopez-Aguila S, Contel JC, Farre J, Campuzano JL, Rajmil L (2011) Predictive model for emergency hospital admission and 6-month readmission. Am J Manag Care 17:e348–e357
Khan MA, Hossain FS, Dashti Z, Muthukumar N (2012) Causes and predictors of early re-admission after surgery for a fracture of the hip. J Bone Joint Surg Br 94:690–697. https://doi.org/10.1302/0301-620X.94B5.28933
Basques BA, Bohl DD, Golinvaux NS, Leslie MP, Baumgaertner MR, Grauer JN (2015) Postoperative length of stay and 30-day readmission after geriatric hip fracture: an analysis of 8434 patients. J Orthop Trauma 29:e115–e120. https://doi.org/10.1097/BOT.0000000000000222
Robinson T, Kerse N (2012) Medical readmissions amongst older New Zealanders: a descriptive analysis. N Z Med J 125:24–34
Harstedt M, Rogmark C, Sutton R, Melander O, Fedorowski A (2015) Impact of comorbidity on 6-month hospital readmission and mortality after hip fracture surgery. Injury 46:713–718. https://doi.org/10.1016/j.injury.2014.12.024
Akugizibwe R, Calderon-Larranaga A, Roso-Llorach A et al (2020) Multimorbidity patterns and unplanned hospitalisation in a cohort of older adults. J Clin Med. https://doi.org/10.3390/jcm9124001
Kates SL, Behrend C, Mendelson DA, Cram P, Friedman SM (2015) Hospital readmission after hip fracture. Arch Orthop Trauma Surg 135:329–337. https://doi.org/10.1007/s00402-014-2141-2
Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM (2016) Readmissions, observation, and the hospital readmissions reduction program. New Engl J Med 374:1543–1551. https://doi.org/10.1056/NEJMsa1513024
Kates SL, Shields E, Behrend C, Noyes KK (2015) Financial implications of hospital readmission after hip fracture. Geriatr Orthop Surg Rehabil 6:140–146. https://doi.org/10.1177/2151458515578265
Jencks SF, Williams MV, Coleman EA (2009) Rehospitalizations among patients in the Medicare fee-for-service program. New Engl J Med 360:1418–1428. https://doi.org/10.1056/NEJMsa0803563
Morkisch N, Upegui-Arango LD, Cardona MI, van den Heuvel D, Rimmele M, Sieber CC et al (2020) Components of the transitional care model (TCM) to reduce readmission in geriatric patients: a systematic review. BMC Geriatr 20:345. https://doi.org/10.1186/s12877-020-01747-w
Coffey A, Leahy-Warren P, Savage E, Hegarty J, Cornally N, Day MR et al (2019) Interventions to promote early discharge and avoid inappropriate hospital (Re)admission: a systematic review. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph16142457
Teixeira A, Trinquart L, Raphael M, Bastianic T, Chatellier G, Holstein J (2009) Outcomes in older patients after surgical treatment for hip fracture: a new approach to characterise the link between readmissions and the surgical stay. Age Ageing 38:584–589. https://doi.org/10.1093/ageing/afp124
Waite SJ, Maitland S, Thomas A, Yarnall AJ (2021) Sarcopenia and frailty in individuals with dementia: a systematic review. Arch Gerontol Geriatr 92:104268. https://doi.org/10.1016/j.archger.2020.104268
Maxwell CJ, Mondor L, Hogan DB et al (2019) Joint impact of dementia and frailty on healthcare utilisation and outcomes: a retrospective cohort study of long-stay home care recipients. BMJ Open 9:e029523. https://doi.org/10.1136/bmjopen-2019-029523
Grande G, Haaksma ML, Rizzuto D et al (2019) Co-occurrence of cognitive impairment and physical frailty, and incidence of dementia: systematic review and meta-analysis. Neurosci Biobehav Rev 107:96–103. https://doi.org/10.1016/j.neubiorev.2019.09.001
Donze J, Aujesky D, Williams D, Schnipper JL (2013) Potentially avoidable 30-day hospital readmissions in medical patients: derivation and validation of a prediction model. JAMA Intern Med 173:632–638. https://doi.org/10.1001/jamainternmed.2013.3023
Heins M, Korevaar J, Schellevis F, Rijken M (2020) Identifying multimorbid patients with high care needs: a study based on electronic medical record data. Eur J Gen Pract 26:189–195. https://doi.org/10.1080/13814788.2020.1854719
Schwab C, Le Moigne A, Fernandez C, Durieux P, Sabatier B, Korb-Savoldelli V (2018) External validation of the 80+ score and comparison with three clinical scores identifying patients at least 75 years old at risk of unplanned readmission within 30 days after discharge. Swiss Med Wkly 148:w14624
Schwab C, Hindlet P, Sabatier B, Fernandez C, Korb-Savoldelli V (2019) Risk scores identifying elderly inpatients at risk of 30-day unplanned readmission and accident and emergency department visit: a systematic review. BMJ Open 9(7):e028302
van Walraven C, Dhalla IA, Bell C, Etchells E, Stiell IG, Zarnke K et al (2010) Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. Can Med Assoc J 182(6):551–557
Hansen TK, Shahla S, Damsgaard EM, Bossen SRL, Bruun JM, Gregersen M (2021) Mortality and readmission risk can be predicted by the record-based multidimensional prognostic index: a cohort study of medical inpatients older than 75 years. Eur Geriatr Med 12(2):253–261
van Walraven C, Bennett C, Jennings A, Austin PC, Forster AJ (2011) Proportion of hospital readmissions deemed avoidable: a systematic review. Can Med Assoc J 183:E391-402. https://doi.org/10.1503/cmaj.101860
Graves N, Courtney M, Edwards H, Chang A, Parker A, Finlayson K (2009) Cost-effectiveness of an intervention to reduce emergency re-admissions to hospital among older patients. PLoS ONE 4:e7455. https://doi.org/10.1371/journal.pone.0007135
Acknowledgements
The authors thank Fiona Ecarnot for editorial assistance, and Emmanuel Fauck administrative assistance.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by LG, and MD. The first draft of the manuscript was written by LG, and MD, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interest directly or indirectly related to this work.
Ethical approval
The study was performed in accordance with the Declaration of Helsinki and current French legislation relating to biomedical research involving human subjects. It was approved by the ethics committee of the General Hospital of Valenciennes (under the number 2021/001).
Informed consent
No participant objected to participate to the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dramé, M., Hombert, V., Cantegrit, E. et al. Derivation and validation of a 90-day unplanned hospital readmission score in older patients discharged form a geriatric ward. Eur Geriatr Med 13, 1119–1125 (2022). https://doi.org/10.1007/s41999-022-00687-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-022-00687-5